Abstract
Peripheral blood mononuclear cells (PBMC) from patients with multiple myeloma (MM) are here shown to include 23% ± 2% of CD34+ cells, the majority of which coexpress CD19, as identified by a panel of 17 anti-CD34 antibodies. The expression of CD34 mRNA by sorted CD34+ PBMC from MM was confirmed by in situ reverse transcriptase-polymerase chain reaction (RT-PCR) with CD34-specific primers. The majority of CD34+ MM PBMC were CD19+ cells that expressed mRNA for CD19 and for rearranged IgH as identified with consensus IgH VDJ primers, as well as having cytoplasmic Ig, definitively identifying them as B cells, in absolute numbers of 0.06 to 0.69 × 109/L of blood. CD34 is largely absent from normal B cells. To determine the clonal relationship of CD34+ B cells to autologous MM plasma cells, IgH VDJ DNA rearrangements of sorted CD34+ MM blood B cells were amplified by nested PCR using consensus primers followed by Southern blotting with allele-specific oligonucleotides for 7 MM patients, and clonotypic IgH mRNA expression was assessed for 4 MM patients using quantitative patient-specific in situ RT-PCR. For 9 of 11 myeloma patients tested, CD34+ blood B cells included IgH gene rearrangements or expressed IgH mRNA identical to that of autologous bone marrow plasma cells. For 4 of 4 MM patients, 74% to 94% of individual sorted CD34+19+ B cells expressed clonotypic IgH mRNA, as detected by in situ RT-PCR with patient-specific primers. Clonotypic IgH VDJ sequences were absent from B cells of unrelated MM patients and of normal donors. Clonotypic CD34+ B cells were detected before, during, and after treatment, and during relapse. Our results indicate a clonal relationship between CD34+ MM B cells and malignant plasma cells. We speculate that CD34 may play an important role in the biology of myeloma by facilitating extravasation from blood and thus spread of myeloma through the skeletal system.
MULTIPLE MYELOMA (MM) is characterized by extensive infiltration of the bone marrow (BM) by monoclonal plasma cells.1 The self-renewing stem cell in myeloma is likely to be a B-lineage cell less mature than the end-stage plasma cells in the BM.2-7 Recent work has conclusively shown the presence in myeloma of monoclonal blood B cells (MM blood B cells)8,9 with an IgH rearrangement identical to that of autologous malignant plasma cells in myeloma.7 Sequencing of the IgH VDJ DNA from single sorted B cells of MM patients indicates that the majority have an IgH rearrangement identical to that of autologous myeloma plasma cells.10 The relationship of circulating clonotypic B cells to the malignant process is as yet undefined, but the presence of a DNA aneuploid subset5,11,12 and N-ras mutation13 suggests at least a subset of these cells may be malignant. Populations of MM blood B cells may also include members of the original antigen-specific B-cell clone from which the malignant transformant arose.8
The contribution of circulating B cells to the malignant process in MM is not fully defined. MM blood B cells express mRNA encoding Ig light chain,14 and cytoplasmic/surface Ig.5,7,15 They have the adhesive and motile properties required for a potentially invasive subset able to traffic to distant BM sites.14-17 They persist in blood despite chemotherapy7 and express functional P-glycoprotein 170,12,18,19 shown by others to modulate the response of myeloma patients to chemotherapy.20 21
No matter where myeloma originates, spread of the malignancy from the place of origin to distant BM sites must be through the blood. Traffic from blood to BM requires binding to endothelium and extravasation. CD34 is a sialomucin,22 which serves as a ligand for L-selectin,23 perhaps binding to an as yet unidentified endothelial or BM ligand and participating in homing or anchoring in a BM stromal environment.24,25 This report shows that CD34, which is expressed on normal hematopoietic stem cells,26 27 is also expressed at relatively high density on 3% to 37% of peripheral blood mononuclear cells (PBMC) in myeloma, is coexpressed with CD19 on 50% to 60% of monoclonal blood B cells in myeloma, and is absent from most myeloma plasma cells in the BM28 as well as from most normal B cells. In this report we show that individual CD34+ blood cells in MM express CD34, CD19, and IgH mRNA. CD19+ PBMC that coexpress CD34 also express IgH mRNA and cytoplasmic Ig, confirming their identity as B cells. Analysis of IgH rearrangements in DNA and mRNA of CD34+ MM B cells demonstrated the presence of an IgH VDJ rearrangement identical to that of autologous myeloma plasma cells in 9 of 11 MM patients tested, indicating a clonal relationship.
MATERIALS AND METHODS
Patients.PB and/or BM was obtained from 13 normal donors, 4 patients undergoing granulocyte colony-stimulating factor (G-CSF ) mobilization of stem cells before autologous or allogeneic transplantation, 4 cord blood samples, and blood from 96 patients with MM, some at multiple time points, including those untreated, being treated, or off treatment, as approved by the University of Alberta or University of Calgary Human Ethics Committee.
Antibodies and reagents.FMC63 (CD19) was from Dr Heddy Zola (Adelaide Children's Hospital, Australia)7,29 30 and was conjugated to fluorescein isothiocyanate (FITC). Leu-2PE (CD8), Leu-3PE (CD4), and HPCA-1 (CD34) were from Becton Dickinson (San Jose, CA). Monoclonal antibody (MoAb) 8G12 (CD34) was from Dr Peter Lansdorp (Terry Fox Laboratories, Vancouver, BC, Canada) and was conjugated to phycoerythrin (PE). Ig2aPE, IgG1, and goat anti-mouse Ig-PE were from Southern Biotech (Birmingham, AL). Anti-human Ig F(ab)2 fragments coupled to PE and goat anti-mouse Ig F(ab)2 -PE were from Southern Biotech. The panel of anti-CD34 MoAbs from the Vth International Leukocyte Typing Workshop, obtained from Dr Peter Lansdorp, were as described in Results.
