Venous thromboembolism (VTE) is a common complication in cancer patients, which negatively affects treatment delivery and, consequently, prognosis. The pathophysiology of cancer‐associated thrombosis (CAT) is extremely complex, relying on cytokine release in response to interactions between tumor cells and macrophages, thus leading to endothelial damage and activation of coagulation. Several risk factors may contribute to VTE risk, including tumor types, advanced stage, and anti-cancer treatments. Anti-angiogenic agents or combination of systemic chemotherapy and concomitant radiotherapy (CT-RT), for instance, are well-established risk factors across different malignancies. Colorectal cancer (CRC) is not listed as a high-risk VTE tumor according to pivotal risk assessment models, although retrospective studies showed a VTE rate of around 20%. Consequently, considering the high prevalence of the disease, VTE in CRC represents a main burden in terms of morbidity, increased healthcare costs, and mortality. Rectal cancer (RC) comprises approximately 30% of all CRC. The treatment of locally advanced disease (LARC) consists of a multimodal approach which includes chemotherapy, radiotherapy, and surgery. In the context of CRC management, circulating tumor DNA (ctDNA) is a fast-growing tool able to detect minimal residual disease, useful for improving patients' stratification and prognosis. Moreover, its determination at the time of diagnosis may represent a surrogate of tumor burden, potentially increasing the risk of VTE compared to ctDNA negative patients. Due to the paucity of prospective data of VTE in LARC, the aim of this analysis is to describe the rate of VTE and the potential association between ctDNA levels at baseline and VTE occurrence.
We conducted a prospective observational study enrolling patients with LARC managed with neoadjuvant CT-RT (capecitabine 1650 mg/m2 concomitant with 50,4 Gy pelvic long course radiotherapy), surgery, plus/minus adjuvant chemotherapy at European Institute of Oncology (IEO) between November 2014 and November 2019. Blood samples for ctDNA were obtained at pre-planned timepoints: baseline (T0), end of CT-RT (T1), after surgery (T2), end of adjuvant chemotherapy (T3). ctDNA was extracted from plasma and mutations detected on tumor biopsy (KRAS, NRAS, BRAF, PIK3CA) were evaluated on ctDNA. Among other clinical information, VTE events were collected, including pulmonary embolism (PE), deep vein thrombosis (DVT) and visceral venous thrombosis (VVT). VTE was counted when occurred after or whitin 30 days before LARC diagnosis. The ctDNA value, defined as variant allele frequency (VAF) in a targeted mutation, was analyzed for correlation with clinical outcomes and VTE events. Median baseline ctDNA value was set as threshold to subdivide patients in VAF high and VAF low.
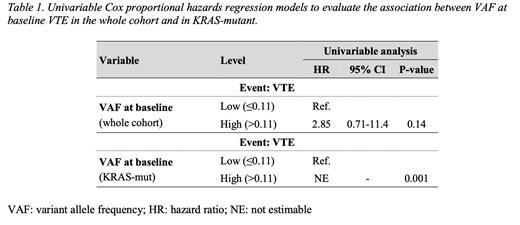
We enrolled 111 patients. Sixty-one (55%) patients harboring tumoral tissue mutations underwent liquid biopsy. KRAS mutation was the most frequent one (42%), followed by NRAS (7%) and PIK3CA (5%). Fifty-one patients (83%) had a clinical node positive disease. Baseline Khorana Score (KS) was 0 in 54 patients (88%) and 1 in 7. Median ctDNA value at T0 was 0.11 ng/2ml (range: 0.00 - 17.40). After a median follow up of 82 months, 9 VTE events (15%) were diagnosed, 4 PE, 3 DVT and 2 VVT. The median time from diagnosis to VTE event was 14 months (IQR 6 - 51). VTE occurrence was associated with VAF high at baseline, even though not statistically significant (Hazard Ratio [HR]: 2.85; 95% CI: 0.71-11.4, p value = 0.14). Looking specifically at KRAS mutant patients, 6 VTE events were observed, all experienced by VAF high patients (HR not estimable, p value = 0.001). Considering the overall population, VTE rate was 14% and no statistical differences were observed for VTE development according to mutational profile.
In our prospective study on LARC patients, VTE was associated with high levels of ctDNA at diagnosis, although not statistically significant. However, the association was significant in KRAS mutant tumors, which may represent a subset of patients with higher risk of thromboembolic complications. Prospective translational studies using deeper molecular techniques and wider populations are required to define the role of ctDNA as additional predictive tool to stratify VTE risk in cancer patients.
Disclosures
Cella:IPSEN: Research Funding; BMS: Consultancy; Leo Pharma: Honoraria. Spada:Novartis: Honoraria; Hutchinson MediPharma: Honoraria; AAA: Honoraria; Merck: Honoraria; Ipsen: Honoraria. Curigliano:Lilly: Honoraria, Speakers Bureau; Foundation Medicine: Honoraria, Speakers Bureau; Roche: Honoraria, Other: travel and accomodation, Speakers Bureau; Novartis: Honoraria, Speakers Bureau; Pfizer: Honoraria, Other: travel and accomodation, Speakers Bureau; Daiichi Sankyo: Honoraria, Speakers Bureau; Ellipses: Honoraria. Fazio:AAA: Honoraria; Hutchinson MediPharma: Honoraria; NUCANA: Other: Financial Institutional interest; IPSEN: Research Funding; Beigene: Other: Financial Institutional interest; FIBROGEN: Other: Financial Institutional interest; Incyte: Other: Financial Institutional interest; 4SC: Other: Financial Institutional interest; Merck: Honoraria; MSD: Other: Financial Institutional interest.