Key Points
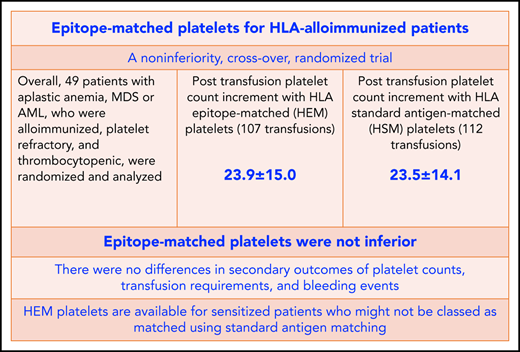
Management of platelet refractoriness resulting from HLA alloimmunization is a major and costly clinical problem.
A noninferiority, crossover, randomized trial supported a role for epitope matched platelets for HLA alloimmunized patients.
Abstract
Platelet transfusion refractoriness results in adverse outcomes and increased health care costs. Managing refractoriness resulting from HLA alloimmunization necessitates the use of HLA antigen–matched platelets but requires a large platelet donor pool and does not guarantee full matching. We report the first randomized, double-blind, noninferiority, crossover trial comparing HLA epitope–matched (HEM) platelets with HLA standard antigen–matched (HSM) platelet transfusions. Alloimmunized, platelet-refractory, thrombocytopenic patients with aplastic anemia, myelodysplastic syndrome, or acute myeloid leukemia were eligible. HEM platelets were selected using HLAMatchMaker epitope (specifically eplet) matching. Patients received up to 8 prophylactic HEM and HSM transfusions provided in random order. The primary outcome was 1-hour posttransfusion platelet count increment (PCI). Forty-nine patients were randomized at 14 UK hospitals. For intention to treat, numbers of evaluable transfusions were 107 and 112 for HEM and HSM methods, respectively. Unadjusted mean PCIs for HEM and HSM methods were 23.9 (standard deviation [SD], 15) and 23.5 (SD, 14.1), respectively (adjusted mean difference, −0.1; 95% confidence interval [CI], −2.9 to 2.8). Because the lower limit of the 95% CI was not greater than the predefined noninferiority limit, the HEM approach was declared noninferior to the HSM approach. There were no differences in secondary outcomes of platelet counts, transfusion requirements, and bleeding events. Adequate 1-hour PCI was more frequently observed, with a mean number of 3.2 epitope mismatches, compared with 5.5 epitope mismatches for inadequate 1-hour increments. For every additional epitope mismatch, the likelihood of an adequate PCI decreased by 15%. Epitope-matched platelets should be considered to support HLA alloimmunized patients. This trial was registered at www.isrctn.com as #ISRCTN23996532.
Medscape Continuing Medical Education online
In support of improving patient care, this activity has been planned and implemented by Medscape, LLC and the American Society of Hematology. Medscape, LLC is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.00 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.0 MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) program. Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider's responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 75% minimum passing score and complete the evaluation at http://www.medscape.org/journal/blood; and (4) view/print certificate. For CME questions, see page 430.
Disclosures
Associate Editor Mario Cazzola, CME questions author Laurie Barclay, freelance writer and reviewer, Medscape, LLC, and the authors declare no competing financial interests.
Learning objectives
Upon completion of this activity, participants will be able to:
Describe primary and secondary outcomes from HLA epitope-matched (HEM) platelets vs HLA standard antigen-matched (HSM) platelet transfusions, according to a randomized, double-blind, noninferiority, crossover trial in 49 patients with alloimmunized, platelet-refractory thrombocytopenia
Determine HLA antibody specificity and identification of target epitopes, according to epitope analysis in patients with alloimmunized, platelet-refractory thrombocytopenia receiving HEM vs HSM platelet transfusions
Identify clinical implications of outcomes of HEM vs HSM platelet transfusions, according to a randomized, double-blind, noninferiority, crossover trial in 49 patients with alloimmunized, platelet-refractory, thrombocytopenia with aplastic anemia, myelodysplastic syndrome, or acute myeloid leukemia
Release date: January 21, 2021; Expiration date: January 21, 2022
Introduction
Platelet refractoriness identifies patients with poorer outcomes and higher costs.1-7 One prospective study of 245 hematology in-patients requiring platelet transfusions showed a significantly longer in-patient stay of a median of 35 days for patients with platelet refractoriness, compared with 14.4 days for those without refractoriness, and higher in-patient costs of $103 956 versus $37 817, respectively.8 Management of platelet refractoriness resulting from HLA alloimmunization is based on provision of platelets from HLA-matched or HLA-compatible donors, where platelets negative for the HLA antigens corresponding to the identified HLA antibodies are selected. However, this strategy is labor intensive and requires the maintenance of a large number of available HLA-typed apheresis donors,9-12 which in England is ∼12 000 donors. Matching is performed at the antigen level, and there is no guarantee a full match will be identified, especially if multispecific HLA antibodies and/or a rare HLA type is present.