Immunofluorescence (IF ) and sorting.Staining for surface phenotype used one- or two-color IF with CD19-FITC and/or the CD34 MoAb HPCA-1 or 8G12 detected in indirect IF using goat anti-mouse Ig-PE as described previously,7,12 or in double direct IF using CD19-FITC and CD34-PE (8G12). All experiments included controls with isotype-matched MoAbs in direct and/or indirect IF. For experiments to evaluate Ig content, before staining with anti-human Ig PE, PBMC already stained for surface CD34 were permeabilized with ethanol to visualize cytoplasmic Ig content; identical stainings using isotype-matched controls were always performed. PBMC stained either with HPCA-1 or 8G12 to identify all CD34+ PBMC, or with MoAbs to CD19 and CD34 (CD19+34+ and CD19+34− subsets), were sorted using the ELITE (Coulter, Hialeah, FL). Sort gates were set to include only those cells with staining brighter than the relevant isotype controls. No scatter gates were set beyond those to exclude red blood cells and dead cells. Sorts involving PBMC stained only with CD34 MoAb collected all cells with anti-CD34 staining above the isotype-matched control. For two-color sorts, to avoid cross-contamination, only the brightest CD34+ cells were included in the CD34+ CD19+ sorting gates, and only the CD19+ cells with staining below the negative control were included in the CD34− sorting gates. On reanalysis, sorted populations had 0.26% to 0.5% mean contamination by cells from the alternate sort window (see legend to Fig 2). These cells had no detectable contamination with any peripheral plasma cells as defined by their relatively low cIg content measured by immunohistochemistry and IF,7,15 and less than 1% of morphologically identifiable plasma cells in cytospins of sorted subsets or PBMC stained with Wright's stain10 as read by a skilled pathologist, and an absence of plasma cells in smears of patient blood as part of routine clinical testing. BM cells (BMC) were stained for PCA-1 (plasma cell antigen) or CD38 and cIg followed by sorting for PCA-1+cIg+ or CD38hicIg+ plasma cells and preparation of DNA to define the clonotypic IgH rearrangements present in the BM. To avoid potential contamination with plasma cells, blood samples were always sorted before BM samples, and tubing in the flow cytometer was always washed with bleach between sorts.
Expression of CD19 and CD34 on PBMC of MM patients. Representative staining by MoAb to CD34 and CD19 on PBMC from a myeloma patient. PBMC from myeloma patients were stained in dual IF with CD19-FITC and 8G12-PE (CD34), or isotype-matched control MoAb in direct IF. For each patient, positive staining was determined by comparison with the isotype-matched controls. Each row represents one patient. For these patients, the rectangles identify the sort windows for purification of CD34+19+ and CD34−19+ MM PBMC (left panels). Reanalysis of sorted subsets indicated the percent purity recorded within each sort window (middle and right panels). Overall, for CD34+19+ sorts 98% ± 0.7% were within the selected sort window and had 0.26% ± 0.3% cells from the other sort window; for CD34−19+ sorts 97% ± 0.5% were within the selected sort window and 0.5% ± 0.6% were from the other sort window (values are mean ±SD).
Expression of CD19 and CD34 on PBMC of MM patients. Representative staining by MoAb to CD34 and CD19 on PBMC from a myeloma patient. PBMC from myeloma patients were stained in dual IF with CD19-FITC and 8G12-PE (CD34), or isotype-matched control MoAb in direct IF. For each patient, positive staining was determined by comparison with the isotype-matched controls. Each row represents one patient. For these patients, the rectangles identify the sort windows for purification of CD34+19+ and CD34−19+ MM PBMC (left panels). Reanalysis of sorted subsets indicated the percent purity recorded within each sort window (middle and right panels). Overall, for CD34+19+ sorts 98% ± 0.7% were within the selected sort window and had 0.26% ± 0.3% cells from the other sort window; for CD34−19+ sorts 97% ± 0.5% were within the selected sort window and 0.5% ± 0.6% were from the other sort window (values are mean ±SD).
