Key Points
cGVHD is characterized by an expansion of Tph cells in the blood of patients and mice with cGVHD.
Clonally related Tph cells and Trh cells traffic between the blood and cGVHD target tissues.
Abstract
Chronic graft-versus-host disease (cGVHD) is an autoimmune-like syndrome. CXCR5-PD-1hi peripheral T-helper (Tph) cells have an important pathogenic role in autoimmune diseases, but the role of Tph cells in cGVHD remains unknown. We show that in patients with cGVHD, expansion of Tph cells among blood CD4+ T cells was associated with cGVHD severity. These cells augmented memory B-cell differentiation and production of immunoglobulin G via interleukin 21 (IL-21). Tph cell expansion was also observed in a murine model of cGVHD. This Tph cell expansion in the blood is associated with the expansion of pathogenic tissue-resident T-helper (Trh) cells that form lymphoid aggregates surrounded by collagen in graft-versus-host disease (GVHD) target tissues. Adoptive transfer experiments showed that Trh cells from GVHD target tissues give rise to Tph cells in the blood, and conversely, Tph cells from the blood give rise to Trh cells in GVHD target tissues. Tph cells in the blood and Trh cells in GVHD target tissues had highly overlapping T-cell receptor α and β repertoires. Deficiency of IL-21R, B-cell lymphoma 6 (BCL6), or T-bet in donor T cells markedly reduced the proportions of Tph cells in the blood and Trh cells in GVHD target tissues and reduced T-B interaction in the lymphoid aggregates. These results indicate that clonally related pathogenic Tph cells and Trh cells traffic between the blood and cGVHD target tissues, and that IL-21R-BCL6 signaling and T-bet are required for the development and expansion of Tph and Trh cells in the pathogenesis of cGVHD.
Introduction
Chronic graft-versus-host disease (cGVHD) is a systemic autoimmune-like syndrome initiated by alloreactive T cells and perpetuated by autoreactive T cells.1-6 T- and B-cell interactions and autoantibodies contribute to the persistence of cGVHD.7-14 We recently reported that pathogenically expanded tissue-resident T-helper (Trh) cells in GVHD target tissues interact with B cells in lymphoid aggregates to produce immunoglobulin G (IgG) autoantibodies that augment cGVHD pathogenesis.15,16
Follicular T-helper (Tfh) cells play an important role in regulating antibody/autoantibody production.17-20 Previous publications showed that the numbers of CXCR5+PD-1+ Tfh cells in the blood of patients with active cGVHD are lower than in patients without cGVHD. The Tfh cells in patients with cGVHD have high expression of programmed cell death 1 (PD-1) and inducible costimulatory molecule (ICOS) and strong helper function for B cells.21,22 Others have shown an expansion of extrafollicular CXCR5-PD-1hi peripheral T-helper (Tph) cells in the blood of patients with autoimmune diseases.23-26 The expansion of Tph cells was associated with disease severity, whereas the expansion of Tfh cells was not.27 These results raise the question of whether CXCR5-PD-1hi Tph cells have a role in the pathogenesis of cGVHD.
Our studies with murine models indicate that cGVHD onset in recipients with prior acute graft-versus-host disease (GVHD) is associated with destruction of lymphoid follicles and loss of germinal centers (GCs) but expansion of Trh cells in GVHD target tissues.15,28 We quantified Tfh and Tph subsets in patients with or without cGVHD and explored the relationship between Trh cells in GVHD target tissues and Tph cells in the blood in a murine model of cGVHD.
Materials and methods
Patients
Written, informed consent was obtained for all patients before sample collection. The study was approved by City of Hope National Medical Center Institutional Review Board (IRB15172) and Fred Hutchinson Cancer Research Center (IRB9634). Detailed patient information is shown in supplemental Tables 1 and 2 (available on the Blood website).
Animal
BALB/c and C57BL/6 mice were purchased from National Cancer Institute Laboratories. Interleukin (IL)-21R-/- and T-bet-/- mice were purchased from the Jackson Laboratory. Murine models of cGVHD were established and closely monitored and scored according to protocols in our previous publications.15,28
Methods
Sample processing, flow cytometry analysis and cell sorting, T-B–cell cocultures, histopathology and histo-immunofluorescent staining, imaging mass cytometry staining, enzyme-linked immunosorbent assay, adoptive transfer, RNA-sequencing analysis, T-cell receptor (TCR) repertoire sequencing and analysis, and statistical analysis are described in previous publications15,28-30 and supplemental Materials and Methods.
Results
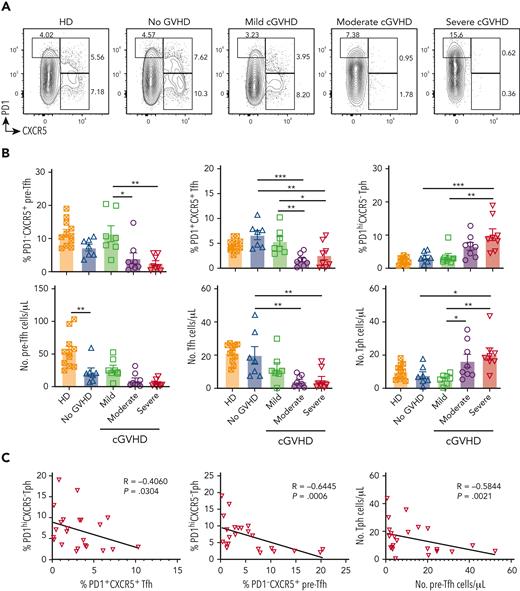
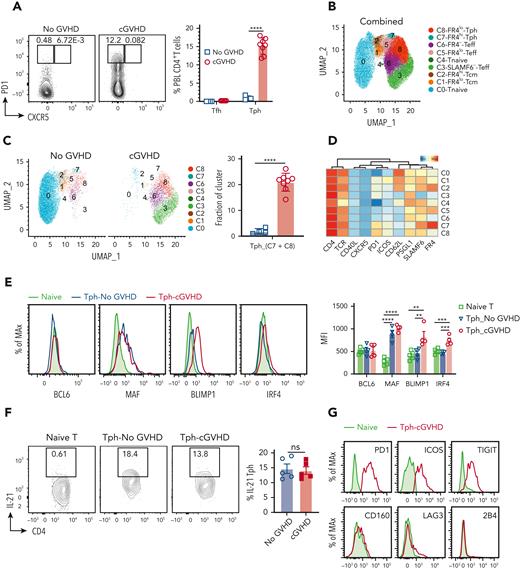
Expansion of Tph cells in patients is associated with cGVHD severity
Reduction of PD-1hiCXCR5+ Tfh cells was reported in the blood of patients with cGVHD,21,22 but changes of PD-1hiCXCR5- Tph cells have not been evaluated. Because cGVHD is a systemic autoimmune-like syndrome,3 and expansion of PD-1hiCXCR5- Tph cells in the blood of patients with other autoimmune diseases (ie, systemic lupus, arthritis, and type 1 diabetes) has been recently reported,23,24,27,31 we investigated whether Tph cells are expanded in the blood of patients with cGVHD. We compared the percentages, numbers, and functional markers of Tph and Tfh in the blood of allogeneic hematopoietic cell transplant (HCT) recipients with or without cGVHD, and the patients with cGVHD were further subdivided into mild, moderate, and severe cGVHD groups (supplemental Tables 1 and 2). Healthy donors (HDs) were used as additional controls. Gated CD3+CD4+CD45RO+ or CD45RA- memory T cells are shown with CXCR5 versus PD-1 staining, which identified 3 subsets: PD-1-CXCR5+ pre-Tfh,32 PD-1+CXCR5+ Tfh, and PD-1hiCXCR5- Tph (supplemental Figure 1A; Figure 1A). The numbers of pre-Tfh cells were lower in the patients without GVHD than in HDs, but the numbers of Tfh and Tph were similar in the 2 groups. The patients with mild cGVHD and patients without GVHD had similar percentages and numbers of the 3 subsets. On the other hand, the patients with mild cGVHD had significantly higher percentages of pre-Tfh and Tfh cells but lower percentages and numbers of Tph cells, compared with the patients with moderate and severe cGVHD. There were no significant differences between patients with moderate and severe cGVHD (Figure 1B). The percentages of Tph cells were inversely correlated with the percentages of Tfh and pre-Tfh cells, and the numbers of Tph cells were inversely correlated with the numbers of pre-Tfh cells (Figure 1C). These results indicate that moderate and severe cGVHD are associated with significant reduction of PD-1-CXCR5+ pre-Tfh and PD-1+CXCR5+ Tfh cells but expansion of PD-1hiCXCR5- Tph cells in the blood.
