Abstract
In an attempt to explore novel treatment modalities in acute myeloid leukemia (AML), we studied the role of costimulatory and cytokine gene immunotherapy in murine AML. We have previously shown that leukemic mice can be cured with CD80 transfected leukemic cells (B7.1-AML vaccine) administered early in the course of the disease and that the failure B7.1-AML vaccines administered late cannot be attributed to immunosuppression induced by tumor growth. CD8+ T cells, which are necessary for tumor rejection, are activated rather than suppressed during the first half of the leukemic course in nonvaccinated mice. In this report, we question whether CD86 (B7.2) or the cytokines granulocyte-macrophage colony-stimulating factor (GM-CSF), interleukin-4 (IL-4), or tumor necrosis factor-α (TNF-α) can improve the vaccination potential of AML cells. The choice of cytokines was based on their combined and alone as well ability to direct the differentiation of CD34+ cells into potent antigen-presenting dendritic cells in vitro. Our studies show that (1) mice vaccinated with a leukemogenic number of AML cells engineered to express B7.2 (B7.2-AML) or to secrete GM-CSF, IL-4, or TNF-α (GM-, IL-4–, TNF-α–AML) do not develop leukemia; (2) GM-AML cells are tumorigenic in sublethally irradiated SJL/J mice but not in Swiss nu/nu mice, indicating that killing of tumor cells is not T-cell–dependent; (3) vaccines with irradiated GM-AML, but not B7.2-, IL-4–, or TNF-α–AML cells, can elicit leukemia-specific protective and therapeutic immunity; and (4) in head-to-head comparison experiments, vaccination with irradiated GM-AML is more potent than B7.1-AML, curing 80% and providing 20% prolonged survival of the leukemic mice at week 2, as opposed to cures only up to 1 week with B7.1-AML vaccines. These preclinical data emphasize that GM-CSF gene immunotherapy deserves clinical evaluation in AML.
IN RECENT YEARS, a tremendous amount of information has emerged regarding biochemical and molecular mechanisms that control the biology of acute myelogenous leukemia cells.1-3 However, these advances have not yet translated into novel therapeutic approaches. Despite the developments in new regimens for induction of remission therapy and in supportive care, long-term survival is usually only achieved in 25% to 30% of patients.4 Factors predisposing to this unfavorable outcome have still to be defined. Certain karyotypic abnormalities and the multidrug resistance phenotype have been considered as principal mechanisms affecting the rate and duration of complete remission in acute myeloid leukemia (AML).4,5 At present, two new treatment modalities represent hopeful prospects for improving the outcome in AML: (1) the use of potent multidrug resistance reversal agents that do not cause immunosuppression4,6 and (2) the use of immunomodulatory compounds or tumor-cell vaccines as adjuvant treatment.7 8 Both treatment modalities are novel approaches that need careful clinical evaluation.
Intense research on animal tumor models has shown that tumor growth does not eliminate immunity against nonself tumor-specific antigens.9,10 Primary factors that have been implicated for the escape of tumor cells from an effective cytolytic response are the lack of expression of costimulatory molecules by most of the tumor cells11 and the absence of an appropriate cytokine microenvironment.12 Numerous studies have emphasized the effectiveness of heightened expression of B7 costimulatory molecules13,14 and immunoregulatory cytokines, such as interleukin-2 (IL-2), IL-4, IL-6, interferon-γ, and granulocyte-macrophage colony-stimulating factor (GM-CSF), in antitumor immunity.15-19 Because few tumor-specific antigenic determinants are currently known, most of these studies have used whole tumor cell vaccines.