In situ reverse transcriptase-polymerase chain reaction (RT-PCR).In situ RT-PCR31 was used to quantitate the proportion of sorted PBMC expressing mRNA encoding CD34, IgH, CD19, or histone. PBMC from MM patients were stained in double direct immunofluorescence with MoAbs CD19-FITC and CD34-PE, and fixed in 10% formalin/PBS overnight. Using the ELITE Autoclone (Coulter), total CD34+ PBMC or CD34+19+ B cells were sorted at 10,000 cells per well into a flat-bottom 96-well microtiter tray. Rapid processing before the fixation step was essential to preserve mRNA. Samples were placed in three spots, at 10,000 cells per spot, on In Situ PCR glass slides (Perkin Elmer, Mississagua, Ontario, Canada) and air dried. Cells were permeabilized using 2 mg pepsin (Boehringer Mannheim, Laval, Quebec, Canada) per milliliter of 0.01N HCl. The time of pepsin digestion was carefully optimized. Pepsin was inactivated by a 1-minute wash in diethyl pyrocarbonate (DEPC)-treated water followed by a 1-minute wash in 100% ethanol. Digestion with 1,000 U/mL of DNAseI (RNAse-free) (Boehringer Mannheim) removed genomic DNA from the negative control and the test sample before reverse transcription. Incubation of the sample with DNAseI was performed in the In Situ PCR System (Perkin Elmer) thermal cycler at 37°C overnight. DNAseI was removed by a 1-minute wash in DEPC-treated water followed by a 1-minute wash in 100% ethanol. In situ reverse transcription was performed for 60 minutes at 37°C only for the test samples under standard conditions recommended by the manufacturer using SuperScript (GIBCO-BRL, Burlington, Ontario, Canada) and the universal primer dT16 . After washing with water and ethanol, an In Situ Core Kit (Perkin Elmer) was used to amplify a target sequence during 25 to 30 cycles (94°C for 1 minute, 56°C for 1 minute, and 72°C for 1.5 minutes) with a direct incorporation of DIG-11-dUTP (Boehringer Mannheim) during PCR to label the product. Amplified DNA was detected using anti-DIG Fab conjugated with alkaline phosphatase (Boehringer Mannheim), followed by incubation with NBT/BCIP substrate solution (Boehringer Mannheim). Color development was monitored under the microscope. Negative controls for every sample included omitting the RT step to confirm digestion of genomic DNA which would otherwise lead to amplification of nonspecific PCR products, and an aliquot with intact DNA as a positive control for the amplification reagents. Every slide had three spots of cells that were used for the negative control, the positive control, and the test spot; the test sample was only evaluated if the two controls on each slide were, respectively, negative and positive. As a positive control for the RT-PCR with specific primers, when sufficient cells were available, a slide was processed to amplify mRNA for a housekeeping gene, histone, to quantitate the number of cells with intact mRNA. As a control for the specificity of the primers used to amplify CD34, IgH, and CD19 mRNA, autologous T cells were tested and were negative,10 as expected, although a small set of T cells (up to 8%) occasionally gave weak positive staining for CD34 mRNA. Positive B cells were visually defined as those with an intensity of color development greater than that of autologous T cells. Primers were as follows: Histone 5′ CCACTGAACTTCTGATTCGC; Histone 3′ GCGTGCTAGCTGGATGTCTT; CD19 5′ GACCTCACCATGGCCCCTGG; CD19 3′ CAGCCAGTGCCATAGTAC; CD34 5′ GGAATTCGAGGCCACAACAAACATCAC; CD34 3′ GGAATTCGCAGATGCCCTGAGTCAATT; IgH FR2 5′ TATGAATTCGGAAAGGGCCTGGAGTGG; IgH JH 3′ ACGGGATCCACCTGAGGAGACGGTGACC.
Ig heavy chain gene (IgH) CDR3 PCR and allele-specific oligonucleotide (ASO) Southern blotting.For the patients analyzed in Fig 3, PCR was used to amplify VDJ rearrangements in DNA from blood CD19+ B cells sorted into CD34− and CD34+ subsets. For all MM patients tested, BM samples were taken during the course of the study, from which a single IgH VDJ band with a unique sequence was amplified from DNA as previously described.7 BM plasma cells were purified by sorting for cells that coexpressed the plasma cell marker PCA-1 and a high density of cytoplasmic Ig (cIg). IgH VDJ PCR used 1,000 cells from each subset as previously described, using consensus primers in nested PCR,7 followed by electophoresis on a 4% Nusieve GTG agarose gel (FMC Bioproducts, Rockland, ME). These Ig fingerprints were transferred to nylon filters by Southern blotting and hybridized with end-labeled ASO probes designed using the patient-specific IgH-CDR3 sequence of purified BM plasma cells from the same patient as detailed previously.7 The presence of ASO sequences in each subset was also confirmed using ASO-PCR.7 N-ras DNA was amplified as a positive control to confirm that the DNA in each sample was intact. For sequencing and synthesis of ASO probes, the CDR3 PCR products were amplified as above, purified from an agarose gel using Promega Magic PCR Preps (Promega, Madison, WI), and the nucleotide sequence determined using end-labeled oligonucleotides FR2 and JH2 with Promega's fmol PCR sequencing kit. ASO were designed based on the nucleotide sequence, and synthesized by Genosys Biotechnologies Inc (The Woodlands, TX).
