Abstract
BACKGROUND: NK cells play a crucial role in the immune surveillance of malignant hemopathies. They undergo fine regulation by the microenvironment and by integrating activating and inhibiting signals trough several receptor/ligand couple interactions, hereafter referred to as "NK synapse". The ligands are expressed by a variety of cell types in the hematopoietic niche, including most immature leukemic stem cells CD34+CD38-. High expression of inhibiting ligands on AML (acute myeloid leukemia) blasts was associated with adverse clinical outcome . This observation highlights the relevance of identifying new ligand/receptor (L/R) pairs that could be targeted to prevent inhibiting interactions at the NK synapse. Relevant interactions to be blocked would display both ligand and receptor expressions on the leukemic cells and NK cells respectively.
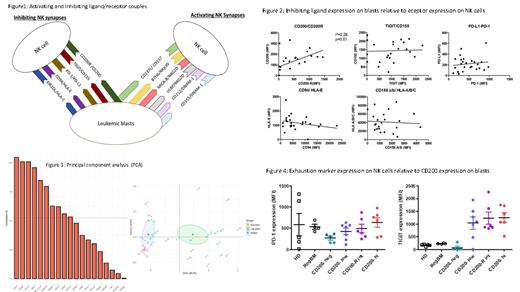
PATIENTS AND METHODS: 23 pediatric AML patients from the pediatric MyeChild01 protocol including in CONECT-AML French national collaborative network project diagnosed between 2018 and 2019 were included in this study. Reference bone marrows used were regenerative (4) or healthy bone marrows (5) . Multicolour flowcytometry protocole used fresh EDTA bone marrow at AML diagnosis and immunostaining with fluorochrome-coupled antibodies using 14 colour panel of L/R couples (Figure 1). Data was acquired on the FORTESSA Becton Dickinson with the Diva software and analysis using script R-PCA and FlowJo .
RESULTS: We studied 5 inhibiting NK synapses (iinhibitory ligand/receptor pairs) . Four out of five inhibiting synapses (TIGIT/CD155; PD1-1/PD-L1; CD94/HLA-E and KIR2DL/HLA-A-B-C), showed not significant expression of ligand associated with the corresponding receptor expression. The CD200/CD200R synapse was the only one in which high ligand expression in blasts was significantly associated with high receptor expression on NK cells (Figure 2). This synapse could thus be of interest to develop targeting therapies for CD200-positive pediatric AML, with the strong advantage that patient eligibility could be easily identified at diagnosis. We then realized a principal component analysis, using the R software (PCA), integrating the MFIs of the 5 inhibiting NK synapses and 6 activating NK synapses (Figure 1) for the pediatric AML cohort (ID #1 to #23 ) together with reference bone marrows (healthy donors (n=5; ID #24 to #28) and regenerative bone marrows (n=4; ID #29 to #32)) . The CD200/CD200R synapse was identified as the main variable, explaining the distribution of patients and healthy donors as both CD200 and CD200R expressions happened to be among the most contributive to PCA axes. Interestingly, healthy donors clustered together, close to regenerative bone marrows. Pediatric AML patients distributed heterogeneously (Figure 3). In parallel, we evaluated whether CD200 expression on bulk leukemia blasts including most immature CD34+CD38- LSC was associated with exhaustion markers on NK cells. We found that patients with high and intermediate expression of CD200 on blasts (MFI > 3 rd quartile and comprised between 2 nd and 3 rd quartile, respectively) displayed strong PD-1 and TIGIT expressions on NK cells. Reciprocally, patients with low CD200 expression (MFI< 2 nd quartile) displayed a moderate PD-1 expression on NK cells, and TIGIT expression was more heterogeneous among individuals (Figure 4).
CONCLUSIONS: Here, we identified CD200 expression in AML blasts including LSC as a marker that could be associated with NK cell exhaustion. at diagnosis. A PCA strategy allowed to observe that this marker differentiated pediatric AML patients NK synapse profiles from healthy donors and regenerative bone marrows sugesting a potential deregulation of bone marrow niche including NK-LSC escape. This suggests that CD200 expression assessment on blasts at diagnosis could be a tool to evaluate NK cell antitumor potential. Indeed, direct NK cell assessment by flow cytometry can be challenging because of blast invasion in the bone marrow. Nevertheless, it remains to be elucidated whether this clustering and exhaustion markers on NK cells correlated with patient clinical outcomes and MRD kinetics including CD34+CD38- LSC flow frequency evaluation that should be useful in most clinical trials to overcome chemoresistance of LSC. These results should be confirmed in a prospectively larger cohort of patients in future clinical trials.
Renard: Jazz Pharmaceuticals: Research Funding.