Abstract
INTRODUCTION Co-production of care in hematopoietic stem cell transplantation (HSCT) involves collaborating with patients to optimize treatment for their specific needs. This project integrates both clinical data and patient reported outcomes (PRO) in HSCT patients over a 12-month period using an electronic dashboard.
METHODSPatient Population Patients 18 years of age or older, who would receive their first autologous or allogeneic HSCT at Dartmouth-Hitchcock Medical Center were eligible to participate.
Identifying the Appropriate Patient Reported Outcome (PRO) Surveys In 2016, the Center for International Blood and Marrow Transplant Research recommended a standardized approach to the collection of PRO to allow comparisons among HSCT patients (Shaw, 2016). The committee identified the Patient-Reported Outcomes Measurement Information System (PROMIS) Profile 29-item instrument because it had been well validated in various cancer patient populations (Jensen, 2017) and HSCT patients (Shaw, 2018, Lee, 2018). We collected the PROMIS-29 from 65 patients receiving HSCT at five time points: pre-HSCT and at 1-, 3-, 6-, and 12-months post-HSCT.
Statistical Analysis Primary analyses used PRO scores at each assessment, with a mixed effects longitudinal regression model including a random individual effect to account for correlation between repeated measurements within individuals. All models were adjusted for age, gender, type of HSCT, and baseline score. In addition, we performed type of HSCT subgroup analyses, and outcomes were stratified by type of HSCT through interaction term between 'type of stem cell transplant’ and 'assessment time-period'. Analyses were performed using SAS software, version 9.4 (SAS Institute Inc., Cary, NC). Statistical significance was defined as p < 0.05 based on a two-sided hypothesis test with no adjustments made for multiple comparisons.
Patient Characteristics 65 patients were included. The median age was 62 years. 52% of the participants were female and 48% were male. 42% received an allogeneic transplant and 58% received an autologous transplant. Diagnoses included ALL 3%, AML 25%, Hodgkin Lymphoma 8%, Non-HL 20%, MDS 8%, multiple myeloma 35%, and MPN 2%.
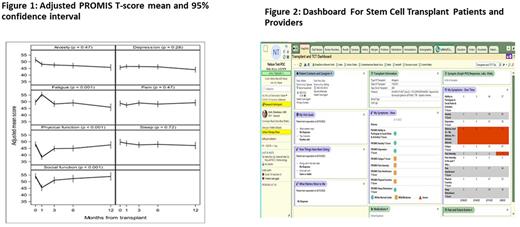
Development of Dashboard to Display PRO Data The HSCT care team and patients co-designed an electronic health record dashboard that could be used during the clinic visit to integrate PROs into the care of patients undergoing HSCT. The dashboard visually displays the PROMIS-29, clinical data (transplant characteristics, labs, medications, and upcoming appointments), and patient-generated responses to questions on goals of care and primary concerns to discuss during the appointment. Preliminary feedback was gathered from 8 patients via exit surveys.
RESULTS There was no association between transplant type and PROMIS-29 domains. We found a statistically significant difference in trends over time in PROMIS-29 physical functioning, social functioning, fatigue, and anxiety domains. There was heightened impairment in physical functioning, social functioning, and fatigue occurring at 1-month post-transplant, but these domains returned to pre-HSCT levels by 3-months post-HSCT for physical functioning and fatigue and by 6-months post-transplant for social functioning. There was a significant reduction in anxiety at 3-months post-transplant compared to the pre-HSCT assessment. (Figure 1) The dashboard (Figure 2) is displayed during the clinic visit and both the patient and the clinician review the results together. Patient feedback has been positive. Most patients reported that it helped them better understand their clinical status (75%, n=6), facilitated discussion with their clinician about what matters most (75%, n=6) and helped them work with their clinicians to make informed make informed decisions (63%, n=5).
DISCUSSION This project provides early insight on the change in PROs over the first 12 months following HSCT. It also supports the feasibility of a patient-provider dashboard to integrate PRO data into the clinic visit. The dashboard facilitates the co-creation of health care visit agendas by patients and clinicians. This simultaneously connects patients with their data and helps clinicians better understand patients’ specific needs.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.