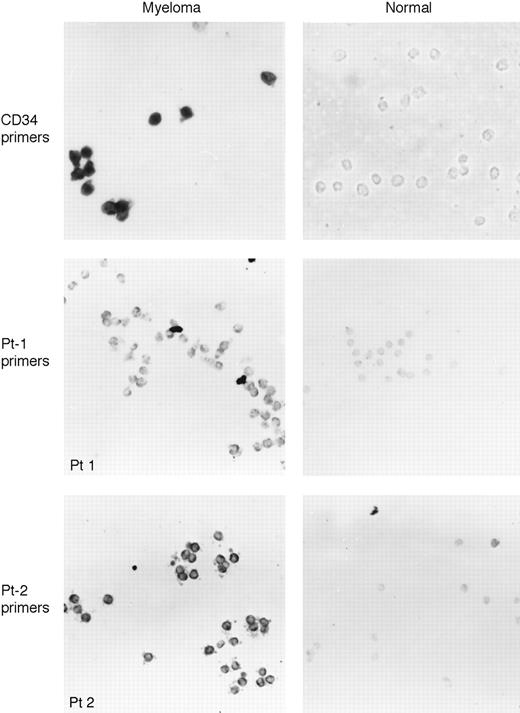
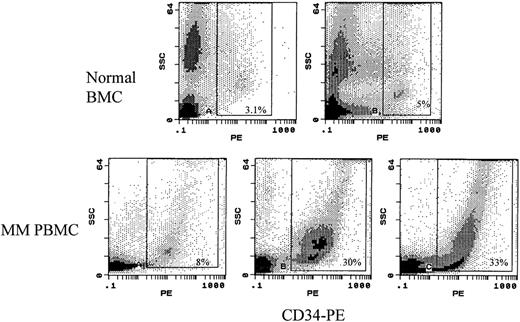
In situ RT-PCR amplification of CD34 or clonotypic IgH VDJ mRNA in sorted CD19+ MM or normal donor B cells. Sorted CD19+ MM, CD34+19+ MM, or normal donor PBMC were placed on slides and using primers to CD34 (top row, CD19+ MM PBMC or normal CD19+ PBMC) or to patient-specific IgH VDJ (middle row, Pt-1 primers on MM Pt-1 CD34+19+ PBMC or normal PBMC CD19+ B cells; bottom row, Pt-2 primers on MM Pt-2 CD34+19+ PBMC or normal CD19+ PBMC B cells), mRNA was amplified using digoxygenin-labeled nucleotide, followed by visualization with antidigoxygenin antibody in a colorimetric assay. The experiment of the top row used a blue dye, Nitro blue tetrazolium chloride, as substrate while the experiment of the middle and bottom rows used Fast Red as the substrate. Positive cells exhibit intense color deposition. MM CD34+19+ blood cells are shown in column 1 (left) and CD19+ B cells from blood of normal donors in column 2 (right).
In situ RT-PCR amplification of CD34 or clonotypic IgH VDJ mRNA in sorted CD19+ MM or normal donor B cells. Sorted CD19+ MM, CD34+19+ MM, or normal donor PBMC were placed on slides and using primers to CD34 (top row, CD19+ MM PBMC or normal CD19+ PBMC) or to patient-specific IgH VDJ (middle row, Pt-1 primers on MM Pt-1 CD34+19+ PBMC or normal PBMC CD19+ B cells; bottom row, Pt-2 primers on MM Pt-2 CD34+19+ PBMC or normal CD19+ PBMC B cells), mRNA was amplified using digoxygenin-labeled nucleotide, followed by visualization with antidigoxygenin antibody in a colorimetric assay. The experiment of the top row used a blue dye, Nitro blue tetrazolium chloride, as substrate while the experiment of the middle and bottom rows used Fast Red as the substrate. Positive cells exhibit intense color deposition. MM CD34+19+ blood cells are shown in column 1 (left) and CD19+ B cells from blood of normal donors in column 2 (right).
Identification of clonotypic IgH VDJ sequences in individual CD34+19+ B cells.For 4 MM patients, the clonotypic IgH VDJ was identified using single-cell RT-PCR with individual sorted CD38hicIg+SSchi BMC.10 The consensus primers described above were used to amplify each plasma cell IgH VDJ, followed by sequencing of the product from at least three individual plasma cells.10 The IgH VDJ sequence identified in consensus RT-PCR was confirmed as clonotypic by in situ RT-PCR or single-cell RT-PCR with patient-specific primers using either BMC or sorted BM plasma cells. For all 4 patients, greater than 80% of individual BM plasma cells expressed the sequence defined as clonotypic. Sorted CD34+19+ MM PBMC were analyzed by patient-specific in situ RT-PCR as described above. The in situ amplification was confirmed as patient-specific by the lack of amplification in sorted B and plasma cells from irrelevant MM patients or from sorted B cells from normal donors. Patient-specific in situ RT-PCR used primers annealing to the patient-specific CDR3 and either CDR2 or FR2. For some MM patients, use of the FR2 primer gave the cleanest amplification, while for others the CDR2 primer was optimal; primers were chosen to obtain a single discrete band in bulk RT-PCR with BM plasma cells.
RESULTS
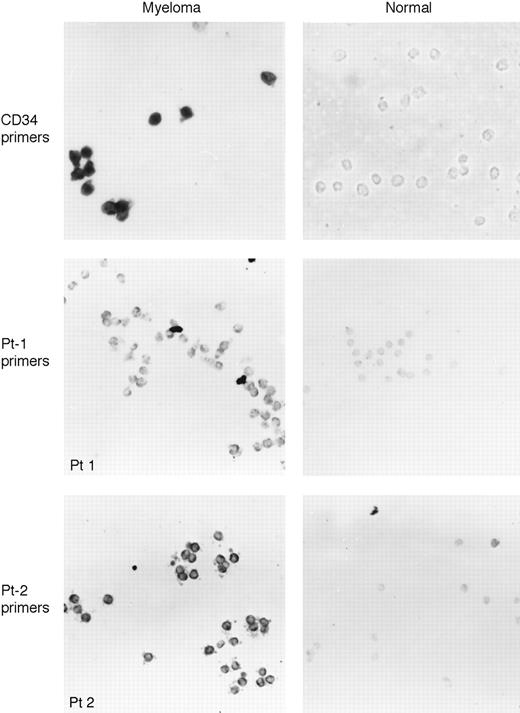
CD34+ cells in the blood of myeloma patients express IgH and CD19 mRNA.In 96 MM patients analyzed, 3% to 37% of PBMC were CD34med/hi (mean = 23% ±2%), compared with less than 1% in normal adult blood, 1% to 4% in cord blood, 1% to 5% in G-CSF–mobilized blood, and 3% to 5% in adult BM (Table 1 and Fig 1). A comparable number of CD34+ MM or normal PBMC/BMC were detected using either direct or indirect IF to detect CD34 (Table 1). The CD34+ populations from both normal and MM donors had a heterogeneous scatter profile, including both small and large cells (Table 1). The majority of CD34+ PBMC in MM and a substantial proportion in normal donor PBMC or BMC coexpressed CD19 (77% to 84%) (Table 1).
