Introduction and Aim. Achievement of deep molecular response (DMR) is the prerequisite for treatment-free remission in chronic phase CML (CP-CML) patients (pts). Pts who fail to achieve early molecular response (BCR-ABL1 > 10% IS) at 3-months (mths), or have high ELTS score at diagnosis have inferior achievement of DMR. We and others have shown that the levels of NK-cell, T-cell, myeloid-derived suppressor cell, and neutrophils in the blood at diagnosis have an impact on DMR achievement. We hypothesized that Cluster of Differentiation (CD) (cell surface marker) gene expression might provide a surrogate marker to characterize immune cell composition. We aimed to identify pts who had a low probability of achieving DMR by 5 years (yrs) by combining 3-mths BCR-ABL1% and CD gene expression. This may enable clinicians to determine whether an individual patient is on a pathway towards DMR and potentially TFR or should be considered for a different therapeutic approach if TFR is the eventual goal.
Methods. 119 blood samples from the imatinib-based TIDEL-II trial were subjected to transcriptomic microarray profiling. A total of 357 CD genes classified by the HUGO Gene Nomenclature Committee CD molecular gene group were assessed. We defined DMR as achieving MR4.5 (BCR-ABL1 < 0.0032%) at two consecutive time points. To construct a predictive model, the samples were randomly assigned to discovery and validation cohorts. Recursive partitioning and construction of a regression tree with tenfold cross-validation based on expression of 357 CD genes and 3-mths BCR-ABL1% were used as inputs in the discovery cohort. The performance was assessed based on accuracy of prediction of DMR by 5 yrs. The final model was validated using the independent validation cohort. All the analysis was performed using R statistical software.
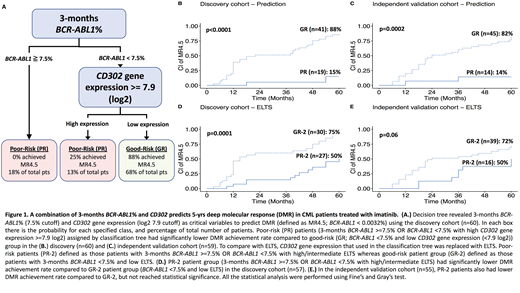
Results. Clinical variables (age, gender, ELTS, 3-mths BCR-ABL1%, MMR, and MR4.5) were well matched in the discovery (n=60) and independent validation cohort (n=59). The predictive model was constructed using the discovery cohort to reveal two risk groups: poor-risk (PR, 15% achieving MR4.5 at 5 yrs, n=19), and good-risk (GR, 88% achieving MR4.5 at 5 yrs, n=41) groups (Figure 1A-B). This model classified PR group by BCR-ABL1 ≥ 7.5% at 3 mths OR BCR-ABL1 < 7.5% at 3 months with high CD302 gene expression (≥7.9 log2 gene expression; top 15%) at diagnosis. GR group was defined as having both BCR-ABL1 < 7.5% and low CD302 gene expression (<7.9 log2 gene expression). These variables were chosen by the model based on accuracy performance in predicting DMR. CD302 is a C-type lectin receptor involved in cell adhesion and migration. It is expressed in myeloid populations as well as in blasts and leukemic stem cells (LSC) in AML. High expression of CD302 in PR pts may be a surrogate for increased LSC. The model was validated in the independent validation cohort. Pts identified as PR in the validation cohort had significantly lower 5-yrs MR4.5 achievement rate (14%, n=14) compared to those with GR (82%, n=45, p=0.0002, Figure 1C).
We asked whether using the more conventional BCR-ABL1 10% cutoff instead of 7.5% in our model would give similar results, but the performance in predicting long-term DMR achievement was inferior: Pts predicted as PR with this criteria had ~2x higher achievement of DMR (e.g. 26% vs 14% using 3-mths BCR-ABL1 10% vs 7.5% cutoff respectively).
ELTS score have been associated with the probability of DMR achievement. We compared the performance of ELTS in combination with 3-mths BCR-ABL1% by replacing CD302 gene expression with ELTS. The predictive accuracy was inferior. Pts with 3-mths BCR-ABL1 ≥7.5% OR BCR-ABL1 <7.5% with high/intermediate ELTS (PR-2) had about 3.3-3.5 fold higher DMR achievement rate than the PR group with CD302 in both discovery and validation cohorts (Figure 1D-E). In contrast, pts with 3-mths BCR-ABL1 <7.5% and low ELTS (GR-2) had approximately 1.1-1.2 fold lower DMR achievement rate than the GR group with CD302 in both discovery and validation cohorts (Figure 1D-E).
Conclusion. We have constructed a predictive model for DMR achievement for pts who receive optimised frontline imatinib therapy. This model performs better than combining ELTS and 3-mths BCR-ABL1%. We postulate that this predictive model could enable identification of poor risk pts at 3 mths who would benefit from intensified therapeutic approaches to obtain eligibility for TFR and potentially optimal clinical outcome.
Yeung:Novartis: Honoraria, Research Funding; BMS: Honoraria, Research Funding; Pfizer: Honoraria; Amgen: Honoraria. Hughes:Novartis: Other: Advisory Board and Symposia, Research Funding; BMS: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.