Expansion of Tph cells is associated with cGVHD severity. Frozen peripheral blood mononuclear cells from patients detailed in supplemental Tables 1 and 2 were thawed and stained with multiple monoclonal antibodies. (A) PD1 versus CXCR5 expression among CD3+ CD45RO+/ CD45RA- CD4+ memory T cells from HDs (N = 11) and patients with no GVHD (N = 7), mild cGVHD(N = 7), moderate cGVHD (N = 8), or severe cGVHD (N = 8) was examined by flow cytometry. (B) Percentage and yield of PD1-CXCR5+ pre-Tfh cells, PD1+CXCR5+ Tfh cells, and PD1hiCXCR5- Tph cells were calculated. (C) Correlation between percentage of Tph cells and percentage of Tfh cells, between percentage of Tph cells and percentage of pre-Tfh cells, and between yield of Tph cells and yield of pre-Tfh cells in patients with cGVHD (N = 23). Data represent mean ± standard error of the mean (SEM). P values were calculated by 1-way analysis of variance (ANOVA) with Holm-Sidak test (B) and nonparametric Spearman correlation (C). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
Expansion of Tph cells is associated with cGVHD severity. Frozen peripheral blood mononuclear cells from patients detailed in supplemental Tables 1 and 2 were thawed and stained with multiple monoclonal antibodies. (A) PD1 versus CXCR5 expression among CD3+ CD45RO+/ CD45RA- CD4+ memory T cells from HDs (N = 11) and patients with no GVHD (N = 7), mild cGVHD(N = 7), moderate cGVHD (N = 8), or severe cGVHD (N = 8) was examined by flow cytometry. (B) Percentage and yield of PD1-CXCR5+ pre-Tfh cells, PD1+CXCR5+ Tfh cells, and PD1hiCXCR5- Tph cells were calculated. (C) Correlation between percentage of Tph cells and percentage of Tfh cells, between percentage of Tph cells and percentage of pre-Tfh cells, and between yield of Tph cells and yield of pre-Tfh cells in patients with cGVHD (N = 23). Data represent mean ± standard error of the mean (SEM). P values were calculated by 1-way analysis of variance (ANOVA) with Holm-Sidak test (B) and nonparametric Spearman correlation (C). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
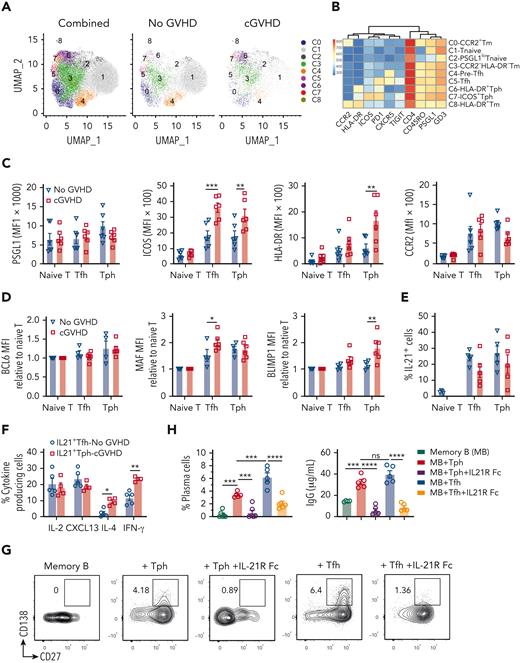
We further analyzed the surface markers of Tfh and Tph cells of CD45RO+ memory CD4+ T cells. Data from 2 representative patients without GVHD and 2 patients with active moderate or severe cGVHD were pooled for cluster identification with UMAP and heatmap generation with FlowSOM according to 10 surface markers. Total CD4+ T cells were grouped into 9 clusters that numbered 0 to 8 (Figure 2A). Cluster 4 has the features of pre-Tfh with high expression of CXCR5 and PSGL1, low expression of ICOS and PD-1, and little expression of HLA-DR. Cluster 5 has the features of Tfh with high expression of CXCR5, PD-1, and PSGL1, low expression of ICOS, and little expression of HLA-DR. Clusters 6/7 have the features of Tph, with high expression of PD-1, PSGL1, and ICOS, but little expression of CXCR5. Clusters 0/8 represent other subsets of CD4+ T cells with little expression of CXCR5 or PD-1 but high expression of CCR2 or HLA-DR (Figure 2B). ICOS expression was higher in Tph and Tfh cells from patients with active cGVHD than in those from patients with no GVHD. HLA-DR expression was higher in Tph but not in Tfh cells when compared with those from patients with no GVHD (Figure 2C).