Expression of CD34 on MM PBMC compared with normal BM. Cells from two individual normal BM (top row) or 3 MM patients (bottom row) were stained with a direct conjugate of CD34-PE, followed by a scatter plot of CD34 versus side scatter. The rectangle indicates those cells identified as CD34+.
Expression of CD34 on MM PBMC compared with normal BM. Cells from two individual normal BM (top row) or 3 MM patients (bottom row) were stained with a direct conjugate of CD34-PE, followed by a scatter plot of CD34 versus side scatter. The rectangle indicates those cells identified as CD34+.
To confirm the expression of CD34 on the CD34+ MM PBMC as defined by MoAb staining, in situ RT-PCR was used to quantitate the proportion of sorted CD34+ MM PBMC expressing CD34 mRNA. Table 2 confirms that on average 79% of CD34+ MM PBMC identified as CD34+ by MoAb staining also expressed CD34 mRNA. We reproducibly found that a minor subset, about 20%, of CD34+ MM PBMC lacked detectable CD34 mRNA, suggesting that CD34 mRNA synthesis had been downregulated but surface expression of CD34 was maintained. The majority (84%) of CD34+ MM PBMC also expressed mRNA for CD19 and rearranged IgH VDJ (Table 2). Of CD34+ MM PBMC falling within the small lymphocyte gates, 79% expressed CD34 mRNA, and 51% expressed CD19 mRNA (Table 2).
Most CD34+ PBMC in MM coexpress CD19.MM includes circulating CD19+ B cells with IgH gene rearrangements identical to those of autologous myeloma plasma cells.7 10 We analyzed the coexpression of CD34 and CD19 on circulating B cells from MM patients. On average, of CD34+ MM PBMC, 84% ± 4% were phenotypically detected as CD19+, and 87% ± 5% expressed CD19 mRNA (Tables 1 and 2). Representative MM patients are shown in Fig 2. Figure 2 also shows the sort windows used to purify MM subsets defined by CD34 and CD19, and the purity of sorted subsets. For the 96 patients in this study, 55% ± 5% of CD19+ B cells coexpressed CD34 (range = 28% to 98%).
On average, of B cells from normal donors only 5% express CD34 (Table 3). For the 96 MM patients studied here, the expression of CD34 was analyzed on MM blood B cells, subdivided by their physical flow cytometric scatter properties into small and large subsets. CD34 was expressed at medium to high density by the majority of large B cells from all patients, including the untreated group (Table 4). Of the small B-cell subset, 5% to 25% expressed CD34. For untreated patients, few of the small B-cell subset were CD34+, comparable to B cells from normal donors. However, compared with normal donors or untreated patients, a significantly higher proportion of CD34+ small B cells was detected in patients during and after chemotherapeutic treatment. Consistent with the work of others,28 the majority of BM plasma cells from 14 different myeloma patients had no or very low expression of CD34 (Table 3).
The expression of CD34 on CD19+ MM PBMC was confirmed in two-color IF, using MoAb to CD19 together with each of 17 different anti-CD34 MoAbs, to detect all of the three identified epitopes of CD34 (Table 4), as defined by staining greater than that of the relevant isotype matched control MoAb. CD34 expression in the aggregate population was also confirmed by amplification of CD34 mRNA from bulk mRNA isolated from purified myeloma blood B cells (not shown). In contrast, only 1% to 2% of B cells from 5 normal donors stained with any members of the CD34 MoAb panel (Table 4).
Individual CD19+ MM PBMC express CD34, CD19, and IgH mRNA.To confirm their expression of CD34, CD19+ PBMC from the blood of MM patients were sorted and analyzed using in situ RT-PCR to quantitate the proportion with detectable CD34 mRNA. All CD19+ PBMC expressed CD19 mRNA and IgH mRNA, confirming their identity as B cells and validating their expression of CD19 (Table 5). Autologous T cells lacked mRNA for either CD19 or IgH providing a negative control for each patient.10 For 6 MM patients, 27% to 82% of CD19+ B cells expressed CD34 mRNA, confirming their expression of CD34 as defined by IF with anti-CD34 MoAbs (Table 5). B cells from normal donors had low numbers with detectable CD34 mRNA (0.3% to 1.8% positive) (Table 5), consistent with their phenotypic profile (Table 1). Figure 3 shows representative in situ RT-PCR amplification of CD34 mRNA in sorted MM or normal donor B cells using CD34 primers.
