Abstract
HLA incompatibility increases the risk of transplant-related complications. Specifically, donor-specific antibodies (DSA) in mismatched related transplants (mm-HCT) increase the risk of graft failure. Less is known about the role of recipient-specific antibodies (RSA) detected in donors, as the immune status of the donor is not routinely examined before transplant with regard to anti-HLA antibodies. These antibodies may be transferred together with transplanted cells or produced by memory donor cells. We hypothesize that donor-derived RSA may induce immune-mediated complement activation in the classical pathway (CH50), leading to overproduction of membrane attack complex (MAC) and exacerbation of endothelial damage. Here we present preliminary epidemiological data regarding the presence of DSA and RSA, and the impact of RSA antibodies on transplant-related complications, especially transplant-associated thrombotic microangiopathy (TA-TMA) and acute graft-versus-host disease (aGvHD).
Methods We prospectively analyzed the presence of anti-HLA antibodies in 20 pairs of donors and recipients qualified for mm-HCT. All recipients suffered from hematological malignancies and received a myeloablative conditioning regimen and immunosuppression consisting of post-transplant cyclophosphamide, tacrolimus, and mycophenolate mofetil. Patients’ and donors’ immunization status were tested with the solid phase method. Tests were carried out using a flow fluorometer across the screening range (Luminex Screen, One Lambda, USA). In the group of positive samples for anti-HLA class I and/or II antibodies, identification of the specificity of the HLA antibodies was performed (Luminex Single Antigen Beads, One Lambda, USA). Reagents enabling the determination of anti-HLA antibodies in the IgG class were used. All results were presented as mean fluorescence intensity (MFI) values. Monitoring of complement activation on days 30, 60, and 100 post-transplant was started after completing epidemiological data in the first 10 pairs. All patients were checked for TA-TMA and GvHD development during routine post-transplant visits. TA-TMA screening included TA-TMA triad: hypertension or kidney injury, LDH increase and decrease in number of platelets or refractoriness to transfusions, and additionally decrease in hemoglobin concentration, proteinuria, and clinical presentation with TA-TMA involved organ damage. Schistocytes as non-objective and nonrepeatable markers were excluded from diagnostic criteria.
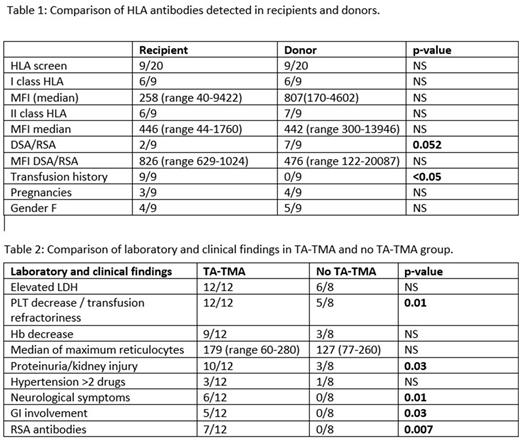
Results Anti-HLA antibodies were detected in 9/20 (45%) of recipients, and in 9/20 (45%) of the donors despite the lack of any transfusion history in donor group. Neither the presence of DSA nor RSA was affected by gender. RSAs were present more often in donors (7/9; 77%) than DSAs in recipients (2/9; 22%); p=0.052. Data summarizing MFI values and type of antibodies are presented in table 1.
Laboratory diagnosis of TA-TMA met 12/20 (60%) patients, with a significant clinical presentation including severe hypertension (3) pericarditis (1), gastrointestinal (5), or neurological (6) impairment in 8/12 (66%). All patients with RSA (7/7; 100%) developed TA-TMA compared to no-RSA group (5/13; 38%) (p<0.01). TA-TMA-mediated organ damage was noticed more often in the RSA population (5/7; 71%) compared to the no-RSA group (3/13, 23%) (p<0.01); (Table 2). A trend for higher activation of CH50 and MAC in RSA compared to a no-RSA group was noted with a mean CH50 93 vs. 82 (p=0,16), and MAC 1428 vs. 1007 (p=0,24) respectively. A trend for higher maximum concentrations of tacrolimus 14 vs 10.7 (p=0.07) was observed in patients with TA-TMA. There was no impact of ABO incompatibility on TA-TMA development.
During the time of observation 6 patients (30%) developed aGvHD - grades I, II, and III were diagnosed in 3, 1, and 2 patients respectively. Only 1 patient with RSA developed aGvHD. There was no correlation between RSA and GvHD occurrence (RSA 1/7, no-RSA 5/13, p=0.26) and between aGvHD and TA-TMA. CMV reactivation was documented in 13/20 (65%) patients, with no differences between the RSA and no-RSA groups (p=0.65).
Conclusions RSAs occur surprisingly often in the donor population, irrespectively to the donor`s gender and the lack of transfusions history. The exact role of these antibodies is not fully understood; however, our data may suggest their impact on complement activation and TA-TMA induction.
Disclosures
Sadowska-Klasa:Novartis: Honoraria, Speakers Bureau; Astellas: Honoraria, Speakers Bureau; Abbvie: Honoraria, Speakers Bureau. Zaucha:Abbvie: Honoraria, Speakers Bureau; Astellas: Honoraria, Speakers Bureau; Roche: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.