Introduction: Major depressive disorder (MDD) often goes unrecognized in cancer patients. Some symptoms of major depression mimic signs and symptoms of malignancy due to which it often remains under-diagnosed. Depression has a contributing role in increasing the morbidity of cancer patients which if diagnosed and managed early in the treatment course can have a positive impact on cancer patients. This study focuses on determining the prevalence of major depression among cancer patients admitted in a tertiary care hospital in Lahore, Pakistan.
Place & Duration: Mayo Hospital, Lahore. (March 01-30, 2019).
Methods: After project approval and consent, a total of 187 patients were recruited in the study. Selection was made based on predefined criteria. Patients ranging between age group of 14-80 years in Mayo Hospital Lahore, Pakistan were included. Interviews were conducted through a pretested questionnaire based on DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) criteria. Data was analyzed with Stata version 13. Patients were considered to be having major depressive disorder if they fulfill DSM-5 criteria for MDD; they must have 5 or more out of following 9 symptoms for ≥2 weeks: low mood, sleep disturbance (insomnia/hypersomnia), loss of interest in daily activities (anhedonia), feelings of guilt, low energy, loss of concentration, appetite changes (increased or decreased), psychomotor agitation/retardation and suicidal ideation. Symptoms should cause significant distress or impairment in social, occupational or other important areas of normal functioning and should not be attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition. The disturbance is not better explained by persistent psychiatric or psychotic disorders like schizophrenia, schizoaffective disorder, delusional disorder or other specified or unspecified schizophrenia spectrum and other psychotic disorders. Patients should not be currently on anti-depressants for any reason.
Objectives: To determine the prevalence of major depression among cancer patients.
Design: Cross-sectional study.
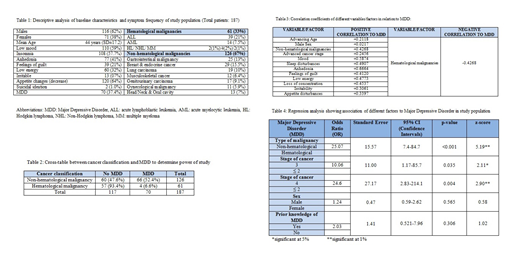
Results: Out of 187 patients (171 in-patient, 16 outpatient), 116 (62%) were males and 71 (38%) were females with mean age of 44 years (SD±17.2). Descriptive analysis shows that 61 (33%) had hematological and 126 (67%) patients had non-hematological malignancies. 110 (59%) patients had low mood, 108 (57.7%) had insomnia, 77 (41%) lost interest in daily activities, 39 (21%) had feelings of guilt, 60 (32%) reported low energy, 13 (07%) were irritable, 120 (64%) noted decrease in appetite, 2 (1.0%) patients had suicidal ideation (not active). Seventy (37.4%) patients fulfilled the criteria to be clinically declared as suffering from major depression. Only 13 (7%) patients had prior knowledge of major depression.
All variables showed positive correlation with MDD (ranging between +0.021 to +0.66) except hematological malignancies which were negatively correlated (-0.426). Regression analysis shows that patients having non-hematological malignancies were more likely to have MDD than hematological malignancies (Odds ratio [OR]: 25.07; 95% CI: 7.4-84.7; p<0.001). Stage 3 cancer patients had more odds to have MDD as compared to stage ≤2 (OR: 10.06; 95% CI: 1.17-85.7; p<0.01) and stage 4 cancer patients had even higher odds to be suffering from MDD in comparison to stage ≤2 (OR: 24.6; 95% CI: 2.8-214; p<0.01).
Using PASS version 11; 95% CI, with 187 cancer patients, effect size of 0.502 with 1 df (degree of freedom), calculated power of this study is approximately 100%. The effect cells were calculated using cross table made between cancer classification and MDD (Table 2).
Conclusion: Major depression is fairly prevalent but under recognized among cancer patients in Pakistani population. Patients having advanced non-hematological malignancies are more likely to have major depression as compared to other malignancy groups. Higher the cancer stage; higher the odds to have MDD. High clinical suspicion, appropriate questioning and psychiatry consultation should be routinely asked if there is high suspicion. Only few patients had the prior knowledge about depression so patients need to be screened and counseled regarding their symptoms and treatment should be tailored accordingly.
Anwer:In-Cyte: Speakers Bureau; Seattle Genetics: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract