Abstract
We have recently shown that more than 90% of long-term culture initiating cells (LTC-IC) mobilized in the peripheral blood (PB) of normal individuals express HLA-DR and CD38 antigens and can sustain hematopoiesis for only 5 weeks. However, 10% of LTC-IC in mobilized PB are CD34+HLA-DR− and CD34+CD38− and can sustain hematopoiesis for at least 8 weeks. We now examine the ex vivo expansion potential of CD34+HLA-DR+ cells (rich in mature LTC-IC) and CD34+HLA-DR− cells (rich in primitive LTC-IC) in granulocyte colony-stimulating factor (G-CSF ) mobilized PB progenitor cells (PBPC). Cells were cultured in contact with M2-10B4 cells (contact) or in transwells above M2-10B4 (noncontact) without and with interleukin-3 (IL-3) and macrophage inflammatory protein (MIP-1α) for 2 and 5 weeks. Progeny were evaluated for the presence of colony-forming cells (CFC) and LTC-IC. When CD34+HLA-DR+ PB cells were cultured in contact cultures without cytokines, a threefold expansion of CFC was seen at 2 weeks, but an 80% decrease in CFC was seen at week 5. Further, the recovery of LTC-IC at week 2 was only 17% and 1% at week 5. This confirms our previous observation that although CD34+HLA-DR+ mobilized PB cells can initiate long-term cultures, they are relatively mature and cannot sustain long-term hematopoiesis. In contrast, when CD34+HLA-DR− mobilized PB cells were cultured in contact cultures without cytokines, CFC expansion persisted until week 5 and 49% and 11% of LTC-IC were recovered at week 2 and 5, respectively. As we have shown for steady state bone marrow (BM) progenitors, recovery of LTC-IC was threefold higher when CD34+HLA-DR− PBPC were cultured in noncontact rather than contact cultures, and improved further when IL-3 and MIP-1α were added to noncontact cultures (96 ± 2% maintained at week 5). We conclude that although G-CSF mobilizes a large population of “mature” CD34+HLA-DR+ LTC-IC with a limited proliferative capacity, primitive CD34+HLA-DR− LTC-IC present in mobilized PB have similar characteristics as LTC-IC from steady state BM: (1) they can be maintained in noncontact cultures containing IL-3 and MIP-1α for at least 5 weeks; (2) they are subject to the same proliferation inhibitory influences of contact with stroma. Since the absolute number of primitive LTC-IC (week 8 LTC-IC) per mL of G-CSF mobilized PB is similar to that per mL of steady state BM, these studies further confirm that G-CSF mobilized PBPC may have similar long-term repopulating abilities as steady state BM.
THE OBSERVATION that primitive hematopoietic progenitors capable of providing complete and sustained hematopoietic reconstitution in myeloablated hosts are present in the peripheral blood (PB) has led to the exponential use of peripheral blood progenitor cells (PBPC) in autologous and allogeneic transplants.1-9 Numerous studies have characterized PB CD34+ cells present in mobilized PB.10-12 PB CD34+ cells express less c-kit and CD71, but more HLA-DR antigens and PB CD34+ cells retain less rhodamine than BM CD34+ cells. This suggests that the majority of mobilized CD34+ cells may represent a more mature category in the hierarchy of hematopoietic stem cells.11,12 We have recently shown that granulocyte colony-stimulating factor (G-CSF ) mobilized PBPC are particularly enriched in long-term culture initiating cells (LTC-ICs) with a limited proliferative potential.13 These LTC-IC are found in the CD34+HLA-DR+ and CD34+CD38+ subpopulation of PBPC and can sustain hematopoiesis in long-term culture for 5 weeks but not for more prolonged periods of time. These studies further indicate that although mobilized PBPC contain primitive progenitors, the majority of these progenitors are more mature than those commonly found in steady state bone marrow (BM). However, 10 ± 2% of CD34+ cells in mobilized PBPC are HLA-DR− and 9 ± 2% of CD34+ cells in mobilized PBPC are CD38−.13 In contrast to mobilized CD34+HLA-DR+ and CD34+CD38+ LTC-IC, CD34+HLA-DR− and CD34+CD38− LTC-IC present in PBPC, like CD34+HLA-DR− and CD34+CD38− LTC-IC in steady state marrow, can support hematopoiesis in LTC for 8 weeks. CD34+HLA-DR− and CD34+CD38− PBPC may thus contain cells responsible for sustained engraftment.13
Although transplantation of mobilized PBPC usually results in early engraftment, patients remain neutropenic for 7 to 15 days.4 Furthermore, collection of sufficient progenitors may be difficult in patients with acute myelogenous leukemia and some patients previously treated with chemotherapy and/or radiation therapy.14 These are some of the reasons for contemplating ex vivo culture of PBPC to increase both the number of mature progenitors and primitive long-term repopulating progenitors.
A number of ex vivo culture systems that can expand/maintain primitive and committed progenitors have been described. “Dexter” type stroma-dependent culture systems can support maintenance and proliferation of murine hematopoietic stem cells, without exogenous added cytokines.15,16 However, although similar cultures in which human hematopoietic progenitors are cultured in contact with a stromal feeder can support initial expansion of colony-forming cells (CFC) and LTC-IC when exogenous cytokines are added,17 less than 20% of LTC-IC can be maintained in contact-cultures for periods exceeding 2 weeks.18,19 We have previously shown that this is caused by failure of the small fraction of conserved LTC-IC to proliferate, at least in part due to adhesive interactions between progenitors and stromal extracellular matrix components.20 In a second type of ex vivo culture system, hematopoietic progenitors are cultured in the absence of a stromal layer but in the presence of repeatedly added defined cytokines including G-CSF, interleukin-3 (IL-3), IL-6, stem cell factor (SCF ), and Flt-3 ligand. A number of studies have shown that these culture conditions can greatly expand committed progenitors present in BM, mobilized PBPC and other sources of stem cells.21-26 Furthermore, recent studies have suggested that under these conditions LTC-IC present in steady state BM may be expanded up to 50-fold after 2 to 3 weeks.27 However, it is unclear if these conditions can also maintain LTC-IC for more protracted periods of time.28,29 Recently, we have described a third culture system in which progenitors are cultured with a stromal feeder, but separated from the feeder by an 0.4-μm filter membrane, also termed “stroma-noncontact” culture system.18 We have shown that steady state BM derived LTC-IC can be expanded fivefold during the first 2 weeks of culture and can be maintained for at least 8 weeks when noncontact cultures are supplemented with the growth promoting cytokine IL-3 and the growth inhibitory cytokine macrophage inflammatory protein (MIP-1α), while generation of CFC is allowed. The observation that 100% of LTC-IC can be maintained in a noncontact system, but not when cultured in Dexter-type contact-cultures, is thought to be due to the absence of progenitor-stroma interactions in the noncontact system, which allows significantly more proliferation of LTC-IC.20
In the current study, we examined the ex vivo expansion potential of CFC and LTC-IC present in CD34+ subpopulations of G-CSF mobilized PBPC. We show that progenitors present in the PB CD34+HLA-DR+ subpopulation cannot be expanded nor maintained ex vivo, consistent with the notion that although PB CD34+HLA-DR+ cells may contain a large population of LTC-IC, these LTC-IC are more mature than those in BM or PB CD34+HLA-DR− cells. However, similar to what we have described for LTC-IC present in steady state BM CD34+HLA-DR− cells, LTC-IC present in mobilized PB CD34+HLA-DR− cells can be maintained for 5 weeks ex vivo when cultured in noncontact cultures containing IL-3 and MIP-1α. Of note, significantly less CD34+HLA-DR− LTC-IC present in PBPC are expanded/maintained when cultured in contact with stroma. This suggests that, as for steady state BM LTC-IC, mobilized PB CD34+HLA-DR− LTC-IC are subject to the same proliferation inhibitory signals resulting from contact with stromal components. This indicates that CD34+HLA-DR− LTC-IC present in G-CSF mobilized PBPC have the same functional characteristics as LTC-IC present in steady state BM.
MATERIALS AND METHODS
Samples
Normal healthy donors were selected using standard criteria of the American Association of Blood Banks for blood donors.30 Informed consent was obtained using guidelines approved by the Committee on the Use of Human Subjects for Research at the University of Minnesota (Minneapolis). All donors had a negative serologic test for HBsAg, anti-hepatitis-C virus (HCV) and anti-human immunodeficiency virus (HIV) and they had normal hemoglobin, white blood cell (WBC) counts, white cell differentials, and platelet counts. Normal donors received a daily dose of 10 μg/kg/d of human recombinant G-CSF (Neupogen; Amgen, Inc, Thousand Oaks, CA) subcutaneously for 5 days (day 1 through 5). G-CSF was given as a single morning dose. Sixty milliliters of blood were obtained by venipuncture from each donor before the first injection of G-CSF (day 0) and on day +6. In addition BM was obtained before the first injection of G-CSF.
Evaluation of Samples
Cell Selection
Steady state BM and G-CSF mobilized PB mononuclear cells (MNC) were separated by Ficoll Hypaque centrifugation (specific gravity, 1077) (Sigma Chemical Co, St Louis, MO). CD34 enrichment was done using the MACS CD34 Isolation Kit (Miltenyi Biotec Inc, Sunnyvale, CA) according to the manufacturer's instructions with modifications. Briefly, MNC cells were suspended in cold phosphate-buffered saline (PBS) and 0.3% bovine serum albumin (BSA) and incubated with modified CD34 antibody (QBEND/10, mouse IgG1) for 15′ at 4°C, washed and incubated for 15′ with superparamagnetic MACS microbeads recognizing anti-CD34 antibodies. Concurrently, the separation column was flushed with cold PBS and positioned in the MACS magnetic field. The cell suspension was loaded onto the separation column and nonadherent cells collected. The CD34+ cells that were retained in the column were then recovered by removing the column from the magnetic field and flushing with buffer. The magnetic separation step was repeated once to obtain a CD34+ cell purity more than 90% in every sample.
Fluorescence-Activated Cell Sorting (FACS)
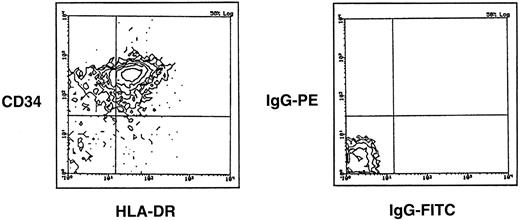
For FACS selection, CD34 enriched cells were labeled with phycoerythrin (PE)-conjugated mouse anti-CD34 antibodies and fluorescein isothiocyanate (FITC)-conjugated mouse anti-HLA-DR antibodies (1 μg/106 cells) (Becton Dickinson, San Jose, CA), incubated for 30′ on ice then washed with cold PBS. Cells were selected on a FACStar-Plus laser flow cytometry system equipped with a CONSORT 32 computer for low forward and side scatter properties and expression of CD34 and HLA-DR antigens using mouse IgG1-PE and IgG2-FITC antibodies as control. Figure 1 includes a sample of gates established for FACS selection.
Representative FACS analysis of mobilized PBPC. Depicted are the gates established for FACS selection as well as the negative controls for mobilized PBPC.
Representative FACS analysis of mobilized PBPC. Depicted are the gates established for FACS selection as well as the negative controls for mobilized PBPC.
BM and PB Cultures
Complete long-term culture (LTC) medium.This consisted of Iscove's modified Dulbecco's medium (IMDM; GIBCO Laboratories, Grand Island, NY) with 12.5% fetal calf serum (FCS; Hyclone, Logan, UT), 12.5% horse serum (Terry Fox Laboratories, Vancouver, Canada), 2 mmol/L glutamine (GIBCO), penicillin 100 U/mL, streptomycin 100 U/mL (GIBCO), and 10−6 mol/L hydrocortisone.31
Stromal feeders.M2-10B4 cells (generous gift from Dr C Eaves, Vancouver, British Columbia, Canada), are mouse BM fibroblasts that can support growth of human CFC and LTC-IC in contact and noncontact cultures to the same extent as normal human BM stromal feeders.32 33 M2-10B4 cells were subcultured in wells of 6-well or 96-well plates. Once confluent, plates were irradiated with 6,000 cGy and the medium was changed to LTC medium.
Contact culture.Confluent M2-10B4 stromal layers, subcultured in 6-well plates, were irradiated and CD34+HLA-DR+ or CD34+HLADR− cells were plated in direct contact with the M2-10B4 feeders. Cultures were maintained for 2 or 5 weeks in LTC medium with or without cytokines.
Noncontact culture.Confluent M2-10B4 layers, subcultured in 6-well plates, were irradiated. A collagen-treated transwell insert (0.4-μm microporous filter) (Costar Corp, Cambridge, MA) was placed above the M2-10B4 feeder and CD34+HLA-DR− cells were plated in the upper wells for 2 or 5 weeks in LTC medium with or without cytokines.
Maintenance of expansion cultures.All cultures were maintained in a humidified atmosphere at 37°C and 5% CO2. At weekly intervals contact and noncontact cultures were fed by removing half of the cell-free supernatant and replacing it with fresh LTC medium with or without cytokines.
Evaluation of expansion cultures.After 2 or 5 weeks, adherent and nonadherent cells were recovered from contact cultures by short-term trypsinization and replated in short-term methylcellulose culture and in LTC in limiting dilutions. Cells from noncontact cultures were recovered at week 2 or 5 by thoroughly washing the transwells with PBS, and cells replated in short- and long-term culture.18,29 33
Cytokines.In some experiments recombinant human (rHu) IL-3 (Genetics Institute, Cambridge, MA) and rHuMIP-1α (R&D Systems, Inc, Minneapolis, MN) were added to the cultures three times per week to obtain a final concentration of 5 ng/mL and 100 ng/mL, respectively.29
Short-term methylcellulose progenitor culture.Two thousand CD34+HLA-DR+ or CD34+HLA-DR− cells or the progeny of 2,000 CD34+HLA-DR+ or CD34+HLA-DR− cells recovered from expansion cultures were plated in methylcellulose containing IMDM supplemented with 30% FCS, 3 IU erythropoietin (Epoietin, EPO; Amgen) and 10% supernatant of the carcinoma cell line 5637 as described.34 Cultures were incubated in a humidified atmosphere at 37°C and 5% CO2. The cultures were assessed at day 14 to 18 for the presence of BFU-E, CFU-GM, and CFU-Mix as previously described.34
Enumeration of LTC-ICs by limiting dilution assays (LDAs).Ten thousand CD34+HLA-DR+ or CD34+HLA-DR− cells or progeny of 10,000 CD34+HLA-DR+ or CD34+HLA-DR− cells recovered from expansion cultures (22 replicates: 300, 100, 33, 11 cells/well day 0) were plated in limiting dilutions onto previously irradiated M2-10B4 feeders in 96-well plates. Cultures were maintained in a humidified atmosphere at 37°C and 5% CO2. Weekly, half of the medium was replaced by fresh LTC medium. After 5 weeks, unless otherwise stated, all media were removed and the feeders overlaid with methylcellulose containing medium supplemented with EPO (3 IU/mL) and 10% supernatant of the bladder carcinoma cell line, 5637. Wells were scored for the presence or absence of secondary CFC on day 14. The absolute number of LTC-IC present in the different cell populations was calculated as the reciprocal of the concentration of test cells that gives 37% negative cultures using Poisson statistics.18 35
Statistics.Results of experimental points obtained from multiple experiments were reported as the mean ± SEM. Significance levels were determined by two-sided Student's t-test.
RESULTS
Consistent with our previous studies13 significantly more CD34+HLA-DR+ cells present in G-CSF mobilized PBPC could initiate and sustain hematopoiesis for 5 weeks in long-term culture than CD34+HLA-DR− cells (week 5 LTC-IC: 1,245 ± 230/105 CD34+HLA-DR+ cells v 461 ± 240/105 CD34+HLA-DR− cells; P < .01). However, when the cultures were examined after 8 weeks, more CD34+HLA-DR− cells sustained hematopoiesis than CD34+HLA-DR+ cells (week 8 LTC-IC: 98 ± 83/105 CD34+HLA-DR+ cells v 149 ± 38/105 CD34+HLA-DR− cells). This confirms that LTC-IC present in CD34+HLA-DR+ cells may be more mature than those present in CD34+HLA-DR− cells. We then calculated the absolute number of primitive LTC-IC (week 8 LTC-IC) present in CD34+HLA-DR− cells per mL of mobilized PB or steady state BM (number of week 8 LTC-IC per 105 MNC × number of MNC per mL of BM or PB). Forty-two ± 14 week 8 LTC-IC were present per mL of mobilized PB while 60 ± 20 week 8 LTC-IC were present in 1 mL of steady state BM. These differences were not significant.
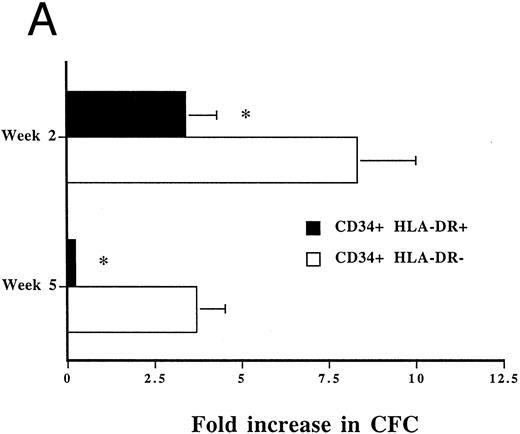
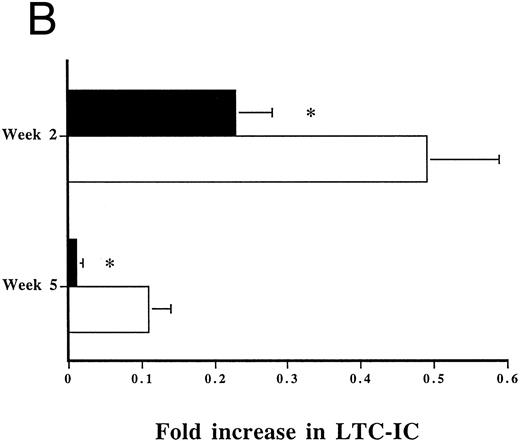
We cultured mobilized PB CD34+HLA-DR+ and CD34+ HLA-DR− cells for 2 and 5 weeks in contact with M2-10B4 feeders without exogenous cytokines and examined their progeny for the presence of CFC and LTC-IC. When CD34+HLA-DR+ cells were cultured for 2 weeks in contact with M2-10B4, a 3.4 ± 0.9-fold expansion in CFC was observed (Fig 2A). However, after 5 weeks of culture only 20 ± 10% of CFC present on day 0 in freshly sorted CD34+HLA-DR+ cells were still present (Fig 2A). Furthermore, when we examined the number of LTC-IC still present after 2 and 5 weeks of culture, we found that the recovery was only 23 ± 5% and 1 ± 1% of day 0 LTC-IC after 2 and 5 weeks of culture, respectively (Fig 2B). Lack of expansion of CFC at 5 weeks and lack of maintenance of LTC-IC both at 2 and 5 weeks in cultures initiated with mobilized PB derived CD34+ HLA-DR+ cells confirms that PB derived CD34+HLA-DR+ cells contain mainly progenitors at an intermediate stage of differentiation. In contrast to mobilized PB CD34+HLA-DR+ cells, when mobilized PB CD34+HLA-DR− cells were cultured for 2 and 5 weeks in contact with M2-10B4, an 8.3 ± 1.7-fold and 3.7 ± 0.8-fold expansion of CFC was seen after 2 and 5 weeks, respectively (Fig 2A). Further, 49 ± 10% and 11 ± 3% of LTC-IC were maintained for 2 and 5 weeks, respectively, in contact cultures initiated with PBPC CD34+HLA-DR− cells (Fig 2B). Thus, expansion/maintenance of CFC and LTC-IC was significantly better in cultures initiated with PB CD34+HLA-DR− than in cultures initiated with PB CD34+HLA-DR+ cells. Results for mobilized PB CD34+HLA-DR− cells are similar to what we have previously reported for LTC-IC rich populations present in steady state BM.18 33
Expansion of CFC (A) and LTC-IC (B) in M2-10B4 contact cultures initiated with PB CD34+HLA-DR+ (n = 6) and CD34+HLA-DR− (CFC n = 10; LTC-IC n = 9) cells. Twelve thousand CD34+HLA-DR+ or CD34+HLA-DR− cells were cultured for 2 to 5 weeks in LTC medium without cytokines in contact with irradiated M2-10B4 feeders. Cells were collected at 2 and 5 weeks and 1/6 of the progeny was replated in methylcellulose assay to enumerate the number of CFC (equivalent of 2,000 day 0 cells) and 5/6 of the progeny in LDA onto M2-10B4 feeders (equivalent of 10,000 day 0 cells) for 5 weeks to enumerate the number of LTC-IC. The number of CFC present at 2 and 5 weeks was divided by the number of CFC per 2,000 freshly sorted cells to calculate CFC expansion. The number of LTC-IC at 2 and 5 weeks was divided by the number of LTC-IC in freshly sorted cells to calculate LTC-IC expansion. Results represent mean ± SEM. (A) The number of CFC on day 0 was 482 ± 45 CFC/2,000 CD34+HLA-DR+ cells and 52 ± 15 CFC/2,000 CD34+HLA-DR− cells; *P < .01 comparison between CFC expansion in cultures initiated with CD34+HLA-DR+ and CD34+HLA-DR− cells. (B) The absolute number of LTC-IC on day 0 was 124 ± 23 LTC-IC/10,000 CD34+HLA-DR+ cells and 46 ± 24 LTC-IC/10,000 CD34+HLA-DR− cells; *P < .01 comparison between LTC-IC maintenance in cultures initiated with CD34+HLA-DR+ and CD34+HLA-DR− cells.
Expansion of CFC (A) and LTC-IC (B) in M2-10B4 contact cultures initiated with PB CD34+HLA-DR+ (n = 6) and CD34+HLA-DR− (CFC n = 10; LTC-IC n = 9) cells. Twelve thousand CD34+HLA-DR+ or CD34+HLA-DR− cells were cultured for 2 to 5 weeks in LTC medium without cytokines in contact with irradiated M2-10B4 feeders. Cells were collected at 2 and 5 weeks and 1/6 of the progeny was replated in methylcellulose assay to enumerate the number of CFC (equivalent of 2,000 day 0 cells) and 5/6 of the progeny in LDA onto M2-10B4 feeders (equivalent of 10,000 day 0 cells) for 5 weeks to enumerate the number of LTC-IC. The number of CFC present at 2 and 5 weeks was divided by the number of CFC per 2,000 freshly sorted cells to calculate CFC expansion. The number of LTC-IC at 2 and 5 weeks was divided by the number of LTC-IC in freshly sorted cells to calculate LTC-IC expansion. Results represent mean ± SEM. (A) The number of CFC on day 0 was 482 ± 45 CFC/2,000 CD34+HLA-DR+ cells and 52 ± 15 CFC/2,000 CD34+HLA-DR− cells; *P < .01 comparison between CFC expansion in cultures initiated with CD34+HLA-DR+ and CD34+HLA-DR− cells. (B) The absolute number of LTC-IC on day 0 was 124 ± 23 LTC-IC/10,000 CD34+HLA-DR+ cells and 46 ± 24 LTC-IC/10,000 CD34+HLA-DR− cells; *P < .01 comparison between LTC-IC maintenance in cultures initiated with CD34+HLA-DR+ and CD34+HLA-DR− cells.
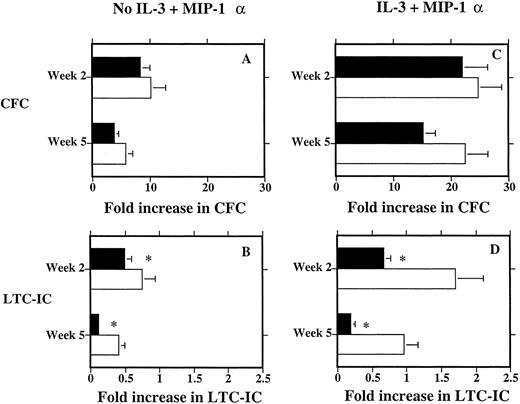
Mobilized PB CD34+HLA-DR− cells were also cultured in transwells above M2-10B4 feeders. We have previously reported that maintenance of steady state BM LTC-IC is significantly better when BM derived CD34+HLA-DR− cells are cultured separately from stromal feeders than when cultured in direct contact with stroma.18 33 We show here that maintenance of LTC-IC present in mobilized PB CD34+HLA-DR− cells was significantly better in noncontact (41 ± 8% maintenance at week 5) than in contact cultures (11 ± 3% maintenance at week 5, P < .05) (Fig 3B). Although expansion of CFC in contact cultures was somewhat lower than in noncontact cultures both at 2 and 5 weeks, these differences were not statistically significant (Fig 3A).
