Introduction:
Allogeneic hematopoietic cell transplantation (HCT) is curative therapy for sickle cell disease (SCD). Good outcomes have spurred an increase in the use of HCT for SCD, including an increasing number of trials using alternative donors. As survival improves, assessment of long-term outcomes and potential late effects (LEs) in this patient population is critical. We evaluated the data reported to the Center for International Blood and Marrow Transplant Research (CIBMTR) to study incidence and risk factors for LEs following HCT for SCD.
Methods:
Patients reported to the CIBMTR with a diagnosis of SCD who had undergone their first HCT between 1996 and June 2015 were included in this analysis. Patients with graft failure were excluded. We performed a descriptive analysis of patient, disease, donor, and transplant-related factors. The cumulative incidence (CI) of LEs was estimated at 1, 3, and 7 years post-HCT. The number of pre- versus post-HCT SCD-specific disease complications was computed. Overall survival (OS) probabilities were calculated using the Kaplan-Meier method. Multivariable Cox regression analysis was used to evaluate risk factors related to OS and LEs.
Results:
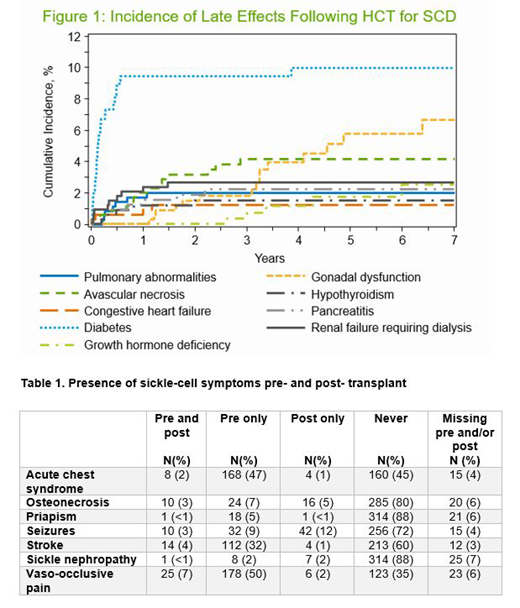
The study population consisted of 355 patients. The median age at HCT was 10 years (range <1-52) and median follow-up was 50 months (range 9-248). The most common indications for HCT were recurrent pain (30%), stroke (29%), and acute chest syndrome (13%). Majority of patients received myeloablative HCT (66%), had a matched sibling donor (59%), and had bone marrow as the graft source (70%). OS at 2, 5, and 7 years was 91%, 89%, and 89%, respectively. Most common causes of death were organ failure (36%), graft-versus-host disease (GVHD; 18%), and infection (13%). Chronic GVHD developed in 30% of patients. Four patients developed a new malignancy post-HCT: AML (N=1; 11 months), MDS/MPN (N=1; 119 months), and lymphoma/lymphoproliferative disease (N=2; 1 and 6 months). The CI of LEs is shown in Figure 1, with highest incidences seen of diabetes, gonadal dysfunction, and avascular necrosis (10%, 6.7%, and and 4.1% at 7 years, respectively, with majority of diabetes occurring in year 1). In multivariable analysis, undergoing HCT when >15 years of age was associated with significantly inferior OS (mortality HR 7.26, 95% CI 3.57-14.77). Multivariable analysis for LEs demonstrated an increased risk of diabetes (HR 7.29, 95% CI 2.94-18.08) and pulmonary abnormalities (HR 5.90, 95% CI 1.14-30.42) with unrelated donor, while older age at HCT was associated with avascular necrosis (HR 14.19, 95% CI 1.86-108.47), diabetes (HR 3.45, 95% CI 1.69-7.05), and congestive heart failure (HR 8.02, 95% CI 1.13-56.94). SCD-related symptoms overall decreased from pre- to post-HCT (Table 1), most notably acute chest syndrome, vaso-occlusive pain crises, and stroke.
Conclusions:
Patients with SCD who have undergone HCT for SCD in recent years have excellent OS, confirmed in this CIBMTR multicenter dataset, with diminished SCD-related symptom burden post-HCT. However, they remain at-risk for a myriad of LEs, with risk factors including older age at HCT and unrelated donor, necessitating systemic organ-based follow up post-HCT. Continued follow-up of this patient population is critical to provide appropriate counseling for medical providers, patients, and families considering HCT as a treatment option for SCD.
Shaw:Therakos: Other: Speaker Engagement.
Author notes
Asterisk with author names denotes non-ASH members.