B-cell helper–related markers and functional analysis of Tph cells in the blood of patients with cGVHD. Thawed mononuclear cell samples from patients with cGVHD were stained with multiple antibodies. (A) Cluster identification was visualized with UMAP, and (B) heatmap was generated with FlowSOM to analyze pooled data from 4 samples, 2 with no GVHD and 2 with active cGVHD. (C) Surface expression of PSGL1, ICOS, HLA-DR, and CCR2 were measured and calculated (N = 6). (D) Intracellular BCL6, MAF, and BLIMP1 were measured among naïve T cells, Tfh cells, and Tph cells between patients with no GVHD (N = 4) and patients with cGVHD (N = 6). (E) IL-21 production by Tfh and Tph cells from patients with no GVHD and patients with cGVHD was also tested (N = 5). (F) IL-2, CXCL13, IL-4, and interferon-γ expression among IL-21–producing Tfh and Tph cells were examined. (G) Sorted CD3+ CD4+ CD45RA- PD1hiCXCR5- Tph and PD1hiCXCR5+ Tfh cells were cultured with memory B cells in vitro in the presence of lipopolysaccharide and staphylococcal enterotoxin B with or without IL-21R Fc for 7 days. CD27+CD138+ plasma cells were measured by flow cytometry, and (H) plasma cell percentages were calculated. Supernatant IgG levels were measured by enzyme-linked immunosorbent assay (ELISA). Data represent mean ± SEM. P values were calculated by 2-way ANOVA with Holm-Sidak test (C, D, F) and 1-way ANOVA with Holm-Sidak test (H). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
B-cell helper–related markers and functional analysis of Tph cells in the blood of patients with cGVHD. Thawed mononuclear cell samples from patients with cGVHD were stained with multiple antibodies. (A) Cluster identification was visualized with UMAP, and (B) heatmap was generated with FlowSOM to analyze pooled data from 4 samples, 2 with no GVHD and 2 with active cGVHD. (C) Surface expression of PSGL1, ICOS, HLA-DR, and CCR2 were measured and calculated (N = 6). (D) Intracellular BCL6, MAF, and BLIMP1 were measured among naïve T cells, Tfh cells, and Tph cells between patients with no GVHD (N = 4) and patients with cGVHD (N = 6). (E) IL-21 production by Tfh and Tph cells from patients with no GVHD and patients with cGVHD was also tested (N = 5). (F) IL-2, CXCL13, IL-4, and interferon-γ expression among IL-21–producing Tfh and Tph cells were examined. (G) Sorted CD3+ CD4+ CD45RA- PD1hiCXCR5- Tph and PD1hiCXCR5+ Tfh cells were cultured with memory B cells in vitro in the presence of lipopolysaccharide and staphylococcal enterotoxin B with or without IL-21R Fc for 7 days. CD27+CD138+ plasma cells were measured by flow cytometry, and (H) plasma cell percentages were calculated. Supernatant IgG levels were measured by enzyme-linked immunosorbent assay (ELISA). Data represent mean ± SEM. P values were calculated by 2-way ANOVA with Holm-Sidak test (C, D, F) and 1-way ANOVA with Holm-Sidak test (H). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
We also compared expression levels of nuclear factors related to T-helper functions (ie, BCL6, MAF, and BLIMP1). No significant differences in BCL6 expression were observed. Both Tph and Tfh had higher expression of MAF compared with naïve CD4+ T cells. Tfh but not Tph from patients with active cGVHD had higher expression of MAF than those from patients with no GVHD. In contrast, Tph but not Tfh from active cGVHD had higher expression of BLIMP-1 than those from patients with no GVHD (Figure 2D). Consistent with the known dependence of IL-21 expression on MAF,33 IL-21 expression was higher in memory Tph and Tfh cells than in naïve CD4+ T cells, with no significant differences between Tph cells and Tfh cells or between patients with cGVHD or no GVHD (supplemental Figure 1B; Figure 2E). Consistent with a previous report,23 PD-1hiHLA-DR+ Tph cells expressed higher levels of MAF and Blimp-1 compared with PD-1hiHLA-DR- cells (supplemental Figure 1C). Thus, like Tfh cells, Tph cells in patients with cGVHD have characteristic surface and nuclear markers of T-helper cells, although differences are also apparent.
Because we observed that Tfh cells from patients without GVHD and patients with active cGVHD had similar percentages of IL-21+ cells (Figure 2E), we used Tfh cells from those without GVHD as the control for functional studies of Tph cells from patients with cGVHD. Compared with IL-21+ Tfh cells from patients without GVHD, IL-21+ Tph cells from patients with cGVHD produced higher levels of interferon-γ and IL-4, with no difference in expression of CXCL13 (ligand of CXCR5) or IL-2 (Figure 2F). Finally, Tph cells from patients with cGVHD and Tfh cells from patients with no GVHD were cocultured with naïve B cells or memory B cells in the presence of staphylococcal enterotoxin B and lipopolysaccharide for 7 days, as previously described.15 Tfh but not Tph cells augmented naïve B-cell differentiation into CD27+CD138+ plasma cells (supplemental Figure 1D). However, both Tph and Tfh cells augmented memory B differentiation into plasma cells and their production of IgG in an IL-21–dependent manner, because neutralizing IL-21 with IL-21R-FC blocked the effect of Tfh and Tph (Figure 2G-H). Taken together, our results demonstrate a marked reduction of Tfh but expansion of Tph in the blood of patients with cGVHD. Like Tfh cells, Tph cells augment memory B-cell differentiation and production of IgG via IL-21.
Expansion of Tph cells in the blood of mice with cGVHD
We used a murine HCT model with C57BL/6 donors and BALB/c recipients that reflect characteristic features of human cGVHD34 to study the Tph cells. The recipients developed acute and cGVHD as determined by clinical manifestations and histopathology (supplemental Figure 2A-B). Recipients given T-cell–depleted bone marrow (TCD-BM) alone were used as no-GVHD controls. On day 60 after HCT, Tfh cells were virtually undetectable in the blood from murine recipients with or without cGVHD, but the proportion of Tph cells in cGVHD recipients was markedly expanded compared with those with no GVHD (Figure 3A). UMAP identified 9 clusters among T cells from cGVHD and no-GVHD recipients (Figure 3B). Recipients without GVHD had predominantly CD62L+ naïve T cells (cluster 0) with a few CXCR5-PD1+ ICOS+ PSGL1+ SLAMF6+ CD62L- Tph cells (Cluster 7/8). In contrast, cGVHD recipients had marked reduction in naïve T cells (cluster 0) but marked expansion of Tph cells (cluster 7/8). In addition, PD-1+ICOS-PSGL1+SLAMF6- cells (cluster 3) and PD-1-ICOS-PSGL1+SLAM6+ cells (cluster 6) among CD62L- memory-like T cells were expanded in cGVHD recipients (Figure 3C-D). Compared with naïve T cells, Tph cells from cGVHD and no-GVHD recipients did not upregulate expression of BCL6. They both upregulated expression of MAF, but only Tph cells from cGVHD recipients upregulated BLIMP-1 and IRF4 (Figure 3E). Stimulated Tph cells from cGVHD and no-GVHD recipients both increased production of IL-21, with no significant difference between the 2 groups (Figure 3F). Tph cells from recipients with cGVHD did not upregulate expression of exhaustion markers CD160, LAG3, or 2B4, although they upregulated expression of PD-1, TIGIT, and ICOS compared with naïve T cells (Figure 3G). Our results indicate that, like Tph cells in the blood of humans with cGVHD, Tph cells in the blood of murine recipients with cGVHD have a PD-1hiCXCR5-ICOS+ phenotype, a similar profile of nuclear transcript factor expression (BCL6-MAF+BLIMP-1+IRF4+), and similar production of IL-21.