Expansion of CD34+HLA-DR− CFC (A) and LTC-IC (B) in contact and noncontact cultures without cytokines and with the addition of IL-3 and MIP-1α (C and D). Twelve thousand CD34+HLA-DR− cells were cultured for 2 to 5 weeks in LTC medium without cytokines or with the addition of IL-3 and MIP-1α (3 times per week to a final concentration of 5 ng/mL and 100 ng/mL, respectively) in contact with irradiated M2-10B4 feeders or in transwells above M2-10B4. Cells were collected after 2 and 5 weeks and 1/6 of the progeny replated in methylcellulose assay to enumerate the number of CFC (equivalent of 2,000 day 0 cells) and 5/6 of the progeny in LDA onto M2-10B4 feeders (equivalent of 10,000 day 0 cells) for 5 weeks to enumerate the number of LTC-IC. The number of CFC present at 2 and 5 weeks was divided by the number of CFC per 2,000 freshly sorted cells to calculate CFC expansion. The number of LTC-IC at 2 and 5 weeks was divided by the number of LTC-IC in freshly sorted cells to calculate LTC-IC expansion. Results represent mean ± SEM (CFC n = 10; LTC-IC n = 9). Closed bars represent contact cultures; open bars represent noncontact cultures. The number of CFC in freshly selected CD34+HLA-DR− cells was 52 ± 15 CFC/2,000 CD34+HLA-DR− cells. The number of LTC-IC in freshly selected CD34+HLA-DR− cells was 46 ± 24 LTC-IC/10,000 CD34+HLA-DR− cells. (A) Comparison between CFC expansion in contact and noncontact cultures; the number of CFC after 5 weeks in contact culture was 176 ± 53 CFC/2,000 day 0 CD34+HLA-DR− and 218 ± 52 CFC/2,000 day 0 CD34+HLA-DR− in noncontact culture; differences not significant. (B) Comparison between LTC-IC maintenance in contact and noncontact cultures without cytokines; the number of LTC-IC after 5 weeks in contact culture was 4.6 ± 1.6 LTC-IC/10,000 day 0 CD34+HLA-DR− and 16.8 ± 4.7 LTC-IC/10,000 day 0 CD34+HLA-DR− in noncontact culture; * P < .01. (C) Comparison between CFC expansion in contact and noncontact cultures supplemented with IL-3 and MIP-1α; the number of CFC after 5 weeks in contact culture supplemented with cytokines was 770 ± 152 CFC/2,000 day 0 CD34+HLA-DR− and 981 ± 159 CFC/2,000 day 0 CD34+HLA-DR− in cytokine supplemented noncontact culture; differences not significant. (D) Comparison between LTC-IC maintenance in contact and noncontact cultures supplemented with IL-3 and MIP-1α; the number of LTC-IC after 5 weeks in contact culture supplemented with cytokines was 7.5 ± 2.9 LTC-IC/10,000 day 0 CD34+HLA-DR− and 42.1 ± 8.9 LTC-IC/10,000 day 0 CD34+HLA-DR− in noncontact culture; * P < .01.
Expansion of CD34+HLA-DR− CFC (A) and LTC-IC (B) in contact and noncontact cultures without cytokines and with the addition of IL-3 and MIP-1α (C and D). Twelve thousand CD34+HLA-DR− cells were cultured for 2 to 5 weeks in LTC medium without cytokines or with the addition of IL-3 and MIP-1α (3 times per week to a final concentration of 5 ng/mL and 100 ng/mL, respectively) in contact with irradiated M2-10B4 feeders or in transwells above M2-10B4. Cells were collected after 2 and 5 weeks and 1/6 of the progeny replated in methylcellulose assay to enumerate the number of CFC (equivalent of 2,000 day 0 cells) and 5/6 of the progeny in LDA onto M2-10B4 feeders (equivalent of 10,000 day 0 cells) for 5 weeks to enumerate the number of LTC-IC. The number of CFC present at 2 and 5 weeks was divided by the number of CFC per 2,000 freshly sorted cells to calculate CFC expansion. The number of LTC-IC at 2 and 5 weeks was divided by the number of LTC-IC in freshly sorted cells to calculate LTC-IC expansion. Results represent mean ± SEM (CFC n = 10; LTC-IC n = 9). Closed bars represent contact cultures; open bars represent noncontact cultures. The number of CFC in freshly selected CD34+HLA-DR− cells was 52 ± 15 CFC/2,000 CD34+HLA-DR− cells. The number of LTC-IC in freshly selected CD34+HLA-DR− cells was 46 ± 24 LTC-IC/10,000 CD34+HLA-DR− cells. (A) Comparison between CFC expansion in contact and noncontact cultures; the number of CFC after 5 weeks in contact culture was 176 ± 53 CFC/2,000 day 0 CD34+HLA-DR− and 218 ± 52 CFC/2,000 day 0 CD34+HLA-DR− in noncontact culture; differences not significant. (B) Comparison between LTC-IC maintenance in contact and noncontact cultures without cytokines; the number of LTC-IC after 5 weeks in contact culture was 4.6 ± 1.6 LTC-IC/10,000 day 0 CD34+HLA-DR− and 16.8 ± 4.7 LTC-IC/10,000 day 0 CD34+HLA-DR− in noncontact culture; * P < .01. (C) Comparison between CFC expansion in contact and noncontact cultures supplemented with IL-3 and MIP-1α; the number of CFC after 5 weeks in contact culture supplemented with cytokines was 770 ± 152 CFC/2,000 day 0 CD34+HLA-DR− and 981 ± 159 CFC/2,000 day 0 CD34+HLA-DR− in cytokine supplemented noncontact culture; differences not significant. (D) Comparison between LTC-IC maintenance in contact and noncontact cultures supplemented with IL-3 and MIP-1α; the number of LTC-IC after 5 weeks in contact culture supplemented with cytokines was 7.5 ± 2.9 LTC-IC/10,000 day 0 CD34+HLA-DR− and 42.1 ± 8.9 LTC-IC/10,000 day 0 CD34+HLA-DR− in noncontact culture; * P < .01.
Finally, we cultured mobilized PB CD34+HLA-DR− cells in contact or non-contact cultures supplemented with IL-3 + MIP-1α. Addition of IL-3 + MIP-1α 3 times per week to noncontact cultures initiated with CD34+HLA-DR− cells significantly increased CFC expansion both at 2 (24.6 ± 5.1-fold v 10.1 ± 2-fold for cultures with and without IL-3 + MIP-1α, respectively; P < .01) and 5 weeks (22.4 ± 3.9-fold v 5.7 ± 1.2-fold for cultures with and without IL-3 + MIP-1α, respectively; P < .01) compared with cultures not supplemented with exogenous cytokines (Fig 3A and C). Maintenance/expansion of LTC-IC was also significantly better in IL-3 + MIP-1α supplemented noncontact cultures than in cytokine free noncontact cultures (at week 2: 170 ± 40% v 74 ± 20% maintenance for cultures with and without IL-3 + MIP-1α respectively, at week 5: 96 ± 20% versus 41 ± 8% maintenance for cultures with and without IL-3 + MIP-1α, respectively; P < .01) (Fig 3B and D). When IL-3 + MIP-1α was added to contact cultures, we also observed a significantly greater recovery of CFC at week 2 and week 5 than in cytokine free contact cultures (Fig 3A and C). Again, the recovery of CFC from IL-3 + MIP-1α supplemented contact or noncontact cultures was not significantly different. Addition of IL-3 + MIP-1α to contact cultures also improved the maintenance of LTC-IC at week 2 and week 5 compared with cytokine free contact cultures (Fig 3B and D). However, in contrast to what was observed for CFC, LTC-IC recovery from contact cultures supplemented with IL-3 + MIP-1α remained approximately threefold lower than that from noncontact cultures supplemented with IL-3 + MIP-1α (Fig 3B and 3D).
DISCUSSION
The widespread use of mobilized PBPC for clinical transplantation has led to numerous studies that characterize and compare committed and primitive hematopoietic progenitors present in steady state BM and mobilized PB. Compared with steady state BM CD34+ cells, mobilized PB CD34+ cells express less c-kit, CD71, and more HLA-DR and retain less rhodamine suggesting that the majority of CD34+ cells in mobilized PBPC may be relatively mature.12,13,25,36-38 Furthermore, several groups have examined the possibility to expand CFC and LTC-IC in mobilized PBPC. Short term (7 to 14 days) in vitro culture with 3 to 7 cytokines can expand the total cell number and committed progenitors in mobilized PBPC significantly.21,24,25,39 However, maintenance of primitive progenitors such as LTC-IC is poor and short lived.21,24,25,39 In the present study we examined the capacity of subpopulations of mobilized PB CD34+ cells, which contain mature and primitive progenitors to be expanded ex vivo for 2 to 5 weeks in both contact and noncontact cultures. We show that G-CSF mobilized PB CD34+HLA-DR+ cells contain mostly LTC-IC with a limited capacity for ex vivo expansion: they can sustain hematopoiesis for 5 but not for 8 weeks and cannot be maintained for even 2 weeks ex vivo. However, LTC-IC present in mobilized PB CD34+HLA-DR−, which represent 5% to 10% of mobilized PB CD34+ cells have similar proliferative potential as their counterparts in steady state BM: they can sustain hematopoiesis for 8 weeks and can be maintained for 5 weeks in noncontact culture containing IL-3 and MIP-1α.18,29 33
We have previously shown that integrin mediated adhesion of steady state BM CFC and LTC-IC to FN in marrow stromal feeders inhibits their proliferation leading to decreased expansion/maintenance of these progenitors at 2 and 5 weeks in contact cultures.20 We have recently shown that mobilized PB CD34+ cells express significantly less α4 integrin than steady state BM CD34+ (CD34+α4+++: mobilized PB 28 ± 5%, mean channel fluorescence 33 ± 2; steady state BM 46 ± 4%, mean channel fluorescence 53 ± 4). Furthermore, we demonstrate that the decreased α4 expression on mobilized CD34+ cells is associated with significantly decreased adhesion of mobilized PB CFC and LTC-IC to BM stroma. Only 29 ± 5% of CFC and 55 ± 2% of week 8 LTC-IC in mobilized PB adhere to stroma whereas 45 ± 5% CFC and 70 ± 14% week 8 LTC-IC in steady state BM adhere to stroma. Adhesion of PB progenitors, but not marrow progenitors, could also not be inhibited by anti α4 or anti-β1 antibodies. This indicates that progenitors in mobilized PB fail to adhere to BM stroma due at least in part to a decreased α4β1-integrin expression. This led to the hypothesis that expansion of mobilized PB CFC and LTC-IC would be similar in contact and noncontact