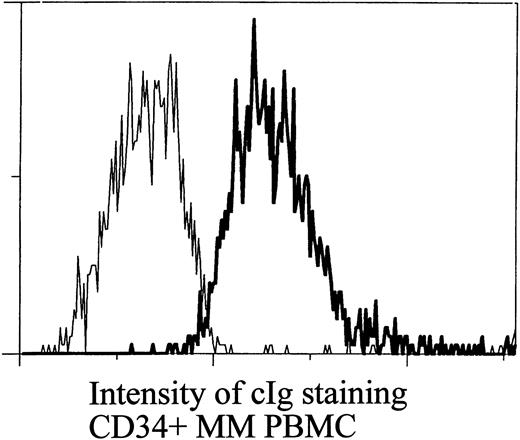
CD34+ B cells in myeloma blood express cytoplasmic Ig.Ig expression of CD34+ blood B cells is shown in Fig 4. Eighty-five percent of all CD34+ blood cells expressed a low-moderate density of Ig, approximately 3- to 10-fold less intense than that seen for BM plasma cells. Comparable Ig expression was seen in both CD34+ and CD34− B cells (not shown). The Ig−CD19− subset of CD34+ small PBMC has been characterized by others as including normal hematopoietic stem cells. Overall, of small PBMC from MM patients, 0.3% to 2.7% were CD34+Ig+, and 0.2% to 0.7% were CD34hiIg− comparable to PBMC from normal donors (Table 1).
CD34+ PBMC express cytoplasmic Ig. PBMC were stained with anti-CD34, followed by ethanol permeabilization and staining with FITC-coupled F(ab)2 fragments of anti-human Ig, or anti-mouse Ig (control). The thin line represents control staining and the thick line represents staining with anti-human Ig. Intensity of staining is on a log scale.
CD34+ PBMC express cytoplasmic Ig. PBMC were stained with anti-CD34, followed by ethanol permeabilization and staining with FITC-coupled F(ab)2 fragments of anti-human Ig, or anti-mouse Ig (control). The thin line represents control staining and the thick line represents staining with anti-human Ig. Intensity of staining is on a log scale.
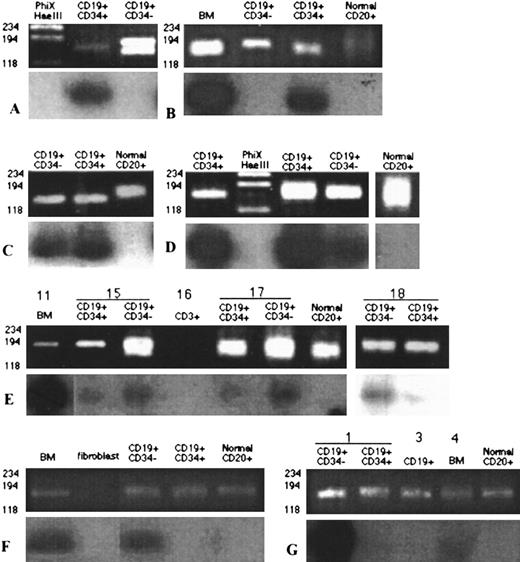
CD34+19+ MM B cells have clonotypic IgH VDJ rearrangements in DNA.To evaluate the relationship of circulating CD34+19+ B cells to the malignant clone in MM, their genomic IgH rearrangements were amplified. All of the IgH rearrangements present in the B-cell population were first amplified by nested consensus CDR3 PCR. To detect patient-specific IgH rearrangements, the amplified products were then hybridized under stringent conditions with a patient-specific oligonucleotide probe (ASO), defined by the CDR3 IgH rearrangement of the BM plasma cells. Because all MM blood B cells express IgH mRNA9,10 (Table 5) and Ig protein (Fig 5),7,15 all purified subsets should, and do, have detectable rearrangement(s) amplified in the consensus CDR3 PCR.7 For 7 patients a unique IgH DNA rearrangement, as confirmed by sequencing (Table 6), was amplified from their BM plasma cells. IgH CDR3 rearrangements were amplified from the DNA of 1,000 CD34+ or CD34− blood B cells and hybridized with an ASO probe labeled with 32P (Fig 5). This assay is semi-quantitative because the density of the band after hybridization with the ASO probe is compared with the density of the band generated by consensus primers for IgH VDJ in each sample of sorted B cells from MM or normal donors. By amplifying all of the rearrangements in a sample, little selection is imposed by the PCR, allowing one to determine the proportion of the amplified rearrangements that are clonal. In relative terms the presence of clonotypic sequences can be compared between samples and patients. Figure 5 shows that three distinct patterns of ASO expression in CD34+ and CD34− blood B cells were detectable, those with clonotypic cells mainly in the CD34+ subset (A and B, 2 of 7 patients), those with both CD34+ and CD34− clonotypic B cells (C through E, 3 of 7 patients), and those with clonotypic cells detectable mainly in the CD34− subset (F and G, 2 of 7 patients). The detection of CDR3 rearrangements by consensus PCR amplification is shown in the top half of each panel, and the extent to which these rearrangements hybridized with the appropriate ASO probe is shown in the lower half of each panel. The ASO blots indicate the relative frequency of the ASO sequence in the subsets being compared, and where positive, confirm the patient-specific identity of the amplified rearrangements. PCR false negatives are eliminated because all of the rearrangements in a sample are amplified, and visualized, controlling for the quality of DNA, and the PCR amplification. PCR false positives are also controlled for since all of the different patient samples are amplified identically, so that any PCR contaminant could not be patient-specific.