Other strategies for platelet refractoriness include use of antigen-negative platelets to avoid specific antibodies or platelets with low expression of specific antigens, such as HLA-B8, -B12, or -A25, despite HLA mismatches,13 platelet crossmatching,12 and acid-treated platelets.14
Specific regions of polymorphism in HLA molecules determine the nature of public and private HLA epitopes. Matching at the epitope level, based on the characterization of short sequences of amino acids from linear or discontinuous regions of the HLA molecules, may be more relevant for assessing HLA compatibility between patients and donors and the effect of donor-specific HLA antibodies. Additional advantages to this approach of epitope matching might extend to more efficient matching for highly sensitized patients and avoidance of some of the challenges of standard matching, without the need to maintain a large panel of HLA-typed apheresis donors.12,15-19
In a retrospective study, we reported the effectiveness of epitope matching in 37 aplastic anemia (AA) patients transfused with 1579 HLA standard antigen–matched (HSM) platelet units using the molecularly defined HLA eplet and triplet epitopes, as well as a correlation between the number of HLA epitope mismatches and the observed platelet count increment (PCI).20 In other studies21-24 and as highlighted in systematic reviews,12,13,25 HLA epitope–matched (HEM) platelets have been reported to show improved PCIs, but these studies have been limited by design, retrospective nature, and lack of clinical outcomes (supplemental Table 1, available on the Blood Web site).
We therefore undertook a randomized, double-blind, noninferiority, crossover trial comparing HEM with HSM platelet transfusions in alloimmunized thrombocytopenic patients with disorders of bone marrow failure. We hypothesized that HEM platelets would result in similar or improved PCIs, longer transfusion-free intervals, and reduced bleeding. A noninferiority study design was indicated, because the objective was to establish that epitope matching is no worse than standard matching, with reduced costs and resource requirements compared with those required for the maintenance of a large panel of HLA-typed apheresis donors. A secondary objective was to compare the 2 approaches with HLA matching of platelets in the context of highly sensitized patients and investigate HLA antibody and epitope specificities. The eplet version of the HLAMatchmaker program was adapted to use high-resolution typing and antibody screening of patients and donors.
Patients and methods
Eligibility criteria
Eligible patients were age ≥16 years with a diagnosis of AA, myelodysplasia (MDS), or acute myeloid leukemia (AML) and refractory to random donor platelet transfusions with documented evidence of HLA antibodies. Patients with palpable splenomegaly, those who had received antithymocyte globulin treatment in the previous 9 days, pregnant or lactating patients, and those unable to give informed consent or comply with the trial protocol were excluded. The following factors were not exclusion criteria but were evaluated in a sensitivity analysis of the primary outcome: use of antimicrobials within 6 hours before transfusion, use of antiplatelet or anticoagulant medication or other medication known to affect platelet refractoriness within previous 7 days, and sepsis or an invasive infection at time of transfusion. Refractoriness was defined as failure on 2 successive occasions to achieve a 10-minute to 1-hour posttransfusion PCI of > 5 × 109/L using ABO-compatible fresh platelets <72 hours old.26,27
Patients and donor HLA and HPA testing
All patients and donors were HLA and human platelet antigen (HPA) typed using molecular techniques for HLA-A, -B, and -C and HPA-1, -2, -3, -4, -5, and -15. Luminex and enzyme-linked immunosorbent assay methods were used to test for HLA- and HPA-specific antibodies, respectively.
HLA antigen and epitope matching
The HSM approach used first-field (low-resolution) HLA type and took into account donor-specific antibodies detected in patients’ serum. The HEM approach was performed using a computer program incorporating the HLAMatchmaker-defined epitopes into a search engine to facilitate the process of HLA antigen– and/or HLA epitope–based platelet selection in platelet transfusion. This program was designed in Microsoft Access and later converted to a Web-based system using the Microsoft SQL Server database and C# programming language based on the Microsoft ASP.NET MVC application framework.28 The program was designed to perform patient-donor compatibility testing by both HSM and HEM methods at HLA-A and -B loci, with an option to include HLA-C. The program allows patient HLA antibody definition at standard HLA antigen and epitope levels and searches to find the most compatible platelet units for each patient, using either the HSM or HEM method.20 Characteristics of transfused platelets are provided in the data supplement.
