Abstract
Background:
Venetoclax(VEN) combination with hypomethylating agent(HMA) are lower-intensity regimens with safety which are widely used for older patients with newly diagnosed acute myeloid leukemia (AML). On the other hand, regimen of cytarabine, aclarubicin and G-CSF (CAG) with or without HMA is also of low-intensity usually applied to older AML patients. The comparison of outcomes of these two regimens has not been reported. In this study, we performed a multicenter, retrospective propensity score-matched study to compare the therapeutic responses and survival outcomes of newly diagnosed AML patients with induction of HMA-VEN to those with CAG based treatment.
Methods:
Newly diagnosed AML patients treated either VEN/HMA or CAG with or without HMA between January 2013 and April 2023 were compared. Age at diagnosis, sex, ECOG performance status, state of fitness for intensive chemotherapy according to Ferrara criteria and ELN2017 risk group were used to construct the propensity score using logistic regression. Propensity score matching was performed in a 1:1 ratio with a calliper value of 0.02. The treatment response, relapse rate, duration of remission, overall survival (OS) were compared between the two groups.
Results:
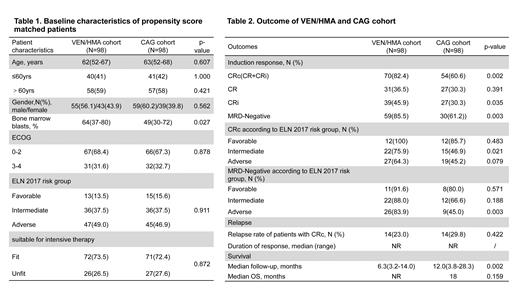
A total of 98 out of 109 newly diagnosed patients treated with VEN/HMA were matched to 98 out of 159 newly diagnosed patients treated with CAG based therapy. The patients in VEN/HMA cohort were treated between February 25, 2021 and April 30, 2023. The CAG based treatment recipients were treated from January 25, 2013 to November 12, 2021. The CAG based treatment cohort which was termed as “CAG cohort” below matched closely with the VEN/HMA cohort in terms of baseline characteristics and propensity scores (Table1). The median age was 62 years (range, 52-67) in VEN/HMA cohort and 63 years (range,52-68) in CAG cohort, and the median follow-up period was 6.3 months (range,3.2-14.0) in VEN/HMA cohort and 12 months (range,3.8-28.3) in CAG cohort.
Patients treated with VEN/HMA achieved a significantly higher rate of CRc (82.4% vs 60.6%, P=0.002) compared to CAG cohort, with 36.5% in CR, 45.9% in CRi in VEN/HMA cohort and 30.3% in CR, 30.3% in CRi in CAG cohort. There was no statistic difference of the CRc rate between CAG versus CAG plus HMA(35.7%,n=14 vs 60.5%,n=76, p=0.085). CRc in the VEN/HMA and CAG cohort were 100% vs 85.7(p=0.483), 75.9% vs 46.9%(p=0.021), 64.3% vs 45.2%(p=0.079) in the ELN2017 favorable, intermediate and adverse risk group, respectively. The MRD-negative remission rate was higher in VEN/HMA cohort compared to CAG cohort (85.5% vs 61.2%, p= 0.003). The MRD-negative remission rate in the VEN/HMA and CAG cohort were 91.6% vs 80.0%(p=0.571), 88.0% vs 66.6%(p=0.188), 83.9% vs 45%(p=0.003) in the ELN2017 favorable, intermediate and adverse risk group, respectively(Table2). Responses of patients with different mutations were analyzed and ASXL1 predicted higher CRc rate with VEN/HMA treatment compared to CAG based treatment (92.3% vs. 40%, p= 0.019).
The median OS was not reached in VEN/HMA cohort and 18 months in CAG cohort(p=0.16). Patients who achieved CRc had longer survival than those without CRc (not reached vs 6.4m, p<0.001). Patients who got MRD negative remission had better survival than those only with MRD positive remission (not reached vs 11.8m, p=0.0002). Patients who underwent allogeneic HSCT had longer survival than those didn't receive transplantation (not reached vs 12.3m, p<0.001).
Conclusions:
With propensity score-matched analysis, our data show that VEN/HMA demonstrates better treatment response than CAG regimen in patients with newly diagnosed AML. The survival outcome benefits from MRD negative response and allogeneic HSCT.
Disclosures No relevant conflicts of interest to declare.
Disclosures
No relevant conflicts of interest to declare.