CD34+ and CD34− B cells in the blood of myeloma patients have IgH rearrangements identical to those of autologous BM plasma cells. (A) through (G) represent analysis of sorted lymphocyte subsets from 7 different patients. In each panel the top half shows CDR3 rearrangements amplified by nested PCR from 103 sorted cells of the indicated PBMC subsets, using consensus primers to FR2a and JH1 followed by a second-stage PCR amplification using consensus primers to FR2b and JH2.7 The bottom half of each panel shows the hybridization of amplified products with end-labeled patient-specific ASO probes. Patient A was post chemotherapy with stable disease. Patients B through D were in relapse. Patient E was analyzed at relapse (no. 11), during his second round of chemotherapy (no. 15) where a partial response occurred, and in the progressive stage of disease (nos. 17 and 18). Patient F was at diagnosis and untreated. Patient G had received the first two cycles of chemotherapy after diagnosis.
CD34+ and CD34− B cells in the blood of myeloma patients have IgH rearrangements identical to those of autologous BM plasma cells. (A) through (G) represent analysis of sorted lymphocyte subsets from 7 different patients. In each panel the top half shows CDR3 rearrangements amplified by nested PCR from 103 sorted cells of the indicated PBMC subsets, using consensus primers to FR2a and JH1 followed by a second-stage PCR amplification using consensus primers to FR2b and JH2.7 The bottom half of each panel shows the hybridization of amplified products with end-labeled patient-specific ASO probes. Patient A was post chemotherapy with stable disease. Patients B through D were in relapse. Patient E was analyzed at relapse (no. 11), during his second round of chemotherapy (no. 15) where a partial response occurred, and in the progressive stage of disease (nos. 17 and 18). Patient F was at diagnosis and untreated. Patient G had received the first two cycles of chemotherapy after diagnosis.
The specificity of the amplification was confirmed by the lack of amplification of IgH rearrangements from sorted T cells from myeloma patients, from fibroblasts (panels E through G), or from water (data not shown). The specificity of the ASO blotting was confirmed by the absence of hybridization to any of the bands amplified from polyclonal PBMC B cells from normal donors (panels B through G). Previous work has established that ASO probes hybridize only to bands amplified from the appropriate myeloma patient.7
For patients A and B, although IgH CDR3 sequences were amplified for all subsets, only those amplified from the CD34+ subset of blood B cells hybridized with the ASO probes defined by the IgH CDR3 rearrangement from autologous BM plasma cells. For patients C through E, hybridization with ASO probes was seen for rearrangements amplified from both CD34+ and CD34− B cells, and in relative terms, a greater proportion of CD34+ B cells were clonotypic for C and D, while for E, CD34− B cells appeared to have the greater proportion of the ASO sequence. Patient E was analyzed at three different time points over a 10-month period and the expression of ASO sequences in both CD34+ and CD34− subsets was consistently seen, as was the relatively greater hybridization in the CD34− subset. For patients F and G, the ASO sequences were mainly detected among the CD34− B cells; patient F was newly diagnosed and patient G was 2 months postdiagnosis. Patients A through E, all of whom had clonotypic sequences among the CD34+ B-cell subset, were postchemotherapy, and all except A were in relapse.
CD34+19+ B cells express clonotypic IgH VDJ mRNA: Quantitative enumeration using in situ RT-PCR shows the majority of individual CD34+ B cells are clonotypic.To determine the number of individual CD34+19+ B cells in MM PBMC that were expressing clonotypic IgH mRNA, in situ RT-PCR using patient-specific primers (CDR3 and CDR2 or FR2) was used (Table 7 and Fig 3). Because in situ RT-PCR amplification detects as few as 1 to 10 copies of IgH VDJ mRNA32 33 in individual cells with a colorimetric sandwich assay, this method is considerably more sensitive than the bulk PCR followed by ASO Southern blotting described above. CD34+19+ MM B cells were sorted, placed on slides, and their mRNA amplified using patient-specific primers (Table 6). For all 4 patients, the IgH VDJ sequences defined as patient-specific were confirmed to be clonotypic by their expression in 80% or more of individual autologous BM plasma cells, but not from plasma cells of unrelated MM patients. As a negative control in the in situ RT-PCR, patient-specific primers did not amplify detectable product in any of the sorted B cells from unrelated MM patients or normal donors (Table 7).
For 4 of 4 MM patients tested, patient-specific primers amplified a clonotypic product in 74% to 94% of individual CD34+19+ B cells, confirming that for all MM patients tested nearly all cells in this PBMC subset are clonally related to the malignant BM plasma cells in MM (Table 7). Figure 3, bottom row, shows representative patient-specific in situ RT-PCR for the appropriate MM patient where nearly all cells are positive, and for B cells from a normal donor, which are negative (Fig 3). Of the 4 patients shown, 1 was untreated (no. 2), 1 had recently undergone a transition from monoclonal gammopathy of undetermined significance (MGUS) to MM and initiated chemotherapy (no. 8), 1 had completed chemotherapy (no. 1), and 1 was in relapse (no. 9).