Intervention
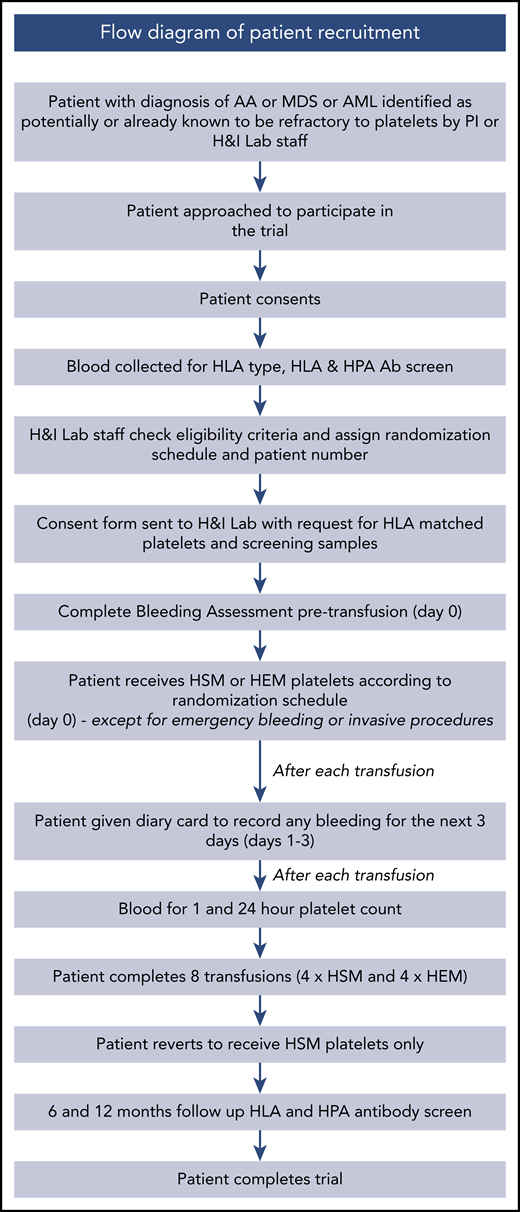
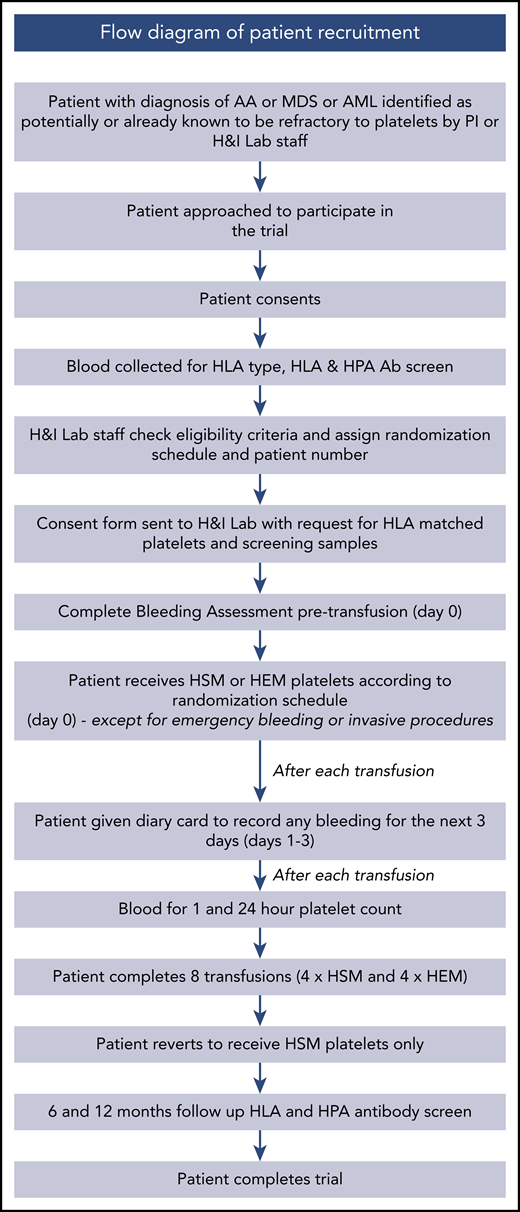
Each patient received up to 8 prophylactic study transfusions, each consisting of 1 platelet unit, comprising 4 each of HSM and HEM units in random order (HSM/HEM platelets are defined in the data supplement). Additional (nontrial) platelet transfusions were given to some patients to treat bleeding or to cover an emergency invasive procedure as necessary (data supplement; supplemental Table 9). The Figure 1 flow diagram shows the process of patient recruitment and progress after recruitment.
Flow diagram showing process of patient recruitment and progress during trial. Ab, antibody; H&I, Histocompatibility and Immunogenetics; PI, principal investigator.
Flow diagram showing process of patient recruitment and progress during trial. Ab, antibody; H&I, Histocompatibility and Immunogenetics; PI, principal investigator.
