Venetoclax-based combination therapies have emerged as promising treatments for elderly acute myeloid leukemia (AML) patients. However, venetoclax resistance renders the treatment ineffective, mainly due to the upregulation of MCL1. Thus, new venetoclax-based combination therapy is under development to circumvent venetoclax resistance. The Ras-GTPase-activating protein SH3-domain binding protein 2 (G3BP2) is upgraded in several solid tumors. Targeting G3BP2 re-sensitized tumor cells to chemotherapy. To date, whether targeting G3BP2 sensitizes venetoclax treatment in AML and its role in leukemogenesis has not been defined.
To this end, the primary AML cells and AML cells were collected and cultured with compound C108 (G3BP2 inhibitor) and venetoclax alone or both. The result showed that co-culture with compound C108 and venetoclax decreased the cell viability in primary AML and AML cells, indicating the potent synergy of G3BP2 inhibitor and venetoclax. The Quantitative real-time PCR (RT-qPCR) showed that G3BP2 was overexpressed in AML patients and was associated with poor prognosis. Knockdown (KD) of G3BP2 decreased proliferation and induced apoptosis in AML cells. In addition, G3BP2 inhibition impeded the tumorigenicity in the subcutaneous AML xenograft tumor model. These data demonstrated that G3BP2 sensitized AML to venetoclax treatment and is critical in AML development.
The RNA-seq analysis was performed to investigate the role of G3BP2 in venetoclax resistance and leukemogenesis. The results showed that differentially expressed genes (DEG) were enriched in apoptotic processes when G3BP2 were downregulated. The immunoblotting results indicated that G3BP2 knockdown decreased the expression of MCL1 and BCL2, and vice versa. Moreover, we found that the transcription factor ELF1 was positively correlated with G3BP2 by the immunoblotting and RNA-seq analysis. The result was further validated by the Pearson correlation analysis based on the online database. The expression of ELF1 was decreased when G3BP2 were downregulated. Thus, we concluded that G3BP2 is an upstream gene of ELF1 and MCL1.
To further investigate the relationship among G3BP2, ELF1, and MCL1, the RNA binding protein immunoprecipitation assay (RIP) and mRNA stability analysis was performed. The results suggested that G3BP2 interacted with the ELF1 mRNA to enhance its stability. We employed bioinformatics analysis via the JASPAR database and RPISeq tools and found ELF1 may facilitate the transcription of MCL1, which was validated in the following study. The expression of MCL1 was restored in the G3BP2 KD cells when ELF1 was overexpressed. We subsequently performed CHIP-qPCR, dual-luciferase reporter gene assays with truncated MCL1 promoter fragments. A 576bp of the binding region upstream of MCL1 promoter was defined, indicating that ELF1 regulated MCL1 expression by modulating its transcription activity. Taken together, our data suggested that targeting G3BP2 decreases MCL1 expression by disturbing ELF1 mRNA stability, thus increasing the sensitivity to venetoclax treatment.
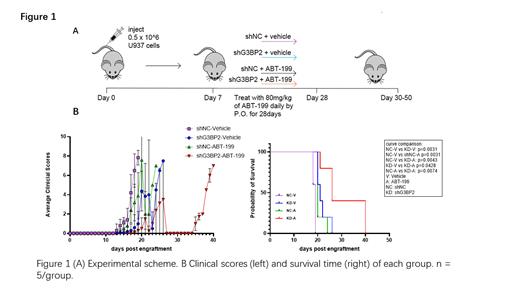
We finally established the intra-venous tumorigenesis xenograft model to verify the role of G3BP2 downregulation in venetoclax-treated leukemia mice. The NCG immunodeficient mice were transplanted with U937 cells and administrated with venetoclax daily from 7-21 days post transplantation (Figure 1A). The data showed that G3BP2 KD in combination with venetoclax reduced clinical scores and prolonged the overall survival of AML mice (combination vs. venetoclax: p<0.01; combination vs. G3BP2 KD: p<0.05, Figure 1B). The reduced leukemic burden was observed when targeting G3BP2 in combination with venetoclax. Meanwhile, we verified the decreased expression of ELF1 and MCL1 in mice targeting G3BP2 in combination with venetoclax by immunofluorescence (IF) and flow cytometry analysis. These data supported the synergic effect of G3BP2 inhibition and venetoclax treatment in AML.
Our findings emphasize the critical role of G3BP2 in conferring resistance to venetoclax in AML by stabilizing ELF1 mRNA to regulate MCL1 expression. Targeting G3BP2 represents an appealing therapeutic strategy for patients with venetoclax-resistant AML.
Disclosures
No relevant conflicts of interest to declare.