Background
Across Canadian Internal Medicine residency programs, a resident's clinical exposure to hematologic disorders is highly heterogeneous depending on the residency program's curriculum, ethnic diversity of the local patient population, and access to resources. Despite this variability in clinical exposure to hematology, there is a paucity of data assessing Internal Medicine residents' competence in the various subspecialties of hematology and whether they are fulfilling the Royal College of Physicians and Surgeons' expected competencies by the end of residency 1. Through this study, our primary aim was to assess Canadian Internal Medicine residents' perceptions of their hematology training to identify gaps in hematology education in residency curricula.
Methods
We administered a cross-sectional survey using REDCap to all Internal Medicine residents (PGY1 to PGY5) from participating sites across Canada. The survey was distributed to residents electronically by email. To increase response rates, the survey was distributed three times (every 2 weeks) over a 6-week period. An incentive ($10 Starbucks gift card) was provided to improve response rates.
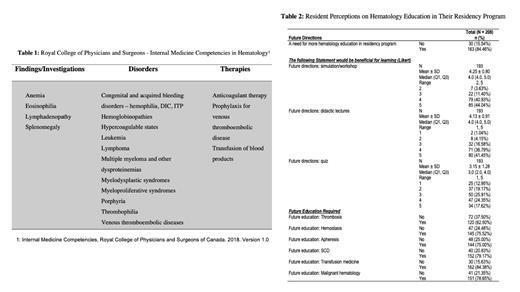
The survey questions were designed based on the Royal College objectives which outline expected competencies by the end of Internal Medicine residency (Table 1). It consisted of 16 questions assessing 4 domains: respondent demographics, competence in diagnosis and management of specific hematologic disorders, competence in management of hematologic emergencies, and resident perceptions on hematology education in their program. Survey responses were anonymous and consisted of a combination of dichotomous (yes/no) and ordinal variables (Likert scale). The study was approved by the University of Toronto Research and Ethics Board (REB).
Generalized linear regression analysis was used to compare survey questions between residents in different subgroups. p<0.05 was considered statistically significant. Least square mean (LSM) difference (with standard error SE) and 95% confidence intervals (CI) were calculated, with positive LSM indicating a higher Likert score.
Results
Of the 17 Internal Medicine programs that were invited to participate, 13 programs participated in the survey. 208 residents responded, with 92.31% (192/208) complete responses and 7.69% (16/208) incomplete responses. The overall response rate was 15.02% (208/1,385), with breakdown as follows: 31.5% (436/1,385) PGY1s, 30.5% (423/1,385) PGY2s, 30.9% (428/1,385) PGY3s, 4.5% (62/1,385) PGY4s, and 1.6% (22/1,385) PGY5s.
84.46% (163/208) of residents felt that there was a need for more hematology education in their residency program (Table 2). Specifically, residents felt that there was a need for more education in thrombosis (62.5%, 120/208), hemostasis (75.5%, 145/208), apheresis (75.0%, 144/208), sickle cell disease (79.2%, 152/208), transfusion medicine (84.4%, 162/208), and malignant hematology (78.7%, 151/208). A simulation/workshop was rated to be the most beneficial intervention (mean score of 4.25 +/- 0.80 on Likert scale) for learning.
Conclusion
Based on a cross-national survey of Internal Medicine residents in Canada, there are significant gaps in hematology education in Canadian Internal Medicine residency programs, most pronounced in transfusion medicine, sickle cell disease, and hemostasis. Interventions targeting these gaps should be designed to improve competence in the diagnosis and management of hematologic disorders and emergencies.
References
1. Internal Medicine Competencies, Royal College of Physicians and Surgeons of Canada. 2018. Version 1.0.
Disclosures
Patriquin:Alexion, AstraZeneca Rare Disease: Consultancy, Honoraria, Other: clinical site investigator, Speakers Bureau; Apellis: Consultancy, Honoraria, Other: clinical site investigator, Speakers Bureau; Regeneron: Other: clinical site investigator; Takeda: Consultancy, Honoraria, Speakers Bureau; BioCryst: Consultancy, Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau.