To the Editor:
Profound neutropenia bearing an increased risk of infections represents one of the cardinal problems after myeloablative and high-dose chemotherapy. In two recent reports we showed stable engraftment in patients transplanted with selected allogeneic CD34+ blood cells alone1 or in combination with bone marrow (BM).2 All patients experienced neutropenia less than 100 neutrophils/μL, lasting for 1 to 11 days. Interestingly, a transient increase of leukocyte counts was observed in some of the patients immediately after transplantation (days 1-3). The highest increase over 10,000/μL occurred in patients receiving unmanipulated BM combined with CD34+ blood cells. A similar increase was described after high-dose therapy rescued by native or ex vivo–expanded autologous peripheral blood progenitor cells (PBPC).3 Brown et al4 observed the same phenomenon and transfused additionally allogeneic PBPC 3 days after the transplantation of the original PBPC graft on day 0. Neutrophil counts increased significantly in all patients and three of six patients never experienced profound neutropenia after conditioning.4 Two major questions arise from these findings. Firstly, the donor or host origin of these increasing leukocyte numbers immediately after transplantation is not defined. Secondly, can neutropenia be further ameliorated or even prevented by such an effect?
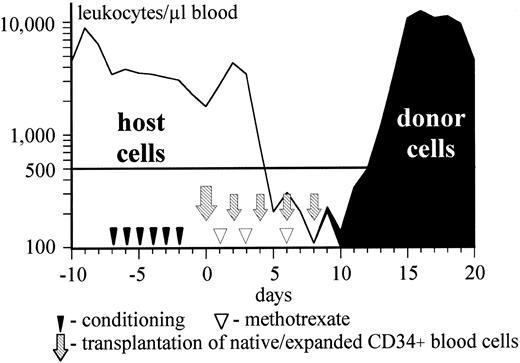
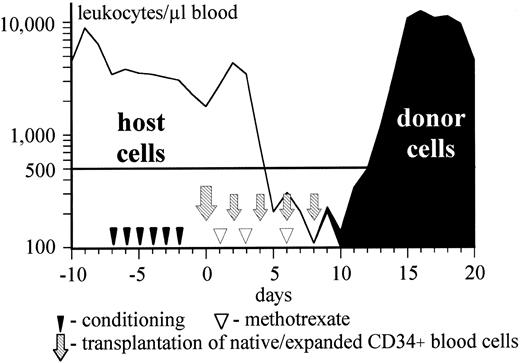
To clarify the first issue we studied three male patients (Table 1, unique patient numbers [UPN] 345, 347, and 363) transplanted with a sex-mismatched graft. Fluorescence in situ hybridization (FISH) for XY-chromosome on blood leukocytes was performed daily until complete hematopoietic reconstitution with special regard to the increase in leukocyte counts immediately posttransplant. In two of these patients (UPN 345 and 347) and an additional sex-matched patient (UPN 357), ex vivo–expanded CD34+ blood cells were transplanted as adjunct to the immunoselected CD34+ blood cell grafts, attempting to ameliorate neutropenia. The patients and transplant characteristics are presented in Table 1. Graft-versus-host disease (GVHD) prophylaxis consisted of cyclosporin A and short methotrexate.1 Granulocyte colony-stimulating factor (G-CSF ) (5 μg/kg/d) was administered subcutaneously starting on day 1 posttransplant. Profound neutropenia was not prevented in any patient, although leukocyte counts did not decrease below 100/μL in two patients (UPN 345 and 347). Immediately posttransplant an increase of leukocyte counts was observed in all three patients receiving chemical conditioning, but not in the patient conditioned with total body irradiation (TBI). Peak leukocyte numbers of 4,400, 1,200, and 6,000/μL were reached on day 2. The majority (>95%) of the cells were proven to be of host origin during this increase (Fig 1). However, FISH analysis was able to detect female cells (5 to 20/1,000) throughout the whole neutropenic phase. An almost complete switch to donor hematopoiesis was observed 1 to 5 days before neutrophil reconstitution became evident in the peripheral blood (Table 1). The infusion of ex vivo–expanded cells did not result in any adverse effects. One of the patients died of interstitial pneumonitis and multiorgan failure on day 30. A stable and durable donor hematopoiesis was established in the three other patients, who are still in complete remission 10 to 13 months posttransplant.
Kinetics of the host (XY-chromosome) and donor (XX-chromosome) leukocytes in patient UPN 345. Sex genotype was proven by FISH, counting 1,000 nucleated blood cells daily.
Kinetics of the host (XY-chromosome) and donor (XX-chromosome) leukocytes in patient UPN 345. Sex genotype was proven by FISH, counting 1,000 nucleated blood cells daily.
Retrospective analysis of 80 patients from our institution who underwent allogeneic BM transplantation with or without addition of CD34+ blood cells showed that an increase in leukocyte counts shortly after infusion of the graft occurred only after chemical conditioning and was fully abrogated by total body irradiation. A clear trend to reach higher peak values was observed in the patients receiving G-CSF posttransplant (P < .01). Both this observation and the findings in the three studied patients strongly suggest that host cells maintain some proliferative potential after myeloablative treatment with busulfan and cyclophosphamide.
Because no data about the exact scheduling in expansion duration and infusion of ex vivo–generated cells were available at the time of planning this trial, cells were cultured for different time intervals and infused to the recipients on different days (Table 1). Although a minor proportion of donor cells was found during the transient leukocyte increase and throughout the following neutropenic period, the transfusion of donor myeloid cells, expanded (UPN 345, 347, and 357) or nonexpanded (complete BM in patient UPN 363), resulted in no significant increase of circulating donor leukocytes. The overall patterns of hematopoietic reconstitution were concordant with our previously published data.1,2 Obviously, the dose of transfused progenitor cells was too low. A computer-based mathematical model of human granulocytopoiesis predicted that at least 5.7 × 108 autologous myeloid postprogenitor cells/kg (MPPC) have to be infused additionally to avoid neutropenia less than 100 neutrophils/μL after high-dose nonmyeloablative treatment.6 In accordance to the mathematical model, in two recent reports on the transplantation of ex vivo–expanded autologous PBPC all patients experienced profound neutropenia.3,7 Not more than 30% of the cells in a standard BM graft of approximately 2 × 108 nucleated cells/kg belong to the MPPC population. Thus, to achieve cell numbers necessary for a relevant early effect after transfusion about one order of magnitude more BM cells or appropriately ex vivo–generated MPPC should be given. The selected and expanded CD34+ cells, used in this trial, contained about two orders of magnitude less cells than predicted by this mathematical model. The application of methotrexate, known to delay hematopoietic reconstitution,2 may have impaired the additionally transfused proliferating donor cells.
In their preliminary report Brown et al4 showed that neutropenia was abolished in three patients receiving cyclosporin plus steroid as GVHD prophylaxis after allogeneic PBPC transplantation on days 0 and 3 without further ex vivo manipulations. Unfortunately, the conditioning regimen and the quantity of transfused PBPC cannot be abstracted from their report. PBPC grafts, collected by leukapheresis after mobilization with G-CSF, contain no or only minimal amounts of MPPC.1 2 Thus, it is not likely that sufficient amounts of progenitor cells to avoid neutropenia are provided by simple addition of a second transfusion of unmanipulated PBPC a few days after the initial transplant. The problem should be addressed in the future by improving of the ex vivo incubation conditions yielding a significantly higher quantity and probably a distinct pattern of myeloid progenitor cells.