DISCUSSION
This work shows that CD34+ B cells in MM PBMC have clonotypic IgH VDJ gene rearrangements and express clonotypic IgH mRNA. Unusually high numbers of CD34+ cells that coexpress CD19 and have IgH gene rearrangements and IgH mRNA (mean = 23%, 0.22 × 109/L) are found in the blood of patients with MM. The expression of CD34 was confirmed by in situ RT-PCR showing the presence of CD34 mRNA in 75% to 85% of sorted CD34+ MM PBMC. The majority (84%) of these CD34+ MM PBMC coexpressed CD19 as defined by MoAb staining and in situ RT-PCR. Of CD19+ MM PBMC, 55% coexpressed CD34. Using in situ RT-PCR, the identity of these CD19+ MM PBMC as B cells was validated by their expression of mRNA encoding CD19 and IgH. In situ RT-PCR indicated that 27% to 98% of sorted CD19+ B cells from individual MM patients expressed CD34 mRNA (mean = 65%), confirming their expression of CD34. An analysis of clonotypic IgH rearrangements using in situ RT-PCR conclusively demonstrated that 74% to 94% of individual sorted CD34+19+ MM blood B cells express clonotypic IgH VDJ mRNA, confirming their clonal relationship to autologous BM plasma cells. Expression of an identical IgH rearrangement, while proving a direct relationship to the malignant clone, does not necessarily indicate that these cells are malignant.8 However, the CD34+ MM blood B cells accumulate excess DNA (DNA aneuploidy5,11,12 ), a characteristic abnormality of malignant cells that is absent from normal B cells, suggesting that the CD34+ MM blood B cells may include a malignant component. For one MM patient, a proportion of CD34+ blood B cells express a mutant N-ras oncogene identical to that of autologous BM plasma cells, providing a genetic marker of tumor progression.13 Thus, it seems likely that these B cells include both malignant and nonmalignant subpopulations.8
A combination of CDR3-PCR and ASO-Southern blotting, or the use of in situ RT-PCR with patient-specific primers, detected the presence of clonotypic IgH rearrangements in the DNA and mRNA of CD34+19+ blood B cells for 9 of 11 MM patients. Of the 9 MM patients for whom clonotypic sequences were detected in CD34+ blood B cells, 2 were untreated, 2 were responding to intermittent chemotherapy, and 5 were in relapse. Their presence throughout the progressive stages of MM indicates that these cells precede treatment and persist despite chemotherapy. For accurate quantitation of clonotypic involvement within CD34+ MM B cells, in situ RT-PCR with patient-specific primers used clonotypic sequences confirmed to be expressed by greater than 80% of autologous BM plasma cells. For 4 of 4 patients, a mean of 87% clonotypic cells were detected among CD34+19+ MM B cells. This assay, which can detect a single copy of the target sequence,32,33 is considerably more sensitive than is hybridization or bulk PCR followed by ASO Southern blotting. The 2 MM patients for whom clonotypic sequences were not detectable among the CD34+ B cells were assayed only using the less sensitive ASO hybridization strategy. For those MM patients analyzed by in situ RT-PCR, 4 of 4 had CD34+19+ B cells that were essentially all clonotypic. Clonotypic IgH rearrangements are not found in normal B cells, nor are they shared between different patients,7 10 confirming the specificity of both analytical methods.
This work demonstrates the presence of CD34 on cells in the clonal hierarchy of myeloma. Thus, some of these cells may copurify with CD34+ hematopoietic cells used in autologous transplantation, although the extent to which they appear in stem cell harvests used for autologous transplantation is unclear. This work suggests that those clonal cells that are detectable in stem cell harvests34-37 are bona fide CD34+ cells. Experiments are in progress to quantitate the extent to which clonotypic members of the myeloma hierarchy are found among mobilized CD34+ populations from myeloma patients. A recent report indicates no detectable tumor contamination of CD34+ stem cells purified from MM BM,28 consistent with our finding that CD34 is absent from BM-localized plasma or B cells. Primitive CD34+ cells have been shown to express Thy-1 (38), and in myeloma it appears that only the Thy1+Lin− subset of CD34+ blood cells may be free of the myeloma clone.37 Consistent with this, the MM B cells described here appear to lack expression of Thy1 (unpublished observations, July 1996).
This and other work5-8,12,14,16,17,19,39 suggest a role for MM blood B cells as mediators of malignant spread in myeloma. In this context, the expression of CD34 may provide a significant biologic advantage to the MM clone. We speculate that MM blood B cells expressing CD34 have increased potential for extravasation and homing to the BM, facilitated by the adhesive properties of CD3422-24 that have been confirmed in CD34 transgenic mice,25 as well as its role in enhancing adhesion mediated by other receptors.40 In this respect the behavioral properties of CD34+ MM blood B cells may be analogous to those of normal CD34+ hematopoietic stem cells. It is likely that migration between blood and BM, perhaps involving CD34, is a prerequisite for the spread of myeloma to multiple BM sites. Nearly all of the CD34+ MM B cells described here express the unique, patient-specific IgH rearrangement that characterizes malignant cells in MM, confirming their clonal relationship with autologous MM plasma cells. At present, however, their place of origin and their in vivo ability to colonize the host BM microenvironment are unknown.
ACKNOWLEDGMENT
Juanita Wizniak provided untiring, skilled, and enthusiastic expertise in flow cytometry and cell sorting. Darlene Paine and Karen Seeberger provided expert technical assistance. We are grateful to the many patients who donated their blood and bone marrow. Dr Peter Lansdorp generously provided helpful discussions as well as MoAb 8G12, the panel of anti-CD34 MoAbs, and the primer sequences for CD34 RT-PCR.
Supported by the National Cancer Institute of Canada, the Alberta Cancer Board Research Initiatives Program, the Alberta Cancer Foundation, and The Cancer Research Society.
Address reprint requests to Linda M. Pilarski, PhD, Department of Oncology, University of Alberta, Edmonton, Alberta, Canada T6G1Z2.