Abstract
Introduction: Lupus Anticoagulant (LA) is an autoantibody that in vitro inhibit phospholipid-dependent coagulation reactions in the absence of specific coagulation factor inhibition
Primary laboratory criteria for LA detection include prolonged clotting time of a phospholipid dependent test, failure of correction on mixing study, shortening of the clotting time in the presence of high phospholipid concentrations & absence of other inhibitors. (1)
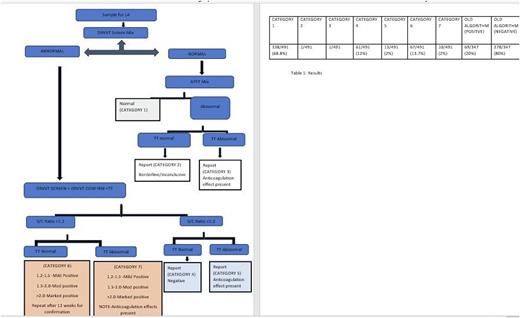
According to guidelines,for diagnosing LA two tests based on different principles should be used- dRVVT(Dilute Russel's Viper Venom Time) should be the first test considered. Second test should be a sensitive aPTT (Activate Partial Thromboplastin Time).LA is a multistep procedure with screening, mixing and confirmation tests. Devreese et al recently concluded that integration of screening and confirmation in a single procedure and skipping the mixing tests result in a poor diagnostic efficacy for LA (2).LA is an in-vitro inhibitor and elevated Screening test without mixing studies does not prove inhibitor effect & it wastes time & resources to perform confirmatory tests skipping the mixing. Hence, we devised a new algorithm- Christian Medical College (CMC) Algorithm as shown in figure-1 which starts with DRVVT Screen Mix. To identify interferences due to anticoagulants like heparin and fibrin degradation products (FDP) thrombin time (TT) was also included. If Screen Mix is normal APTT Screen Mix was performed.
Aim of our new algorithm was to reduce false positives and avoid interferences in LA
Materials and methods: Four hundred and ninety-one (491) samples were analysed retrospectively for a period of 5 months from January 2022 to May 2022. The new algorithm was incorporated into STA R Max2 (Diagnostica Stago) analyser and automatic calculation of ratios and interpretation of results were done based on flow charts.
LA testing was performed using DRVVT screen and confirm reagents (STA-Staclot DRVV Screen and STA-Staclot DRVV Confirm) and/or APTT reagent (STA-PTT Synthasil).
LA test was considered positive when Screen/ Confirm(S/C) ratio was >1.2.
We compared this result to the three hundred forty seven(347) samples, over a period of 4 months(September 2021 - December 2021) analyzed in old algorithm where DRVVT screen & APTT were done as the initial steps instead of DRVVT mixing studies as the 1st step.
Results: In the new algorithm result were classified into 7 categories.
Category 1 had normal DRVVT screen Mix and normal APTT; these represent true negative cases comprising 68.8 % of the cases.
Category 2 had normal DRVVT screen Mix, prolonged APTT Screen Mix with normal TT. 1 case in this category had other Antiphosholipid Antibody (APLA) negative & repeat testing for LA was advised.
Category 3 had normal DRVVT Screen mix, prolonged APTT Screen Mix with prolonged TT. There was 1 case in this category, who was on heparin, APLA antibody was negative. Repeat testing was advised at a later date.
Category 4 had prolonged DRVVT Screen Mix, normal S/C ratio , with normal TT. There were 61 cases (12%) in this category among which 5 cases had normal DRVVT Screen with prolonged Mix
Category 5 had Prolonged DRVVT Screen Mix, with normal S/C Ratio, prolonged TT and this category had 13 (2 %) cases. On further evaluation they were found to be on anticoagulants.
Category 6 had prolonged S/C Ratio with normal TT, which are the true positive cases, n=67 (13.6%). There were 4 cases where Screen mix was more prolonged than Screen, and Screen fell below the cut off & could have been missed if mixing step was not done
Category 7 had prolonged S/C ratio with prolonged TT. There were 10 cases (2%) in this category. On further evaluation 6 patients had history of anticoagulants and 2 had features of DIC. These 8 patients could represent false positive LA and would have been misclassified if TT was not done.
Old algorithm had 20 % positive cases & 80 % negative cases.
Since the algorithm were incorporated into STA R Max2 hands on time decreased from 240 minutes to 80 minutes. Cost of the reagents were similar by 2 algorithms.
Conclusion: The new algorithm gives better clarity in classification of patients into true positive and true negative & detection of interference due to heparin as thrombin time is also done in parallel. Possible false positive cases could be identified at the onset even before repeat confirmatory lupus testing. This study concludes the importance of mixing studies in avoiding false negatives.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.