Background:
Detection of cytogenetic abnormalities by fluorescent in situ hybridization (FISH) are a critical component of diagnostic workup and prognostication in patients with multiple myeloma. Higher risk cytogenetic abnormalities are defined as t(4;14), t(14;16) and del(17p),1 with 1q21 gain more recently described, and are associated with reduced overall survival and lower response rate.2
Objectives:
To ascertain the impact of presence of multiple high risk cytogenetic abnormalities, "double-hit", on clinical characteristics, response to therapy, overall and progression free survival in newly diagnosed patients with multiple myeloma.
Methods:
We retrospectively analyzed records of 279 patients with multiple myeloma aged over 18 years reviewed and/or treated across two tertiary hospitals (Fiona Stanley Hospital and Royal Perth Hospital) between 1st January 2008 and 31st of December 2019. Karyotyping and FISH on interphase nuclei on bone marrow cells was recorded. High risk cytogenetic abnormalities (HRC) were categorized in accordance with the International Myeloma Working Group (IMWG) definition and included deletion (17p), t(4;14) and t(14;16). Patients were categorized into three groups based on number of HRC present (HRC=0, HRC=1 and HRC>1).
Results:
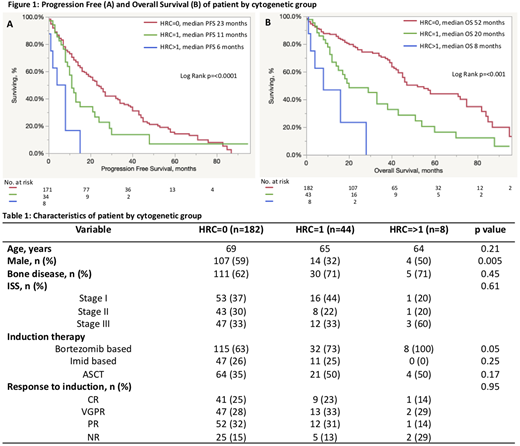
Two hundred and thirty four patients had complete data on HRC and were included in the analysis (n=182 for HRC=0, n=44 for HRC=1 and n=8 for HRC>1). Baseline characteristics for the three groups are listed in Table 1. One or more high risk cytogenetic abnormalities (HRC) were detected in 22.2% of patients, with del(17p) and t(4;14) identified most commonly, at 10.7% and 9.3% respectively. All patients in the HRC>1 cohort had del (17p) with 62% (n=5) having concurrent t(14;16) and 38% (n=3) having t(4;14). Females were more likely to have HRC (41.2% in HRC=0 vs 68.1% in HRC=1 vs 50% in HRC=>1, p=0.0055). Patients in the HRC>1 cohort appeared to have higher ISS stage (60% stage III) however this did not meet statistical significance due to low numbers in the HRC>1 cohort. A greater proportion of patients in the HRC>1 cohort (100%) received bortezomib-based therapy (p=0.05). Overall response rate (ORR) was similar between cohorts, 84.8%, 86.0% and 71.43% in HRC=0, HRC=1 and HRC>1 respectively, p=0.95.
High risk cytogenetic abnormalities were associated with a worse overall survival (OS) and progression free survival (PFS) compared to patients with standard risk disease. Median overall survival (OS) was 52, 20 and 8 months for HRC=0, HRC=1 and HRC>1 respectively, p<0.0001 Figure 1a. Median PFS was 43, 12 and 6 months for HRC=0, HRC=1 and HRC>1 respectively, p<0.0001 Figure 1b.
Conclusions: Patients with multiple high risk cytogenetics, "double hit" myeloma have an exceptionally poor prognosis with earlier relapse and shorter survival than those with a single high risk abnormality. This represents a significant area of unmet need in myeloma therapy and risk adapted treatment intensification strategies need to be evaluated in clinical trials to improve outcomes in this cohort.
Leahy:Pfizer: Membership on an entity's Board of Directors or advisory committees. Sidiqi:Amgen: Honoraria; Celgene: Honoraria, Other: Travel grant; Janssen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.