An experimental murine model of cGVHD shows expansion of Tph cells in the blood. Irradiated BALB/c recipients were engrafted with TCD-BM alone (no GVHD) or plus splenic Thy1.2+ T cells (2 × 105) to induce cGVHD, and approximately 40% of cGVHD recipients survived at 60 days after HCT. (A) PD1 versus CXCR5 expression among CD4+T cells at day 60 after HCT in the PBL from recipients with no GVHD or with cGVHD. (B, C) Cluster identification was visualized using UMAP to analyze peripheral blood CD4+T cells among 4 recipients with no GVHD and 8 recipients with cGVHD. Fractions of Tph cells were also calculated. (D) Heatmap shows protein expression levels among the clusters in (B). (E) Intracellular expression levels of BCL6, MAF, BLIMP1, and IRF4 were examined among Tph cells from recipients with no GVHD or cGVHD and naïve CD4+ T cells from no-GVHD recipients. MFI was also calculated. (F) PBMCs were stimulated with PMA and ionomycin, and subsequent IL-21 expression levels were measured. (G) Exhaustion-related markers PD1, ICOS, TIGIT, CD160, LAG3, and 2B4 were also compared. Data represent mean ± SEM. P values were calculated by 2-way ANOVA with Holm-Sidak test (A, E) and unpaired Student t test (C, F). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
An experimental murine model of cGVHD shows expansion of Tph cells in the blood. Irradiated BALB/c recipients were engrafted with TCD-BM alone (no GVHD) or plus splenic Thy1.2+ T cells (2 × 105) to induce cGVHD, and approximately 40% of cGVHD recipients survived at 60 days after HCT. (A) PD1 versus CXCR5 expression among CD4+T cells at day 60 after HCT in the PBL from recipients with no GVHD or with cGVHD. (B, C) Cluster identification was visualized using UMAP to analyze peripheral blood CD4+T cells among 4 recipients with no GVHD and 8 recipients with cGVHD. Fractions of Tph cells were also calculated. (D) Heatmap shows protein expression levels among the clusters in (B). (E) Intracellular expression levels of BCL6, MAF, BLIMP1, and IRF4 were examined among Tph cells from recipients with no GVHD or cGVHD and naïve CD4+ T cells from no-GVHD recipients. MFI was also calculated. (F) PBMCs were stimulated with PMA and ionomycin, and subsequent IL-21 expression levels were measured. (G) Exhaustion-related markers PD1, ICOS, TIGIT, CD160, LAG3, and 2B4 were also compared. Data represent mean ± SEM. P values were calculated by 2-way ANOVA with Holm-Sidak test (A, E) and unpaired Student t test (C, F). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
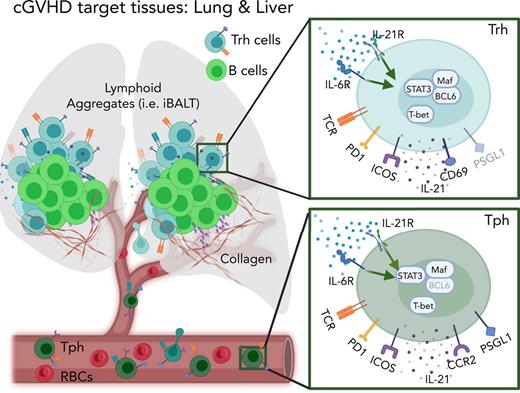
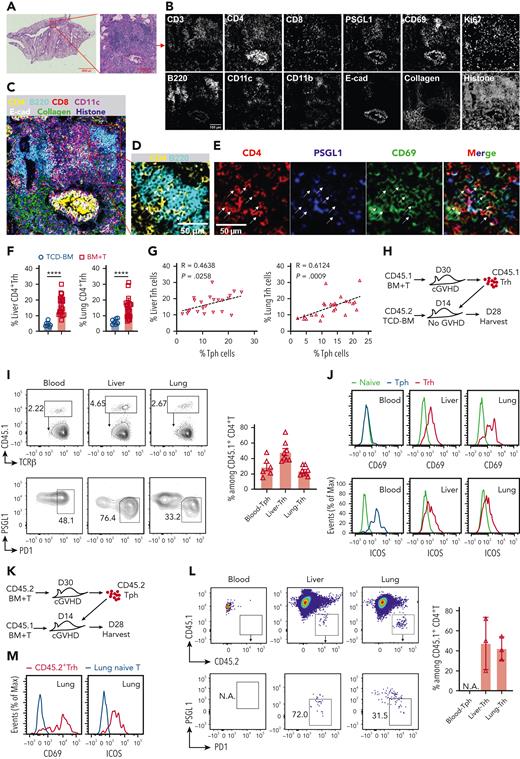
Pathogenic Tph cells and Trh cells traffic between the blood and GVHD target tissues
With imaging mass cytometry, we observed that in GVHD target tissues (ie, lung), the infiltrating lymphocytes formed an inducible bronchus-associated lymphoid tissue35 consisting of CD4+/CD8+ T, B, dendritic cells, and clusters of CD4+ T and B cells, with surrounding collagen deposition (Figure 4A-C). In the inducible bronchus-associated lymphoid tissue, the CD4+ T cells were mainly PSGL1loCD69+CD4+ Trh cells (Figure 4D-E). To explore the relationship between Tph and Trh cells, we first determined whether the percentages of Tph in the blood and Trh cells in GVHD target tissues correlate with each other. Compared with no-GVHD recipients of TCD-BM, the percentage of PSGL1loPD-1+ Trh cells among CD4+ T cells in the GVHD target tissues liver and lung of cGVHD recipients of BM + T was markedly increased (Figure 4F), and the percentage of Trh cells in those tissues was positively correlated with the percentage of Tph cells in the blood (Figure 4G).
Pathogenic Tph cells and Trh cells traffic between the blood and cGVHD target tissues. Lung FFPE slides from cGVHD mice were processed to visualize lymphocyte infiltration via imaging mass cytometry (N = 4). (A) Selected lung lymphocyte infiltration area via hematoxylin-eosin stains. (B) Representative images of 12 markers are shown. (C) Merged channels image shows signals of CD4, B220, CD8, CD11c, E-cadherin, collagen, and histone. (D) Merged channels image shows signals of CD4 and B220 within lung inducible bronchus-associated lymphoid tissue (iBALT). (E) Images show signals of CD4, PSGL1, CD69, and merged channels in lung iBALT. (F) Percentage of liver (N = 23) and lung (N = 25) PSGL1loPD1hi Trh cells among total CD4+ T cells in cGVHD mice and compared with Trh cells (N = 7) from no-GVHD mice by flow cytometry on day 60 after HCT. (G) Correlations between percentage of liver Trh cells and Tph cells, and between percentage of lung Trh cells and Tph cells were analyzed. (H) Diagram of transfer experiments in which donor CD45.1+ Trh cells in the liver and lung of primary cGVHD mice were isolated on day 30 after HCT and transferred into CD45.2+ adoptive recipients of no-GVHD mice on day 14 after HCT. Fourteen days after cell transfer, CD45.1+ T cells were isolated from the adoptive recipients and analyzed (N = 8). (I) Percentages of Tph cells from blood and Trh cells from liver and lung were measured among injected CD45.1+ T cells, mean ± SEM. (J) Representative panel of CD69 and ICOS expression of CD45.1+ Tph cells in the blood and CD45.1+ Trh cells in the liver and lung compared with tissue-matched naïve CD4+ T cells. (K) Diagram of transfer experiments in which donor CD45.2+ blood Tph cells of primary cGVHD mice were enriched at day 30 after HCT and adoptively transferred into CD45.1+ cGVHD recipients at 14 days after HCT. CD45.2+ T cells were monitored 14 days later (N = 3). (L) CD45.2+ T cells in the blood, liver, and lung were identified and tested for PSGL1 versus PD1 expression as shown for 1 representative recipient (left) and calculated (right), mean ± standard deviation. (M) Representative panel of CD69 and ICOS expression of lung CD45.2+Trh cells compared with naïve T cells. P values were calculated by unpaired Student t test (F) and nonparametric Spearman correlation (G). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
Pathogenic Tph cells and Trh cells traffic between the blood and cGVHD target tissues. Lung FFPE slides from cGVHD mice were processed to visualize lymphocyte infiltration via imaging mass cytometry (N = 4). (A) Selected lung lymphocyte infiltration area via hematoxylin-eosin stains. (B) Representative images of 12 markers are shown. (C) Merged channels image shows signals of CD4, B220, CD8, CD11c, E-cadherin, collagen, and histone. (D) Merged channels image shows signals of CD4 and B220 within lung inducible bronchus-associated lymphoid tissue (iBALT). (E) Images show signals of CD4, PSGL1, CD69, and merged channels in lung iBALT. (F) Percentage of liver (N = 23) and lung (N = 25) PSGL1loPD1hi Trh cells among total CD4+ T cells in cGVHD mice and compared with Trh cells (N = 7) from no-GVHD mice by flow cytometry on day 60 after HCT. (G) Correlations between percentage of liver Trh cells and Tph cells, and between percentage of lung Trh cells and Tph cells were analyzed. (H) Diagram of transfer experiments in which donor CD45.1+ Trh cells in the liver and lung of primary cGVHD mice were isolated on day 30 after HCT and transferred into CD45.2+ adoptive recipients of no-GVHD mice on day 14 after HCT. Fourteen days after cell transfer, CD45.1+ T cells were isolated from the adoptive recipients and analyzed (N = 8). (I) Percentages of Tph cells from blood and Trh cells from liver and lung were measured among injected CD45.1+ T cells, mean ± SEM. (J) Representative panel of CD69 and ICOS expression of CD45.1+ Tph cells in the blood and CD45.1+ Trh cells in the liver and lung compared with tissue-matched naïve CD4+ T cells. (K) Diagram of transfer experiments in which donor CD45.2+ blood Tph cells of primary cGVHD mice were enriched at day 30 after HCT and adoptively transferred into CD45.1+ cGVHD recipients at 14 days after HCT. CD45.2+ T cells were monitored 14 days later (N = 3). (L) CD45.2+ T cells in the blood, liver, and lung were identified and tested for PSGL1 versus PD1 expression as shown for 1 representative recipient (left) and calculated (right), mean ± standard deviation. (M) Representative panel of CD69 and ICOS expression of lung CD45.2+Trh cells compared with naïve T cells. P values were calculated by unpaired Student t test (F) and nonparametric Spearman correlation (G). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
We also compared the surface phenotype of Tph and Trh cells. Although Tph cells were CD69-PSGL1hiCCR2+ and Trh cells were mainly CD69+PSGL1loCCR2-, they were both PD-1hiICOS+CCR6+CCR7- (supplemental Figure 2C). Although Trh upregulated expression of BCL6, Tph did not. Both Tph and Trh cells upregulated expression of MAF, compared with naïve T cells from HDs (supplemental Figure 2D). Finally, both Tph and Trh produced IL-21 (supplemental Figure 2E). In addition, we compared Tph cells from cGVHD recipients versus Tfh cells from the spleen of no-GVHD recipients. Compared with Tfh cells, Tph cells expressed higher levels of PSGL1 and BLIMP1 but lower levels of CXCR5, CD69, BCL6, and MAF (supplemental Figure 2F-G). Consistent with destruction of GCs and loss of Tfh cells in the spleen of cGVHD recipients,15,28 few GL7+Fas+ GC B cells were identified in the spleen or blood of cGVHD recipients, but GL7+Fas+ GC-like B cells were expanded in the liver and lung of cGVHD recipients (supplemental Figure 2H). These results indicate that, like Trh and Tfh cells, Tph cells have characteristic features of T helpers, but Tph cells have more similarities with Trh than with Tfh cells.
We used adoptive transfer experiments to determine whether PSGL1hiCCR2+CD69-PD-1hi Tph cells in the blood were related to PSGL1loCCR2-CD69+PD-1hi Trh cells in GVHD target tissues. As shown in Figure 4H, Trh cells were from primary GVHD recipients at 30 days after engraftment of donor CD45.1+Thy1.2+ T cells and TCD-BM. Sorted CD45.1+PSGL1loPD-1hiCD4+ Trh cells (1 × 106) from the liver and lungs of primary GVHD recipients were injected into the adoptive recipients at 14 days after engraftment with CD45.2+ TCD-BM. Fourteen days after the adoptive transfer of CD45.1+ Trh cells, the CD45.1+ T cells were observed in the blood, liver, and lung, although there were few in the spleen (Figure 4I; supplemental Figure 3A-C). Among CD45.1+ T cells in the blood, approximately 30% were PSGL1hiCXCR5-PD-1hi Tph cells. Among CD45.1+ T cells in the liver and lung, approximately 50% and 30%, respectively, were PSGL1loCXCR5-PD-1hi Trh cells that were mainly CD69+ ICOS+(Figure 4I-J). The presence of adoptively transferred Trh cells in the liver was associated with an increase of GL7+Fas+ GC-like B cells and PD-L2+CD80+ memory B cells in the liver, but they had no significant impact on B-cell differentiation in the spleen or lung (supplemental Figure 3D-E). These results indicate that Trh cells in the GVHD target tissues can become Tph cells.
Conversely, we tested whether Tph cells from the blood of cGVHD recipients gave rise to Trh cells in the tissue of cGVHD recipients. Sorted congenic CD45.2+PD-1hi Tph cells (5 × 103) from the blood of primary recipients with GVHD at 30 days after HCT were transferred into adoptive recipients at 14 days after engraftment of CD45.1+ T and TCD-BM cells (Figure 4K). Fourteen days after transfer, the injected CD45.2+ Tph cells were detected in the lung and liver tissues of the adoptive recipients, and ∼40% of them were PSGL1loPD1hi Trh cells that express CD69 and ICOS (Figure 4L-M). These results indicated that Tph cells in the blood can become Trh cells in the GVHD target tissues.
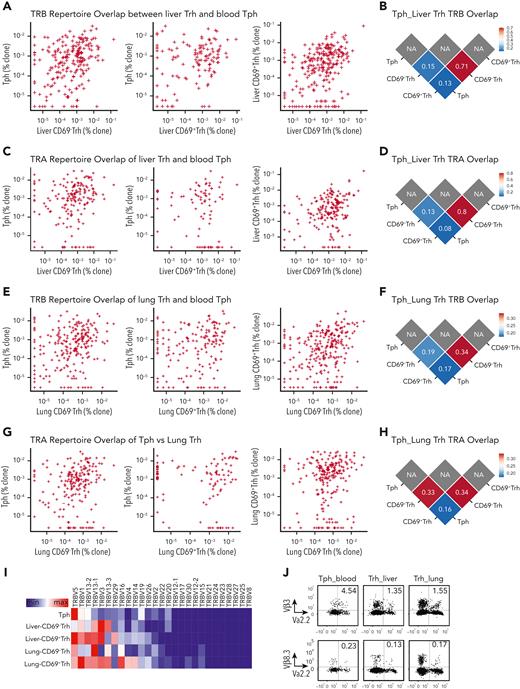
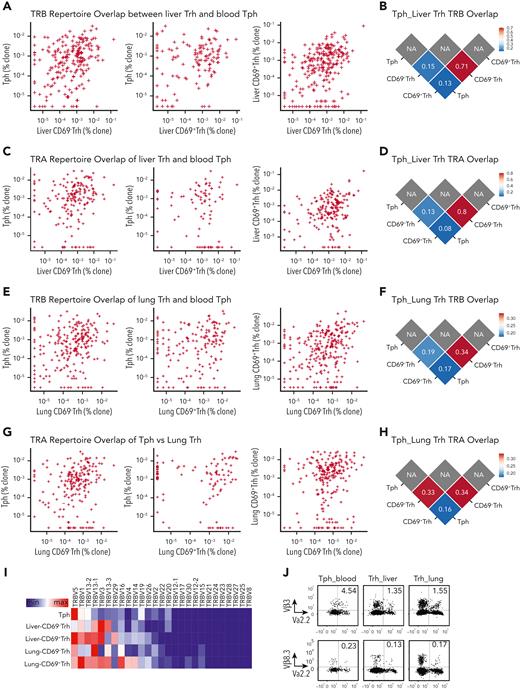
Tph clonotypes in the blood are highly overlapping with Trh clonotypes in cGVHD target tissues
PSGL1lo Trh cells in GVHD target tissues include a large CD69+ subset and a smaller CD69- subset.15 To evaluate the clonal relationship between CD69+ and CD69- Trh cells and their relationship with Tph cells, CD69+ and CD69- PSGL1loPD-1hi Trh subsets from the liver and lung, and PSGL1hiPD-1hiCXCR5- Tph cells from the blood were sorted and analyzed with TCR sequencing. Scatter plots of TCR beta (TRB) show many overlapping TCR clonotypes between Tph from the blood and Trh from the liver, including Tph versus CD69- Trh, Tph versus CD69+ Trh, and CD69+ Trh versus CD69- Trh cells (Figure 5A). TRB repertoire similarities were analyzed with Morisita’s overlap index 0 to 1, in which 0 is no similarity and 1 is fully matched and an index >0.1 is considered as highly overlapping.36,37 The similarity index between CD69+ and CD69- Trh subsets was 0.71, and the index values between CD69+ Trh versus Tph and between CD69- Trh versus Tph were 0.15 and 0.13, respectively (Figure 5B). TCR alpha (TRA) clonotypes between blood Tph and CD69+ or CD69- Trh cells from the liver tissues also showed high overlapping and similarity index values (∼0.08-0.13) (Figure 5C-D).
