Abstract
Background: Severe aplastic anemia (SAA) is a rare bone marrow failure disorder associated with significant morbidity and mortality. SAA is characterized by severe pancytopenia and a hypocellular (<25%) bone marrow. The standard of care treatment is hemopoietic stem cell transplant or immunosuppressive therapy (IST) for patients (pts) who are ineligible for transplant. IST usually comprises an antithymocyte globulin (ATG) derived from horse or rabbit, and cyclosporine A (CsA). Although IST can be an effective treatment, individual intolerance, insufficient response, relapse, and clonal evolution remain significant limitations. The lack of global availability of the more effective horse ATG also leaves many pts with limited treatment options and poorer outcomes. In addition, pts with SAA often require transfusions which can be burdensome and negatively impact their quality of life. Eltrombopag (ETB) is indicated for use in pts with SAA who have had an insufficient response to IST (FDA PI, 2014) or are refractory to IST (EMA SmPC, 2015). More recently in the USA, ETB may also be used in combination with IST as first-line (1L) treatment (FDA PI, 2018).
Aims: To assess the efficacy and safety of ETB + CsA (without ATG) as 1L therapy in adult pts with SAA.
Methods: SOAR (NCT02998645) is a Phase 2, single-arm, multicenter, open-label study. Treatment-naive pts with SAA received ETB + CsA for 6 months; responders continued CsA therapy for an additional 24 months (later reduced to 18 months). The primary efficacy endpoint was overall response rate (ORR) by 6 months. ORR was defined as the proportion of pts with complete response ([CR] = absolute neutrophil count [ANC] ≥1000/μL AND platelet count ≥100,000/μL AND hemoglobin ≥10 g/dL) plus the proportion of pts with partial response ([PR] = any 2 of the following counts: ANC ≥500/μL; platelet count ≥20,000/μL; automated reticulocyte count ≥60,000/μL, but not sufficient for a CR). CR and PR were confirmed by 2 assessments ≥7 days apart; transfusion restrictions were also applied. For the primary endpoint to be considered 'clinically meaningful' at least 17/54 pts treated were required to have a response. Other endpoints included ORR by 3 months, ORR at 6 months (ie, confirmed response at the 6-month visit), and transfusion independence, which was defined as transfusion not being required in a period of ≥28 days for platelet transfusions and ≥56 days for red blood cell (RBC) transfusions.
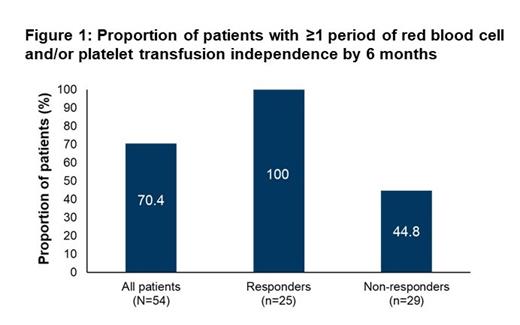
Results: Pts (N=54) had a median (interquartile range [IQR]) age of 55.0 (40.0-67.0) years and 63.0% were male. The majority of pts were White (40.7%) or Asian (40.7%). The median (IQR) duration of exposure to ETB and CsA was 5.7 (2.5-5.8) months and 5.7 (2.4-8.1) months, respectively, and the median (IQR) daily ETB dose was 150.0 (100.0-150.0) mg/day. In the full analysis set, the primary endpoint was met, with 25/54 pts having a CR or PR by 6 months (ORR 46.3%; 95% confidence interval [CI], 32.6-60.4%). Of the 25 responders, 2 (3.7%) achieved a CR by 6 months. ORR by 3 months was 40.7% (95% CI, 27.6-55.0%; n=22/54), and ORR at 6 months was 37.0% (95% CI, 24.3-51.3%; n=20/54). 70.4% of all pts qualified for ≥1 period of RBC and/or platelet transfusion independence by 6 months, including all 25 (100%) responders and 13/29 (44.8%) non-responders (Fig. 1). 40.7% of all pts (responders: 68.0%; non-responders: 17.2%) qualified for ≥1 period of RBC transfusion independence (corresponding percentages for platelet transfusion independence were the same as for the combined RBC and/or platelet endpoint). Adverse events (AEs) occurred in 52/54 (96.3%) pts; 45 (83.3%) pts experienced treatment-related AEs (TAEs), 23 (42.6%) of whom had a grade ≥3 TAE. The most common all-grade AEs were increased blood bilirubin (40.7%), nausea (29.6%), increased alanine aminotransferase (22.2%), and diarrhea (22.2%). Seven (13.0%) pts discontinued treatment due to grade ≥3 AEs. There were 8 on-treatment deaths (aplastic anemia [n=3]; COVID-19, hemorrhage, multi-organ dysfunction syndrome, pyrexia, and thrombosis [all n=1]); no deaths were considered treatment-related.
Conclusion: Data from the SOAR study indicate that ETB + CsA may be beneficial for pts with SAA ineligible for transplant who cannot access or tolerate ATG. All responders and almost half of non-responders qualified for ≥1 period of transfusion independence by 6 months, suggestive of a decreased transfusion burden. No new safety signals were identified.
Vallejo: Novartis: Honoraria; Sanofi: Honoraria; Pfizer: Honoraria. Finelli: Takeda: Consultancy; Celgene BMS: Consultancy, Research Funding, Speakers Bureau; Novartis: Consultancy, Speakers Bureau. Calado: Agios: Membership on an entity's Board of Directors or advisory committees; AA&MDS International Foundation: Research Funding; Alexion Brasil: Consultancy; Instituto Butantan: Consultancy; Novartis Brasil: Honoraria; Team Telomere, Inc.: Membership on an entity's Board of Directors or advisory committees. Peffault De Latour: Novartis: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; Amgen: Research Funding; Alexion: Consultancy, Honoraria, Research Funding; Apellis Pharmaceuticals Inc: Consultancy, Honoraria; Swedish Orphan Biovitrum AB: Consultancy, Honoraria. Kriemler-Krahn: Novartis: Current Employment. Haenig: Novartis: Current Employment. Maier: Novartis: Current Employment. Scheinberg: Alexion pharmaceuticals: Consultancy, Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau; BioCryst Pharmaceuticals: Consultancy; Roche: Consultancy; Abbvie: Consultancy.
In the United States, eltrombopag is a thrombopoietin receptor agonist indicated in combination with standard immunosuppressive therapy (ATG + CsA) for the first-line treatment of adult and pediatric patients aged 2 years and older with severe aplastic anemia (SAA). It is also indicated for the treatment of patients with SAA who have had an insufficient response to immunosuppressive therapy. The SOAR trial aims to assess the efficacy and safety of eltrombopag + CsA (without ATG) as first-line therapy in adult patients with SAA.