Abstract
Background: Although clinical trial data exist describing the adverse effects of Bruton's tyrosine kinase inhibitors (BTKi)s, the patient experience outside clinical trials, including differences among agents is less well-described. We evaluated the selection criteria, efficacy and toxicities related to the use of BTKi at our site.
Methods: A retrospective patient chart review was used to collect data from patients treated with one or more BTKi. Demographics, prior therapies, duration of treatment, response to treatment, and incidence and severity of pre-determined toxicities of interest were collected for each patient. Descriptive statistics for each variable were reported. Association between variables of interest and the study cohort were examined using ANOVA for categorical variables and Pearson correlation coefficient for continuous variables. Survival and duration of treatment were estimated using the Kaplan-Meier method according to first novel agent. Survival analysis for each novel agent was conducted using Cox proportional hazards models and log-rank tests.
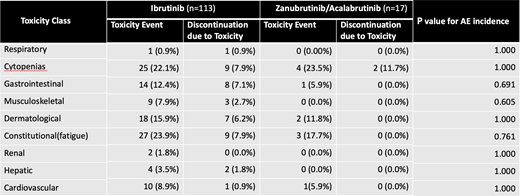
Results: One hundred forty patients were included in this study, including 94 patients with CLL, 24 with MCL, and 22 with other NHL subtypes. One hundred thirteen patients received ibrutinib, while 17 patients received acalabrutinib (n=16) or zanubrutinib (n=1), which were combined in the statistical analysis. Of patients receiving ibrutinib, 69% reported at least one toxicity event during the duration of their treatment. Across all patients who received ibrutinib, 35 individuals did not report a toxicity, 48 individuals reported one toxicity, and 30 individuals reported two or more toxicities. Among the 78 patients who experienced at least one toxicity, 41 (52.5%) discontinued the medication due to these adverse effects, most commonly cytopenias (n=9), diarrhea (n=8), and fatigue (n=9). 57% of patients who reported diarrhea, 36% of patients who reported cytopenias, and 33% of patients who reported fatigue discontinued therapy due to that reported AE. In total, 60/113 patients receiving ibrutinib discontinued therapy, including 40 (66%) due to toxicity and 14 (23.3%) due to disease progression. The remaining patients discontinued therapy due to voluntary choice of new therapy or due to personal decision to stop treatment. Patients remained on ibrutinib therapy for a median duration of 40 months. 53% of patients taking zanabrutinib or acalabrutinib reported at least 1 toxicity, but only 11.7% of patients discontinued therapy for any reason. All patients who discontinued zanubrutinib/acalabrutinib therapy did so due to toxicity, with no patients ceasing therapy due to disease progression. Because only 2 of 17 patients discontinued zanubrutinib/acalabrutinib treatment, a raw median duration of treatment was calculated to be 5 months. 12.4% of patients taking ibrutinib experienced a gastrointestinal toxicity, whereas 5.9% of patients taking acalabrutinib/zanubrutinib experienced a gastrointestinal toxicity (Table 1). Additionally, 8% of individuals taking ibrutinib reported a musculoskeletal toxicity, while no acalabrutinib/zanubrutinib patients reported a musculoskeletal toxicity. There were no statistically significant differences in frequency of toxicities encountered, possibly due to study size. Other toxicities common to all analyzed BTK inhibitors included hematological, cardiovascular, and constitutional adverse effects with no significant difference between agents.
Conclusions: We identified that >1/3 of individuals taking BTK inhibitors are stopping therapy prematurely due to toxicity related outcomes rather than due to disease progression. Our findings suggest that proactive identification and management of adverse effects could prolong therapy duration and provide better outcomes for patients. Strategies to personalize therapy selection to limit therapy discontinuation due to toxicity are needed as additional targeted agents are developed.
Valla: BeiGene: Speakers Bureau. Cohen: Janssen, Adaptive, Aptitude Health, BeiGene, Cellectar, Adicet, Loxo/Lilly, AStra ZenecaKite/Gilead: Consultancy; Genentech, Takeda, BMS/Celgene, BioInvent, LAM, Astra Zeneca, Novartis, Loxo/Lilly: Research Funding.