Tph cells share large portions of repertoires with Trh cells. Tph cells in the blood and CD69+ or CD69- Trh subsets in the liver and lung of cGVHD recipients 30 days after HCT were isolated for TCR-Seq analysis to compare the similarity of TCR repertoires. Because of lymphopenia in cGVHD mice, peripheral blood mononuclear cells from 15 mice were pooled for a single sorting experiment and liver or lung mononuclear cells were pooled from 5 mice. (A, C) Scatterplot comparison of TRB and TRA repertoire fractions between Tph cells and liver CD69+ or CD69- Trh cells. (B, D) TCR repertoire similarity of TRB and TRA in A and C was compared by Morisita’s overlap index. (E, G) Scatterplot comparison of TRB and TRA repertoire fractions between Tph cells and lung CD69+ or CD69- Trh cells. (F, H) TCR repertoire similarity of TRB and TRA in E and G was compared by Morisita’s overlap index. (I) Heatmap of gene use of TRB-V segments among Tph from blood, CD69-, and CD69+ Trh subsets from the liver and lung. (J) Two representative TCR clonotypes TCR-Vα2.2-Vβ3 and TCR-Vα2.2-Vβ8.3 were measured by flow cytometry among Tph cells from blood, Trh cells from the liver, and lung of cGVHD recipients.
Tph cells share large portions of repertoires with Trh cells. Tph cells in the blood and CD69+ or CD69- Trh subsets in the liver and lung of cGVHD recipients 30 days after HCT were isolated for TCR-Seq analysis to compare the similarity of TCR repertoires. Because of lymphopenia in cGVHD mice, peripheral blood mononuclear cells from 15 mice were pooled for a single sorting experiment and liver or lung mononuclear cells were pooled from 5 mice. (A, C) Scatterplot comparison of TRB and TRA repertoire fractions between Tph cells and liver CD69+ or CD69- Trh cells. (B, D) TCR repertoire similarity of TRB and TRA in A and C was compared by Morisita’s overlap index. (E, G) Scatterplot comparison of TRB and TRA repertoire fractions between Tph cells and lung CD69+ or CD69- Trh cells. (F, H) TCR repertoire similarity of TRB and TRA in E and G was compared by Morisita’s overlap index. (I) Heatmap of gene use of TRB-V segments among Tph from blood, CD69-, and CD69+ Trh subsets from the liver and lung. (J) Two representative TCR clonotypes TCR-Vα2.2-Vβ3 and TCR-Vα2.2-Vβ8.3 were measured by flow cytometry among Tph cells from blood, Trh cells from the liver, and lung of cGVHD recipients.
Likewise, we observed high overlapping and similarity index values for TRB (0.17-0.19) and TRA (0.16-0.33) clonotypes between Tph cells and CD69+ or CD69- Trh cells from the lung tissues (Figure 5E-H). On the other hand, the similarity index values for TRB and TRA between Tph and Tfh cells were ∼0.002 or 0.03, respectively (supplemental Figure 4A-B). The TRB segments gene expression profile of blood Tph cells showed high similarity with the profiles of CD69+ and CD69- Trh cells from the liver and lung tissues (Figure 5I). Overlapping of Vα2.2Vβ3 and Vα2.2Vβ8.3 T expression among blood Tph and Trh cells from liver or lung tissues was validated with flow cytometry analysis at protein level (Figure 5J). These results indicate that Tph clonotypes in the blood are highly overlapping with Trh clonotypes in cGVHD target tissues.
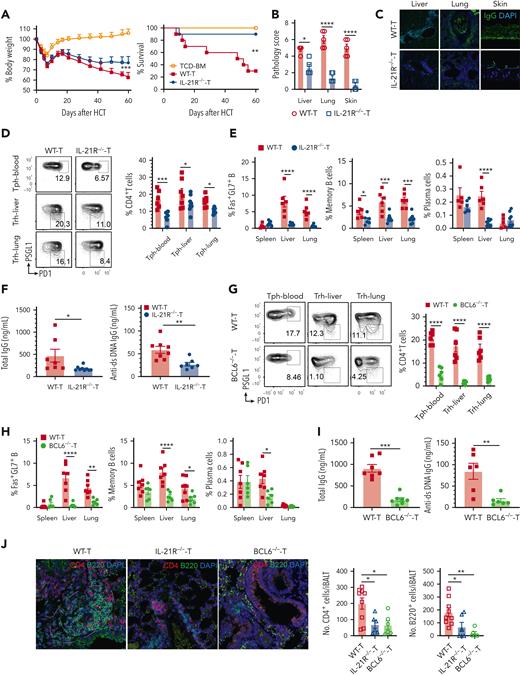
Tph and Trh development and expansion depend on IL-21R-BCL6 signaling
IL-21 plays an essential role in T- and B-cell survival and Tfh development.38-40 Because Tph and Trh cells had a lower expression of IL-21R than Tfh cells (supplemental Figure 5A), we tested whether IL-21/IL-21R signaling has an important role in the expansion of Trh and Tph cells in cGVHD. We observed that IL-21R deficiency in donor T cells significantly reduced cGVHD severity, as judged by higher body weight and survival; lower histopathology scores; reduced fibrosis in the liver, lung, and skin tissues; lower IgG antibody deposition in the liver, lung, and skin tissues; and higher percentages of CD4+CD8+ cells in the thymus compared with control recipients given wild-type (WT) T cells (Figure 6A-C; supplemental Figure 5B-E). IL-21R deficiency in donor T cells also markedly reduced the percentage of PSGL1hiPD-1hi Tph in the blood and PSGL1loPD-1hi Trh cells in the liver and lung (Figure 6D), reduced percentage of GL7+Fas+ GC-like B cells, memory B cells, and plasma cells in the liver and lung, with less striking differences in the spleen and reduced serum concentrations of total IgG and anti–double-stranded DNA (dsDNA) IgG (Figure 6E-F). Administration of blocking anti–IL-21R (clone 4A9), however, did not prevent induction of cGVHD (supplemental Figure 5F-G), although anti-human IL-21 ameliorated Xeno-GVHD.41 Nevertheless, the results with IL-21R-/- donor T cells indicate that IL-21R signaling is important for Tph and Trh development and expansion.