Outcomes
The primary outcome measure was PCI at 1 hour posttransfusion, defined as the difference between the platelet count at 1 hour after transfusion (range, 10-90 minutes) and the platelet count pretransfusion (taken no more than 24 hours before the transfusion). An adequate 1-hour increment was defined as 10 × 109/L. Secondary outcome measures were PCI at 24 hours (range, 8-36 hours) posttransfusion, corrected count increment (CCI; defined in the data supplement) at 1 hour (range, 10-90 minutes) and 24 hours (range, 8-36 hours) posttransfusion, interval between trial platelet transfusions, patient bleeding events, and grade of HSM matching (either grade A, B1, B2, B3, or B4) and number of epitope mismatches for HEM transfusions. Bleeding events were captured using a modified version of previously piloted self-assessment tools29,30 and reported as a score for 3 days posttransfusion or until the next platelet transfusion, whichever occurred first.
Subgroup analysis of the primary outcome assessed the impact of HLA alloimmunization by calculated reaction frequency (CRF; defined in the data supplement; <40% vs ≥40%) and separately as a post hoc analysis (< 85% vs ≥85%), sex, diagnosis (AA vs MDS/AML), and post hoc donor-recipient blood group match or mismatch on 1-hour PCI. We also performed an analysis of the features of the highly sensitized patient group, in which we compared all the non-self eplets identified on antigens targeted by a patient’s serum.
Data collection and randomization
A daily bleeding assessment form was completed. Patients also completed clinical bleeding assessment forms for 3 days posttransfusion or until the next platelet transfusion, whichever occurred first. Grade of bleed was assigned centrally using a computer algorithm, which was validated previously by comparison with a manual assignment system, using a modified World Health Organization definition of bleeding events.30
Randomization was managed by the NHS Blood and Transplant H&I Laboratory once eligibility had been confirmed and consent obtained. Computer-generated randomization lists were created, which indicated 8 prophylactic study transfusions randomly alternating between the HSM or HEM approach, with 1:1 allocation, plus up to 22 additional transfusions in case any of the first 8 were not evaluable. These were created by the independent statistician and provided to staff at each platelet-issuing laboratory. These were the only individuals unblinded to treatment allocation during the trial.
Analyses
All primary and secondary outcomes were analyzed as intention to treat (ITT), which included all consented participants who were randomized as the primary analysis for the trial. Per-protocol (PP) analysis excluded participants randomized in error and any transfusions where the participant did not receive the treatment specified in the randomization list. No adjustment was made for any center or H&I Laboratory differences, because all laboratories followed the same national protocol. A trial transfusion was considered to be evaluable at 1 hour and 24 hours if pretransfusion and 1-hour and 24-hour posttransfusion platelet counts were both recorded within the time windows (ie, pretransfusion within 24 hours before transfusion and posttransfusion within 10-90 minutes [1 hour] and 8-36 hours [24 hours]).
The primary outcome was analyzed using a normal linear regression model adjusting for pretransfusion platelet count, period effect, and a random patient effect. Carryover from the previous transfusion was not tested for in the model, because it was deemed there should be no carryover effect.
For subgroup analyses, an additional interaction term (between subgroup and treatment) was included. This model and adjustment were also used to analyze 24-hour PCI, CCI at 1 hour and 24 hours, and participant bleeding self-assessment scores. Features of the highly sensitized patient group were also analyzed, in which all non-self eplets identified on antigens targeted by a patient’s serum were compared. (Data supplement provides details of secondary outcomes, sensitivity analyses, and missing data.)
Sample size calculation
Data were used from a retrospective cohort study, where mean PCI was 29.1 × 109/L (95% confidence interval [CI], 22.8 × 109/L to 35.5 × 109/L) and the within- and between-patient standard deviations (SDs) were both 18.5 × 109/L.20 The noninferiority margin was set to 5 × 109/L, as the maximum difference in favor of the HSM method that would be clinically acceptable for the new HEM method to be implemented in practice. Such a difference was also compatible with the CI around the current estimated mean count increment for the standard method of ∼30. Sample size was calculated using simulation (Stata [version 12]), with 2000 repetitions and a 1-sided significance level of 2.5%. Assuming a small amount of dropout (where 25% of patients received only 4 transfusions and the remaining 75% received all 8 transfusions), 40 patients would provide 89% power to exclude a mean difference of 5, based on the lower bound of the 95% CI. It was prespecified that the HEM method would be declared noninferior if the lower bound of the 95% CI were greater than a difference of 5 × 109/L in favor of the standard method. A predefined (blinded) interim analysis at 20 patients confirmed no changes were required to the sample size.
Oversight
This study was undertaken according to Declaration of Helsinki and Good Clinical Practice principles, and ethics approval of the protocol was obtained. All patients provided written informed consent, and safety was monitored by an independent data monitoring committee.
