Introduction: The objective of this study is to establish a prediction system using circulating tumor DNA (ctDNA) to determine the effectiveness of CAR-T cell therapy in patients with relapsed or refractory B-cell non-Hodgkin lymphoma (R/R B-NHL). Furthermore, the study aims to compare the mutation characteristics between different therapeutic groups to provide guidance for the prevention and follow-up treatment of patients who fail CAR-T cell therapy.
Methods: In this part of the study, a total of 79 (192 serum samples) R/R B-NHL patients with CAR-T cell therapy were collected for ctDNA detection (187 lymphoma-related gene panel), including 62 samples before treatment (T0), 69 samples at 1 week (T1) and 62 samples at 4 weeks (T2) after reinfusion. Differences of categorical variables were tested using the chi-square test or Fisher's exact test, and differences in survival events between different groups were compared using Kaplan-Meier analysis and log-rank test.
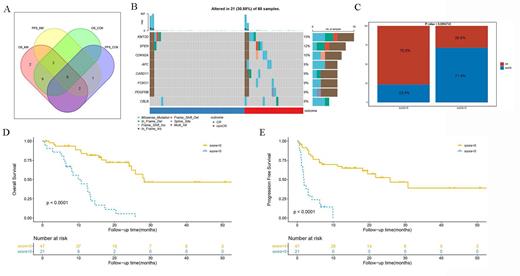
Results: The results of Kaplan-Meier analysis showed that patients with ctDNA mutation genes >10 before CAR-T cell therapy had poorer OS (1-year OS rate: 0% vs 74.9%, 2-year OS rate: 0% vs 68%, P<0.001) and PFS (1-year PFS rate: 0% vs 52.5%, 2-year PFS rate: 0% vs 36.6%, P=0.0056). Patients with MYD88, FAT1 and BTG2 mutation before CAR-T cell therapy had poorer OS, while patients with MUC16 mutation had better OS. The CR rate in patients with TP53 mutation before CAR-T cell treatment was significantly lower than that of patients without TP53 mutation (33.3% vs 68.1%, P=0.02). However, the TP53 mutation status before treatment did not have an impact on the long-term survival of patients. All patients with TP53 mutations at 4 weeks after CAR-T cell therapy failed to achieve CR, and OS was poorer (1-year OS rate: 37.5% vs 66.4%; 2-year OS rate: 12.5% vs 56.3%, P=0.0023). For CR patients, patients with BCR mutation at 4 weeks after treatment had poorer OS (2-year OS rate: 40.9% vs 76.1%, P=0.035). At one week after CAR-T cell therapy(Figure 1), patients without mutations of CDKN2A, CBLB, APC, SPEN, KMT2D, CARD11, FOXO1 and PDGFRB, were more likely to achieve CR (76.6% vs 28.6%, P<0.001), and had better OS (1-year OS rate: 81.5% vs 38.9%, 2-year OS rate: 62.2% vs 5%, P<0.001) and PFS (1-year PFS rate: 67.2% vs 0%, P<0.001).
Conclusions: In this study, we evaluated the characteristics of gene mutation between different therapeutic groups, and a gene set was screened to predict the efficacy of CAR-T cell therapy in R/R B-NHL patients, helping clinicians accurately evaluate the efficacy and assisting in decision-making of treatment options.
Disclosures
No relevant conflicts of interest to declare.