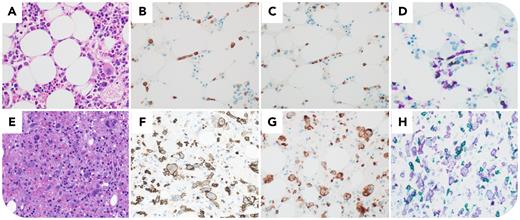
A 71-year-old man with rheumatoid arthritis presented with severe neutropenia (0.01 × 109/L), relative lymphocytosis (2.4 × 109/L), and mild splenomegaly. Bone marrow biopsy was normocellular (panel A) with 15% infiltration by bland αβ T cells expressing CD2, CD3, CD8 (panel B), CD16, granzyme B, and TIA1 (panel C), with aberrant CD5 and CD7 loss and intrasinusoidal distribution. CD3 (purple)/TRBC1 (green) dual-stain (panel D) revealed the intrasinusoidal T cells were CD3+/TRBC1–-restricted (purple only), indicative of clonality, in contrast to the polytypic background including both CD3+/TRBC1+ (evergreen) and CD3+/TRBC1– (purple) T cells. Next-generation sequencing identified STAT3, TET2, and PPM1D mutations, supporting T-large granular lymphocytic leukemia (T-LGLL). Methotrexate and prednisone were initially effective, but after 2 years he developed malaise and severe pancytopenia. Bone marrow biopsy showed extensive large lymphocytic infiltrate with irregular nuclei and prominent nucleoli (panel E), sharing immunophenotypic features with prior T-LGLL: CD2+, CD3+, CD8+ (panel F), granzyme B+, TIA1+ (panel G), CD5–, CD7–, and CD3+/TRBC1– on dual-stain (panel H); and also CD30+. An objective magnification of 40× was used for all images. Clonal T-cell receptor gene rearrangement peaks and genetic mutations were identical to those of prior T-LGLL, confirming the same T-cell clone. The patient responded to brentuximab vedotin, cyclophosphamide, doxorubicin, and prednisone.
This case details an extremely rare transformation of indolent T-LGLL to aggressive peripheral T-cell lymphoma. A novel CD3/TRBC1 dual-stain provided support for shared clonality.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.