Absence of IL-21R or BCL6 in donor T cells reduces expansion of Tph and Trh cells and ameliorates cGVHD. WT or IL-21R-/- C57BL/6 donor T cells (0.2 × 106) were engrafted with or without WT C57BL/6 TCD-BM cells (2.5 × 106) in lethal total body irradiation–conditioned BALB/c recipients. The BALB/c recipients given TCD-BM alone or with WT-T or IL-21R-/--T cells were assessed at day 60 after HCT. (A) Curves of percent body weight and percent survival are shown. (B) GVHD pathology scores. (C) Representative staining of IgG deposition in the liver, lung, and skin. Original magnification ×200. (D) Tph cells among CD4+ T cells from blood and Trh cells among CD4+ T cells from liver and lung were measured and calculated. (E) Percentages of Fas+GL7+ B cells among total B cells, memory B cells among IgD- B cells, and plasma cells from the spleen and liver were measured. (F) Serum concentrations of total IgG and anti-dsDNA IgG were measured with ELISA. (G) Tph cells among CD4+ T cells from blood and Trh cells among CD4+ T cells from the liver and lung of BALB/c recipients after HCT with TCD-BM plus WT-T or BCL6-/- T cells. (H) Percentages of Fas+GL7+ B cells among total B cells, memory B cells among IgD- B cells, and plasma cells from the spleen and liver were measured. (I) Serum concentrations of total IgG and anti-dsDNA IgG were measured with ELISA. (J) Representative confocal images show CD4+ and B220+ cells in the lung iBALT among WT, IL-21R-/-, and BCL6-/- cGVHD mice. Counts of CD4+ and B220+ cells per iBALT are also shown. Original magnification ×200. Results (mean ± SEM) are combined from 2 replicate experiments. N = 7 to 10. P values were calculated by nonlinear regression with comparison of fits and log-rank test for survival compared with TCD-BM (A), 2-way ANOVA with Holm-Sadik test (B, D, E, G, H), unpaired Student t test (F, I), and 1-way ANOVA with Holm-Sadik test (J). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
Absence of IL-21R or BCL6 in donor T cells reduces expansion of Tph and Trh cells and ameliorates cGVHD. WT or IL-21R-/- C57BL/6 donor T cells (0.2 × 106) were engrafted with or without WT C57BL/6 TCD-BM cells (2.5 × 106) in lethal total body irradiation–conditioned BALB/c recipients. The BALB/c recipients given TCD-BM alone or with WT-T or IL-21R-/--T cells were assessed at day 60 after HCT. (A) Curves of percent body weight and percent survival are shown. (B) GVHD pathology scores. (C) Representative staining of IgG deposition in the liver, lung, and skin. Original magnification ×200. (D) Tph cells among CD4+ T cells from blood and Trh cells among CD4+ T cells from liver and lung were measured and calculated. (E) Percentages of Fas+GL7+ B cells among total B cells, memory B cells among IgD- B cells, and plasma cells from the spleen and liver were measured. (F) Serum concentrations of total IgG and anti-dsDNA IgG were measured with ELISA. (G) Tph cells among CD4+ T cells from blood and Trh cells among CD4+ T cells from the liver and lung of BALB/c recipients after HCT with TCD-BM plus WT-T or BCL6-/- T cells. (H) Percentages of Fas+GL7+ B cells among total B cells, memory B cells among IgD- B cells, and plasma cells from the spleen and liver were measured. (I) Serum concentrations of total IgG and anti-dsDNA IgG were measured with ELISA. (J) Representative confocal images show CD4+ and B220+ cells in the lung iBALT among WT, IL-21R-/-, and BCL6-/- cGVHD mice. Counts of CD4+ and B220+ cells per iBALT are also shown. Original magnification ×200. Results (mean ± SEM) are combined from 2 replicate experiments. N = 7 to 10. P values were calculated by nonlinear regression with comparison of fits and log-rank test for survival compared with TCD-BM (A), 2-way ANOVA with Holm-Sadik test (B, D, E, G, H), unpaired Student t test (F, I), and 1-way ANOVA with Holm-Sadik test (J). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
IL-21-IL-21R-BCL6 signaling is important for Tfh development.42-44 We tested whether this was the case for Trh and Tph. Compared with WT donor T cells, BCL6 deficiency in donor T cells significantly reduced cGVHD severity (supplemental Figure 5H-M), reduced the percentages of PSGL1hiPD-1hi Tph in the blood and PSGL1loPD-1hi Trh in the liver and lung tissues (Figure 6G), reduced the percentage of Fas+GL7+ GC-like B cells, memory B cells, and plasma cells in the liver and lung (Figure 6H), and reduced the concentrations of total IgG and anti-dsDNA IgG in the serum (Figure 6I). Finally, lymphoid aggregates of T-B interactions in the GVHD target tissues (ie, lung) were markedly reduced in recipients given IL-21R-/- or BCL6-/- T cells (Figure 6J). These results indicate that the IL-21R/BCL6 axis plays an essential role in regulating Trh and Tph cell development and expansion during cGVHD pathogenesis.
Tph and Trh development and expansion depend on T-bet
T-bet plays an important role in maintaining the tissue-resident T-cell population.45 We tested whether this is the case for Trh and Tph in cGVHD. First, we observed that Trh cells from GVHD target tissues expressed higher levels of T-bet compared with Tfh cells from the spleen of no-GVHD recipients (supplemental Figure 6A). Thus, we tested whether T-bet deficiency in donor T cells prevented the development of Trh and Tph, using T-bet-/- or WT donor T cells. Consistent with reports by others,46 T-bet deficiency in donor T cells markedly reduced the severity of acute and cGVHD, as judged by higher body weight and survival, lower cutaneous GVHD score, lower thymus damage and histopathology scores in the liver, lung, and skin, and lower IgG antibody deposition in the liver, lung, and skin (Figure 7A-C; supplemental Figure 6B-D). T-bet deficiency in donor T cells markedly increased the percentage of Tfh cells in the spleen (supplemental Figure 6E) but decreased the percentages of CXCR5-PD-1hi Tph in the blood and PSGL1loPD-1hi Trh cells in the liver and lung (Figure 7D), and decreased the T-B clusters in the lung tissues (Figure 7E). T-bet deficiency in donor T cells also increased the percentages of Fas+GL7+ GC-B cells and plasma cells in the spleen but decreased the percentages of Fas+GL7+ GC-like B cells in the liver, with no difference in the percentages of memory B cells in the spleen or liver (Figure 7F). T-bet deficiency in donor T cells resulted in higher concentrations of total IgG but lower concentrations of anti-dsDNA IgG in the serum (Figure 7G). These results indicate that T-bet is required for development and expansion of Trh and Tph cells.
Absence of T-bet in donor T cells reduces expansion of Tph and Trh cells and ameliorates cGVHD. (A) Irradiated BALB/c recipients were engrafted with T cells from WT or T-bet-/- C57BL/6 donors together with TCD-BM from WT C57BL/6 donors. The recipients were monitored for body weight changes and survival for up to 60 days after HCT. Curves of percent body weight, percent survival, and cutaneous cGVHD score are shown. (B) GVHD pathology score. (C) One representative pattern of IgG deposition in the liver, lung, and skin is shown for 4 replicate experiments. Original magnification ×200. (D) Percentages of Tph cells among CD4+ T cells from the blood and Trh cells among CD4+ T cells from the liver and lung of recipients given WT or T-bet-/- donor T cells were examined by flow cytometry. (E) Representative confocal images show CD4+ and B220+ cells inside the lung iBALT of WT and T-bet-/- cGVHD mice. Original magnification ×200. Counts of CD4+ and B220+ cells per iBALT are also shown. (F) Percentages of Fas+GL7+ B among total B cells, memory B cells among IgD- B cells, and plasma cells were measured. (G) Concentration of serum total IgG and anti-dsDNA IgG was measured with ELISA. Mean ± SEM is combined from 2 replicate experiments, N = 10. P values were calculated by nonlinear regression with comparison of fits and log-rank test (A), 2-way ANOVA with Holm-Sadik test (B, D, F), and unpaired Student t test (E, G). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
Absence of T-bet in donor T cells reduces expansion of Tph and Trh cells and ameliorates cGVHD. (A) Irradiated BALB/c recipients were engrafted with T cells from WT or T-bet-/- C57BL/6 donors together with TCD-BM from WT C57BL/6 donors. The recipients were monitored for body weight changes and survival for up to 60 days after HCT. Curves of percent body weight, percent survival, and cutaneous cGVHD score are shown. (B) GVHD pathology score. (C) One representative pattern of IgG deposition in the liver, lung, and skin is shown for 4 replicate experiments. Original magnification ×200. (D) Percentages of Tph cells among CD4+ T cells from the blood and Trh cells among CD4+ T cells from the liver and lung of recipients given WT or T-bet-/- donor T cells were examined by flow cytometry. (E) Representative confocal images show CD4+ and B220+ cells inside the lung iBALT of WT and T-bet-/- cGVHD mice. Original magnification ×200. Counts of CD4+ and B220+ cells per iBALT are also shown. (F) Percentages of Fas+GL7+ B among total B cells, memory B cells among IgD- B cells, and plasma cells were measured. (G) Concentration of serum total IgG and anti-dsDNA IgG was measured with ELISA. Mean ± SEM is combined from 2 replicate experiments, N = 10. P values were calculated by nonlinear regression with comparison of fits and log-rank test (A), 2-way ANOVA with Holm-Sadik test (B, D, F), and unpaired Student t test (E, G). ∗P < .05; ∗∗P < .01; ∗∗∗P < .001; ∗∗∗∗P < .0001.
Discussion
In the current studies, we observed that CXCR5+PD-1+ Tfh cells were markedly reduced in the blood of patients with moderate and severe cGVHD, consistent with previous reports,21,22 but strikingly, the numbers of CXCR5-PD-1hi Tph cells in those patients were significantly increased. Murine models also showed marked expansion of PSGL1hiCXCR5-PD-1hi Tph cells in the blood of recipients with cGVHD, and the expansion was positively correlated with expansion of PSGL1loCXCR5-PD-1hi Trh cells in GVHD target tissues. PSGL1hi Tph cells in the blood are clonally related to PSGL1lo Trh cells in GVHD target tissues. These cell types traffic between the target tissues and the blood in cGVHD recipients, as indicated by adoptive transfer of Trh or Tph cells. These observations provide novel insights and implications regarding the role of Tph and Trh cells in the pathogenesis of cGVHD.
Our results show that circulating PSGL1hiPD-1hi Tph cells in the blood can exchange between tissue-resident PSGL1loPD-1hi Trh cells in GVHD target tissues and vice versa. Similar trafficking has been observed in a reinfection model showing that CD69+ tissue-resident memory CD8+ Trm cells could downregulate expression of CD69 and enter circulation.47,48 PSGL1lo Trh cells in GVHD target tissues were mainly CD69+ but also contained a small CD69- subset. The TCR repertoires of CD69+ and CD69- Trh subsets in GVHD target tissues showed high clonal overlap with each other and with Tph cells in the blood. Because the pathogenic Trh cells in the tissues are constantly stimulated by antigens from donor- and host-type tissue cells, we hypothesize that although CD69+ Trh cells remain in the tissue and interact with memory B cells to produce IgG autoantibodies,15 CD69+PSGL1lo Trh cells can downregulate expression of CD69 and upregulate expression of PSGL1 and become CD69-PSGL1hi Tph cells in the blood. The Tph cells may subsequently reenter GVHD target tissues and revert to CD69+PSGL1lo Trh cells. Our previous15,28 and current studies indicate that IL-6/Stat3/BCL6 and IL-21/IL-21R/Stat3/BCL6 pathways play important roles in regulating the exchange and circulation between Tph and Trh cells during cGVHD pathogenesis. Details of the mechanisms that regulate this exchange remain to be elucidated.
In lymphoid tissues such as the spleen, GL7+Fas+ B cells represent GC-B cells that interact with Tfh cells.49 Our results show that Trh cell interaction with B cells in GVHD target tissues leads to expansion of GL7+Fas+ GC-like B cells independent of GC interactions.50 Loss of Tfh cells and GC-B cells was associated with lymphopenia in the blood and lymph tissues but higher percentages of GC-like B cells in cGVHD target tissues. Amelioration of cGVHD by T-bet deficiency in donor T cells was associated with higher percentages of Tfh and GC-B cells in the spleen and higher concentrations of total IgG in the serum. In contrast, the amelioration of cGVHD by T-bet deficiency in donor T cells was associated with lower percentages of Tph in the blood, lower percentages of Trh and GC-like B cells in GVHD target tissues, and lower concentrations of anti-dsDNA IgG in the serum. These results indicate that T-bet+Trh cell interaction with B cells in GVHD target tissues leads to expansion of GC-like B cells that produce IgG autoantibodies. CD11c+ B cells are also expanded in the blood of patients with cGVHD.51 The relationship between GC-like B cells and other newly identified B-cell subsets in patients and murine recipients with cGVHD is under investigation.
In summary, our studies demonstrate that cGVHD in patients is associated with a reduction of Tfh cells but expansion of Tph cells that augment memory B-cell production of IgG antibodies in an IL-21–dependent manner. With murine models, we demonstrate that PSGL1hiCXCR5-PD-1hi Tph cells in the blood of cGVHD recipients and PSGL1loCXCR5-PD-1hi Trh cells in GVHD target tissues are clonally related. Our studies suggest that the proportion of Tph cells among CD4+ T cells in the blood of patients with cGVHD could reflect pathogenic tissue-resident T cells in GVHD target organs. The proportion of Tph cells among CD4+ T cells in the blood could serve as a measure of disease activity and therapeutic effect in GVHD target tissues, as suggested for other autoimmune diseases and chronic lung transplant rejection.23,24,31,52,53 This question will need to be further addressed in future studies.
Acknowledgments
The authors thank all the anonymous patients. The authors also thank Lucy Brown and her staff at the COH Flow Cytometry Facility, Aimin Li and her staff at COH Pathology-Solid Tumor Core, Brian Armstrong and his staff at COH Light Microscopy Core, and Richard Ermel and his staff at COH Animal Research Center for providing excellent service.
This work was mainly supported by National Institutes of Health (NIH), National Institute of Allergy and Infectious Diseases grant R01 AI066008 and R56 bridged fund and partially supported by NIH, National Cancer Institute grants R01 CA228465 and NCI P30CA033572, as well as Legacy Heritage Fund.
Authorship
Contribution: X.K. designed, performed research, acquired and analyzed data, and prepared and wrote the manuscript; X.W. designed and analyzed and H.Q. performed the TCR and RNA sequencing; B.W., Deye Zeng, K.C., U.N., M.Z., and A.W. assisted in experiments; W.T., A.S., R.N., and P.J.M. provided patient samples and collected clinical data; R.N. provided advice on the clinical experimental design; P.J.M. provided advice on the experimental design and critically reviewed and edited the manuscript; and Defu Zeng designed and supervised the research and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Defu Zeng, The Beckman Research Institute of City of Hope, 1500 E Duarte Rd, Duarte, CA 91010; e-mail: dzeng@coh.org.
References
Author notes
The raw TCR repertoire data can be accessed in the National Center for Biotechnology Information sequence Read Archive under Accession Number GSE200520. All other datasets generated during the current study are available via reasonable request by contacting the corresponding author.
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.