Results
Screening, recruitment, and follow-up
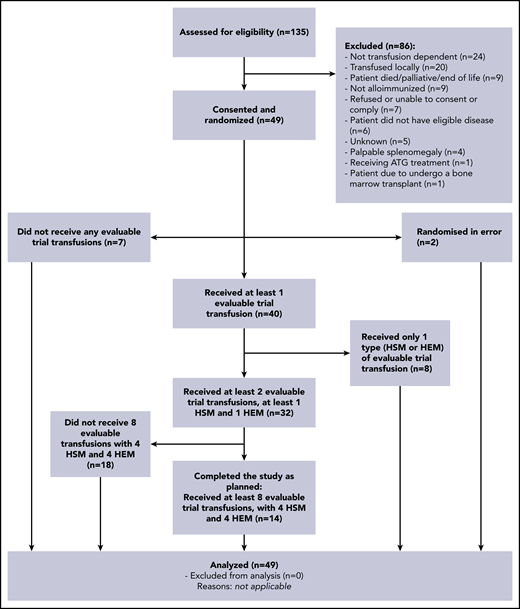
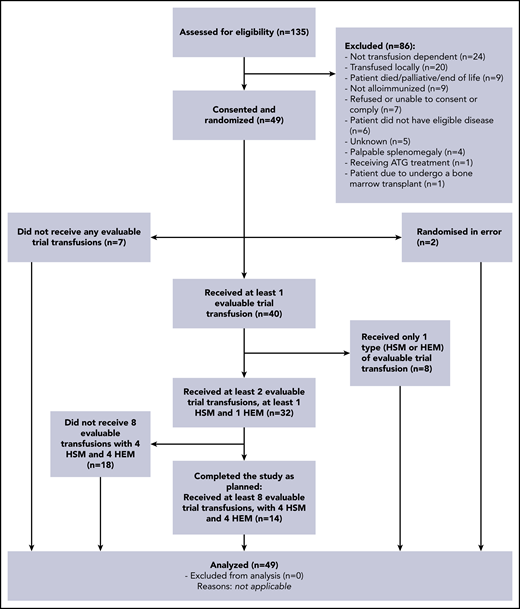
Between October 2012 and November 2015, 135 adult patients diagnosed with AA, MDS, or AML were assessed for eligibility at 14 UK hospitals. Figure 2 (CONSORT diagram) summarizes participants’ progression through the trial. Of these 135 patients, 86 (64%) were excluded and 49 randomized participants were included as per ITT. Seven participants did not receive any evaluable trial transfusions, and 2 participants were randomized in error. Participant characteristics were balanced between the 2 treatment arms (Table 1).
CONSORT diagram. Evaluable here means evaluable at 1 hour posttransfusion. Treatments are as randomized. ATG, antithymocyte globulin.
CONSORT diagram. Evaluable here means evaluable at 1 hour posttransfusion. Treatments are as randomized. ATG, antithymocyte globulin.
Primary outcome
A total of 219 adequate transfusions were evaluated for the study (HEM, n = 107; HSM, n = 112). Results of the primary outcome after transfusions with trial HSM and HEM platelets are presented in Table 2 for both ITT and PP analyses (supplemental Figure 1). For ITT, there was no significant difference in PCI at 1 hour (range, 10-90 minutes) posttransfusion between the 2 treatment arms (P = .9686; adjusted mean difference HEM vs HSM, −0.1; 95% CI, −2.9 to 2.8). Because the lower limit of the 95% CI was > −5, the HEM method was declared noninferior to the HSM method. Similar results were observed for the PP analysis (P = .7469; adjusted mean difference HEM vs HSM, −0.5; 95% CI, −3.4 to 2.4).
The proportion of inadequate PCIs was 16% in both arms (supplemental Table 2). The percentage of nonevaluable transfusions at 1 hour and 24 hours posttransfusion was similar in both treatment arms (proportion of nonevaluable trial transfusions at 1 hour posttransfusion was 48% for HEM and 46% for HSM methods; at 24 hours posttransfusion, it was 54% for HEM and 51% for HSM methods; supplemental Table 3). For both treatment arms, the most common reason for a nonevaluable 1-hour trial transfusion was missing 1-hour posttransfusion platelet count and time (HEM arm, 34%; HSM arm, 47%).
Sensitivity analysis demonstrated no impact on the primary outcome when considering use of antimicrobials within 6 hours before the transfusion, use of antiplatelet or anticoagulant medication or other medication known to affect platelet refractoriness within the previous 7 days, and sepsis or an invasive infection at the time of the transfusion (supplemental Table 4).
