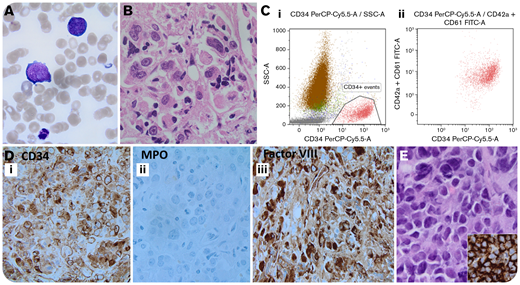
A 78-year-old man with a diagnosis 1 month ago of asymptomatic treatment-naive chronic myeloid leukemia (CML) presented with back pain and dyspnea. Peripheral blood revealed a white blood cell count of 23.8 × 109/L (neutrophils, 22.8 × 109/L; basophils, 0.0 × 109/L; lymphocytes, 0.8 × 109/L), hemoglobin count of 68 g/L, and platelet count of 6 × 109/L, with scattered large mononuclear cells with open chromatin, prominent nucleoli, and deep basophilic cytoplasm with cytoplasmic blebs (panel A; original magnification ×100, May-Grünwald-Giemsa stain). The marrow aspirate was hemodilute; trephine biopsy showed hypercellularity with extensive fibrosis and sheets of blasts (panel B; original magnification ×60, hematoxylin and eosin stain). Flow cytometry (panel Ci-ii) and immunohistochemistry (panels Di-Diii; original magnification ×40) showed that these blasts were positive for CD45 (dim), CD34, CD33, CD42a, CD61, and factor VIII and negative for myeloperoxidase. In addition, a biopsy of a lytic lesion of the ilium bone revealed sheets of large blasts (panel E; original magnification ×40) that were positive for CD34 (panel E inset, original magnification ×40) and CD45 (dim), consistent with a myelosarcoma. Cytogenetics revealed t(9;22) and a complex karyotype. Next-generation sequencing detected TP53 mutation only. A diagnosis of CML in megakaryoblastic crisis was rendered, and the patient succumbed to his illness 9 days later.
The most common blast crisis in CML is myeloid and then lymphoid, but very rarely, megakaryocytic, especially with extramedullary manifestation, which has an even poorer prognosis. This case also emphasizes the importance of performing megakaryocytic markers in the workup for acute leukemia, using flow cytometry and/or immunohistochemistry.
A 78-year-old man with a diagnosis 1 month ago of asymptomatic treatment-naive chronic myeloid leukemia (CML) presented with back pain and dyspnea. Peripheral blood revealed a white blood cell count of 23.8 × 109/L (neutrophils, 22.8 × 109/L; basophils, 0.0 × 109/L; lymphocytes, 0.8 × 109/L), hemoglobin count of 68 g/L, and platelet count of 6 × 109/L, with scattered large mononuclear cells with open chromatin, prominent nucleoli, and deep basophilic cytoplasm with cytoplasmic blebs (panel A; original magnification ×100, May-Grünwald-Giemsa stain). The marrow aspirate was hemodilute; trephine biopsy showed hypercellularity with extensive fibrosis and sheets of blasts (panel B; original magnification ×60, hematoxylin and eosin stain). Flow cytometry (panel Ci-ii) and immunohistochemistry (panels Di-Diii; original magnification ×40) showed that these blasts were positive for CD45 (dim), CD34, CD33, CD42a, CD61, and factor VIII and negative for myeloperoxidase. In addition, a biopsy of a lytic lesion of the ilium bone revealed sheets of large blasts (panel E; original magnification ×40) that were positive for CD34 (panel E inset, original magnification ×40) and CD45 (dim), consistent with a myelosarcoma. Cytogenetics revealed t(9;22) and a complex karyotype. Next-generation sequencing detected TP53 mutation only. A diagnosis of CML in megakaryoblastic crisis was rendered, and the patient succumbed to his illness 9 days later.
The most common blast crisis in CML is myeloid and then lymphoid, but very rarely, megakaryocytic, especially with extramedullary manifestation, which has an even poorer prognosis. This case also emphasizes the importance of performing megakaryocytic markers in the workup for acute leukemia, using flow cytometry and/or immunohistochemistry.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.