cultures. However, maintenance of LTC-IC in mobilized PB CD34+HLA-DR− cells was significantly better in noncontact cultures than in contact cultures, results similar to what we have reported for BM progenitors.18 Thus, LTC-IC present in mobilized PBPC may also be subject to adhesion mediated proliferation inhibition described for BM LTC-IC. Since PBPC LTC-IC adhere significantly less to stroma than BM LTC-IC as a result of lack of α4-integrin expression these results may seem at odds with the hypothesis that integrin mediated adhesion results in inhibition of progenitor proliferation.20 However, additional studies from our group (manuscript submitted) show that removal of mobilized PB CD34+ cells from their in vivo milieu and culture of these cells for 1 to 2 days in Dexter conditions results in upregulation of α4-antigen expression and associated adhesion to BM stroma. This may thus explain the observed poorer maintenance of PB LTC-IC in contact compared with noncontact cultures. Interestingly, differences between CFC recovered from noncontact and contact cultures were less pronounced than for LTC-IC. At 2 weeks of culture equivalent, the number of CFC were present in contact and noncontact cultures while the differences were bigger at 5 weeks although not yet statistically significant. Significantly more LTC-IC were recovered at 2 weeks from noncontact than contact cultures, but the difference was greater at 5 weeks. This suggests that contact with stroma inhibits proliferation of progressively less mature progenitors (week 2 and week 5 CFC, week 2 and week 5 LTC-IC) significantly more. The mechanisms underlying this observation are currently being studied.
In previous studies we have shown that addition of the growth promoting cytokine, IL-3, and the proliferation inhibitory cytokine, MIP-1α, significantly improves maintenance of LTC-IC in noncontact cultures as a result of increased proliferation and conservation of LTC-IC while allowing production of CFC.29 IL-3 and MIP-1α also significantly increased the maintenance of LTC-IC and generation of CFC in noncontact cultures initiated with mobilized PB CD34+HLA-DR− cells, further indicating that CD34+HLA-DR− cells in mobilized PBPC have similar potential as their BM counterparts. Although IL-3 and MIP-1α improved LTC-IC maintenance in contact cultures, significantly less LTC-IC were present both at 2 and 5 weeks in contact compared with noncontact cultures. This suggests that the combination of IL-3, which can override contact mediated proliferation inhibition, at least at the CFC level,40 and MIP-1α, which may increase adhesion to stroma41 and therefore possibly adhesion mediated growth inhibition, does not seem to affect contact dependent inhibition of LTC-IC maintenance/expansion.
In conclusion, we confirm that CD34+HLA-DR+ cells present in mobilized PBPC contain progenitors that can initiate and sustain hematopoiesis in long-term cultures. However, they cannot maintain hematopoiesis beyond 5 weeks, which translates in inability to obtain CFC expansion and LTC-IC expansion/maintenance when plated in ex vivo expansion cultures. However, mobilized PBPC also contain CD34+HLA-DR− LTC-IC, which are functionally indistinguishable from LTC-IC in steady state BM: (1) they can support hematopoiesis in LTC for 8 weeks; (2) when cultured in ex vivo expansion cultures, significant CFC expansion is seen for at least 5 weeks and 100% of LTC-IC can be maintained for 5 weeks; (3) as for steady state BM LTC-IC, LTC-IC in mobilized PB CD34+HLA-DR− cells are subject to contact mediated proliferation regulation. Since the absolute number of primitive week 8 LTC-IC per mL of G-CSF mobilized PB is similar to that per mL of steady state BM, these studies further confirm that G-CSF mobilized PBPC may have similar long-term repopulating abilities as steady state BM.
ACKNOWLEDGMENT
We thank Brad Anderson for his excellent technical assistance and the nurses of the donor center for providing the samples for this study.
Supported by National Institutes of Health Grants No. RO1-HL-49930-01, RO1-HL-48730-01, PO1-CA 65493-01 (Bethesda, MD). Also supported by the Leukemia Task Force (Minneapolis, MN), the Bone Marrow Transplantation Research Fund (Minneapolis, MN), and the University of Minnesota Hospital and Clinics (Minneapolis). C.M.V. is a scholar of the Leukemia Society of America.
Address reprint requests to Catherine M. Verfaillie, MD, Department of Medicine, Box 480, 520 Delaware St SE, Minneapolis, MN 55455.