When exploring subgroups, there was no interaction between treatment and sex or treatment and diagnosis (P = .4978 and .1890, respectively; supplemental Table 5). For CRF subgroup analysis, using cutoffs of ≥40 and <40, there were insufficient numbers to estimate a treatment effect (supplemental Table 5). Therefore, a post hoc analysis of highly sensitized patients, as defined by CRF ≥85%, was conducted, and no significant interaction with PCI was found (P = .6601; supplemental Table 6). A further post hoc analysis showed no evidence of an interaction between ABO blood group matching/mismatching on the primary outcome (supplemental Table 7).
Secondary outcomes
For both ITT and PP analyses, there was no significant difference in secondary outcomes between the 2 treatment arms (Table 2; supplemental Table 8). For both treatment arms, the most common reason for a nonevaluable 24-hour trial transfusion was missing 24-hour posttransfusion platelet count and time (HEM arm, 56%; HSM arm, 61%). Table 3 lists matching grades for HSM platelets transfused and number of epitope mismatches for HEM platelets.
The impact of HEM mismatching and ABO matching on PCI was examined in a post hoc analysis. Adequate 1-hour PCI was more frequently observed, with a mean number of 3.2 (SD, 3.6) epitope mismatches, compared with 5.5 (SD, 5.3) for inadequate 1-hour increments (P = .0485; Table 4). For every additional 1-epitope mismatch, the chance of an adequate PCI decreased by 15%. There was no interaction between ABO blood group mismatching and treatment arm on 1-hour PCI (supplemental Table 7).
Nontrial platelet transfusions were most often due to nonavailability of trial transfusions (n = 204; 54%) and requirement for a double dose of platelets (n = 159; 41%). Supplemental Table 9 provides a summary of nontrial transfusions. There was no difference in time interval between platelet transfusions (trial and nontrial) between the 2 arms, with means of 74.7 and 69.7 hours (P = .5929) for HEM and HSM transfusions, respectively.
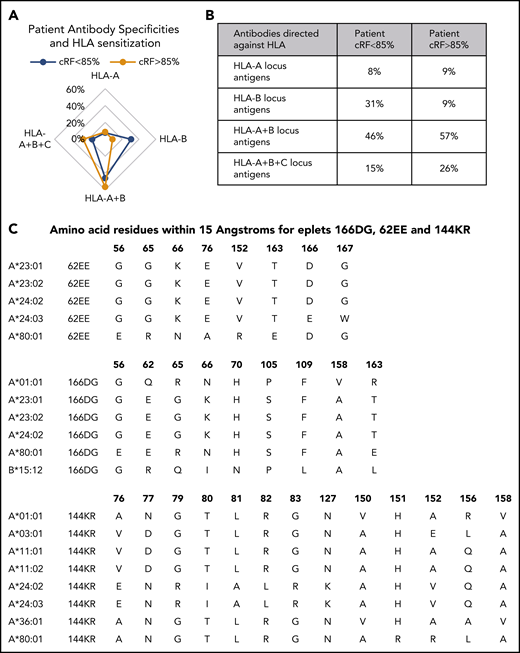
HLA antibody specificity
HLA antibodies were more frequently directed against the more polymorphic HLA-B locus antigens compared with HLA-A and -C. There was evidence of epitope spreading with increased sensitization, where there were more patients with antibodies directed against antigens from >1 locus in the highly sensitized group (Figure 3A-B).
HLA antibody specification and target epitope identification. (A) Frequency of patient antibody specificities and degree of HLA sensitization as defined by CRFs of >80% vs <85%. (B) Percentage of patients with antibodies directed against specific and groups of HLA antigens and according to the degree of HLA sensitization. (C) Amino acid composition of eplet epitopes more frequently found in highly sensitized patients.
HLA antibody specification and target epitope identification. (A) Frequency of patient antibody specificities and degree of HLA sensitization as defined by CRFs of >80% vs <85%. (B) Percentage of patients with antibodies directed against specific and groups of HLA antigens and according to the degree of HLA sensitization. (C) Amino acid composition of eplet epitopes more frequently found in highly sensitized patients.
Epitope analysis: identification of target epitopes
In serum from highly sensitized patients (Figure 3C), the following eplets were identified more frequently: 166DG eplet epitopes found on HLA-A1, -A23, -A24, -A80, and -B15:12; 62EE eplet epitopes found on HLA-A23, -A24, and -A80; and 144KR eplet epitopes found on HLA-A1, -A3, -A11, -A23, -A24, -A36, and -A80. An epitope found on HLA-A23 and -A24 formed from amino acid residues at positions 56, 65, 66, 76, and 152 within 15A was shared between eplets 62EE and 166DG, and these antibody-reactive antigens were more frequent in patients with a CRF of >85% (48%) compared with patients with a CRF of <85% (21%). There were no antibody-reactive antigens bearing shared eplets specific for a highly sensitized patient. However, only 4 patients (14%) were typed as HLA-A*23 or -A*24 in the highly sensitized group, compared with 5 (35%) with a CRF of <85%. The allele frequency of HLA-A*23 and -A*24 (14%) in highly sensitized patients seemed similar to that found in the general population (16%).31 Highly immunogenic HLA-A*02 and HLA-B*07 also had similar allele frequencies between patients and normal population, but eplets found on these antigens were not recognized more frequently in the antisera of highly sensitized patients.
The following case study illustrates the potential value of the HEM approach in specific patients who are highly sensitized. Patient 20005 had an uncommon HLA type in the UK population and was highly sensitized. HLA typing showed HLA-A*66:01, A*69:01, -B*41:02, -B*55:01, -C*01:02, and -C*17:01, and the CRF was 100%. This patient received no A or B1 grade matches, only B2 to B4 mismatches, but all epitope-selected platelets had <12 eplet mismatches (mean, 9.6 eplet mismatches). In contrast, patient 10002 had an HLA type found more frequently in the UK population and, although highly sensitized, received well-matched donations. HLA typing showed HLA-A*03:01, -B*07:02, -B*35:01, -C*04:01, and -C*07:02, and the CRF was 92.58%. All antigen-matched platelets issued for this patient were A grade, and all epitope-selected platelets had no eplet mismatches. Patient 20005 benefited from an HLA epitope matching strategy using the same panel of apheresis donors as used for patient 10002. Therefore, it would not be necessary to expand the HLA-typed apheresis panel to recruit donors with the less common HLA types, like that seen in patient 20005, if an epitope-matching strategy were used for transfusing patients with immunological platelet refractoriness.
Discussion
Our trial has established noninferiority in 1-hour PCI using HEM compared with HSM platelets. We analyzed a large number of evaluable platelet transfusions in a group of patients with myeloid disorders treated with either immunosuppressive therapy or chemotherapy. Baseline characteristics showed that the 2 treatment groups were balanced, including exposure to ABO-incompatible platelets and infections. We used the HLAMatchMaker epitope-matching program with high-resolution HLA typing to provide matching at the eplet level. The robust methodology of our crossover design may also be applicable to other clinical studies aimed at evaluating different products in transfusion medicine.32 We did not demonstrate longer transfusion-free intervals or reduced bleeding using the HEM compared with HSM method, even though we hypothesized an advantage with the HEM approach. A larger study may be required to further examine this effect.
We consider our findings to have implications for practice, including HLA laboratories supporting provision of platelets to alloimmunized patients. Limitations of standard strategies based on the use of HSM platelets are multiple, including less accuracy, because matching is performed at the antigen level, and no guarantee a full match will be found, especially if there are multispecific HLA antibodies and/or a rare HLA type; it is also expensive, time consuming, and labor intensive and requires a large number of available HLA-typed donors. We showed that HEM platelets were available for sensitized patients who might not have been classed as matched using standard antigen matching.
Using an HEM approach, it is possible to identify matched products that would have been missed by searching for HSM platelets, especially important in highly alloimmunized patients. For these patients with panel-reactive antibodies >80%, identification of HLA-matched platelets is especially difficult.10 Knowledge of the restricted HLA antibody and epitope specificity could enable a more cost-effective future approach of specific epitope avoidance without the alternative approach of further increasing the size of a platelet donor pool.
We also explored the impact of the degree of mismatching at the eplet level on PCI, showing that a median of 3.2 mismatches more often produced an adequate PCI compared with a median of 5.5. Furthermore, for every 1 mismatch, the risk of an inadequate PCI increased by 15%. When analyzed in further detail, we showed that HLA antibodies were most often directed against HLA-B locus antigens compared with HLA-A and -C. We also showed that certain eplets (166DG, 144KR, and 62EE) were recognized more frequently among highly sensitized patients, specifically an epitope found on HLA-A23 and -A24.
A previous retrospective study reported a majority mapped to the HLA-A molecule compared with HLA-B, and certain epitopes were immunodominant.33 Although we found no interaction between the degree of sensitization and PCI, we were able to provide HEM platelets for heavily sensitized patients, in whom matched platelets would not have been otherwise available when using standard serological matching. This is illustrated by the case study demonstrating that the chance of finding HLA-compatible platelets depends on patient HLA type and level of sensitization.
Our findings extend results of earlier studies by providing a more robust evaluation of different approaches for selecting platelets for transfusion. In a small study in AA, low numbers of triplet mismatches were associated with better chances of successful transfusion outcomes.21 Brooks et al22 reported that ≤9 triplet mismatches or ≤11 eplet mismatches marked a threshold for successful transfusion. Pai et al23 used HLAMatchmaker for the prospective selection of platelets for alloimmunized patients in a study of 19 patients. If no suitable platelets could be found by serological matching, patients were randomized to receive either cross-reactive group–matched platelets or HEM (eplet) platelets. There was no difference in 24-hour CCIs between grade A HSM, cross-reactive group–matched, or HEM platelets, but a major limitation was the small number of patients evaluated prospectively with HEM platelets (n = 9). In a study of 20 alloimmunized thrombocytopenic patients, higher PCIs using eplet-matched platelets were reported after platelet transfusion, except for those patients receiving an HEM transfusion with a high eplet mismatch score.24
Limitations of our study should be recognized. Only 49 patients were randomized, and of these, only 14 received the total 8 transfusions; however, the trial objectives were comparisons not only between patients but also within patients for each transfusion given, resulting in 219 adequate transfusions evaluated for the study. The interim analysis confirmed that the number of patients was adequate. Additionally, the number of highly sensitized patients was small, and interpretation was limited by the relative frequency of different HLA types in the patients and platelet donor groups. Many patients received platelet transfusions on the day when their platelet count was > 10 × 109/L, reflecting a prior established individual need for regular prophylactic platelets to prevent bleeding, and all patients fulfilled the entry criteria at time of randomization. Finally, disseminated intravascular coagulation, fever, and infection were not exclusion criteria, because we did not want to exclude such patients. We addressed multiple factors in the sensitivity analysis.
In summary, this first randomized trial supports the use of epitope-matched platelets for HLA alloimmunized patients with platelet refractoriness, which may have benefits in terms of more efficient use of resources. Our study design provides a more robust assessment of different platelet products for HLA alloimmunized patients. Management of heavily sensitized patients represents a major clinical challenge; such patients remain at high risk of serious bleeding, because serologically matched HLA-compatible platelets are less often available. A secondary objective of our study was to explore HLA matching of platelets in the context of highly sensitized patients or those cases where discrepancies were identified between results for identification of compatible platelet components between HSM and HEM platelets. We showed that HEM platelet selection can help overcome this problem and highlighted the importance of the degree of mismatching in the selection of platelet units. A review of our national data from the platelet laboratory for NHS Blood and Transplant indicated that from 1 April 2019 to 31 March 2020, 18 552 HLA-selected platelets were issued. There were 908 platelets (4.9%) issued in patients with >2 mismatches. It is these mismatched platelets where an epitope-based approach is being used at present to support more efficient matching (C. Brown, NHSBT, personal communication, 23 July 2020). The alternative approach based on standard matching may require further increases in the platelet donor panel, with associated costs.
Individual participant data that underlie all published HLA Epitope trial results will be available upon request from NHSBT Clinical Trials Unit after deidentification. Beginning 9 months and ending 5 years following article publication, data will be shared with investigators whose use of the data are approved by NHSBT review committee as a methodologically sound proposal. Data will be shared to achieve the aims in the approved proposal.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank all hospital staff and research teams (data supplement) who helped conduct this trial and all the patients who agreed to participate and acknowledge the support of the NHS Blood and Transplant Clinical Trials Unit, including: Val Hopkins (data manager); Brennan Kahan (statistician); Jeff Davies, Claire Critchley, Keith Wilson, Khaled El-Ghariani, and Anna Martin (trial steering committee); and Adrian Newland, Paul White, Gavin Murphy, Michael Greaves, Keith Wheatley, and Marc Turner (data monitoring committee). The study was adopted by the National Cancer Research Network and included in the UKCRN Portfolio (UKCRN ID 13193).
This work was supported by the NHS Blood and Transplant Research & Development Committee (BS08/3).
This report is independent research funded by NHS Blood and Transplant. The views expressed in this publication are those of the authors and not necessarily those of NHS Blood and Transplant.
Authorship
Contribution: All authors critically reviewed the manuscript, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work; J.C.M., S.J.S., D.K., C.V.N., and C.J.B. were responsible for conception and design of the study, interpretation of the data, and preparation of the manuscript; C.A.L., A.J.D., D.S., and A.S.M. managed the study; C.P., J.B., E.S.L., A.Z.G., and K.H. acquired the data; L.L.C. and L.A.P. analyzed the data; R.H. managed the data; C.J.B., A.M., and G.J.M. interpreted the data; and J.C.M. had full access to all the data in the study and had the final responsibility for the decision to submit for publication.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Judith C. Marsh, Department of Haematological Medicine, King’s College Hospital, Denmark Hill, London SE5 9RS, United Kingdom; e-mail: judith.marsh@nhs.net; and Simon J. Stanworth, Radcliffe Department of Medicine, University of Oxford, Oxford OX3 9DU, United Kingdom; e-mail: simon.stanworth@nhsbt.nhs.uk.
REFERENCES
Author notes
J.C.M. and S.J.S. contributed equally to this work.