The mechanisms by which tumor cells that are engineered to secrete cytokines induce tumor-specific immunity differ from vaccine to vaccine.20,21 Variables influencing this outcome include the immunogenicity of the tumor, the microenvironment surrounding the tumor, the type of cytokine secreted, and, finally, the amount of cytokine secreted.20 In recent reports comparing the ability of different cytokines to enhance the immunogenicity of murine tumor cells, GM-CSF was the most potent molecule for inducing antitumor immunity.19,22 It has been speculated that this effect may be due to the ability of GM-CSF to promote differentiation of dendritic cells (DC),10 which are very potent antigen-presenting cells (APC) for activating both class I- and class II-restricted T cells.23 This idea is strengthened by studies on the ex vivo generation of functionally mature DC from human CD34+bone marrow precursors, showing that GM-CSF or the combination of GM-CSF and IL-4 or tumor necrosis factor-α (TNF-α) promote the differentiation of CD34+ bone marrow cells and their acquisition of DC phenotypic and functional characteristics within 7 to 8 days.24 25
Murine acute leukemia cells that are genetically modified to express B7 costimulatory molecules can become immunogenic and be used effectively as vaccines.26-29 We and others have shown that B7-1 vaccines eliminate only a relatively small leukemic burden; hence, their efficacy is lost in later stages of the disease.26,27The hypothesis that progressive tumor growth modulates the outcome of immunotherapeutic strategies was not confirmed by our later studies, showing that the CD8+ T cells necessary for tumor rejection are activated rather than suppressed during the leukemic course.30 In this respect, we investigated whether transduction of AML cells with molecules other than B7.1 can enhance immunogenicity and vaccine efficacy. First, we tested whether the costimulatory ligand CD86 (B7.2) was more efficient than CD80 in this model of AML vaccines. B7.2, the second member of the B7 family costimulatory molecules, has been variously efficacious in a number of murine tumor models.28 31-33 Second, we studied the role of GM-CSF, IL-4, and TNF-α as single cytokine vaccines in murine AML. In this report, we show that vaccination with B7.2-, IL-4–, and TNF-α–AML cells activates tumor-killing mechanisms resulting in rejection of the inoculated leukemic burden, but does not elicit leukemia-specific immunity. GM-AML vaccines, on the other hand, provide potent, long-lasting antitumor immunity and can cure mice with a considerably larger tumor burden than mice cured with B7.1-AML vaccines.
MATERIALS AND METHODS
Mice.
Female SJL/J mice (H-2s), 6 to 8 weeks old, were purchased from Jackson Laboratories (Bar Harbor, ME) or Charles River Laboratories (NCI-Frederick Cancer Research & Development Center, Frederick, MD). Swiss nu/nu mice were purchased from Taconic Laboratories (Germantown, NY). The animals were kept at the animal facility of Dana-Farber Cancer Institute according to the institute's guidelines.
Murine AML model.
The murine AML model used in this study has been previously described.27 Briefly, radiation-induced AML cells34 are maintained by growth in syngeneic SJL/J female mice. Mice injected intravenously (IV) or intraperitoneally (IP) with ≥104 AML develop lethal leukemia in 4 to 5 weeks. In all experiments, freshly isolated or frozen spleen mononuclear cells from leukemic mice (killed just before succumbing to leukemic burden) were used.
Retroviral constructs and producer clones.
A cDNA fragment encoding the entire open reading frame of murine B7.2 was amplified by reverse transcriptase-polymerase chain reaction from total cellular RNA extracted from the murine B-cell line A20 (activated for 24 hours with 4 μg/mL lipopolysaccharide). The B7.2-specific sense and antisense primers had the sequences 5′-ATCGATGAAGCACCCACGATGGAC-3′ and 5′-ATCGATTCACTCTGCATTTGGTTTTGC-3′, respectively.31 The full-length murine B7.2 cDNA was subcloned in sense and antisense (mock virus) orientation at theCla I unique cloning site of the LNCX retroviral vector (kindly provided by Dusty Miller, Fred Hutchinson Cancer Research Center, Seattle, WA). For generating virus producer clones, E-86 packaging cell lines were transfected with LNCX-B7.2 constructs and E86-B7.2-sense or E86-B7.2-antisense clones secreting high titer of virus were used to infect AML cells. E-86-B7.1-sense and E-86-B7.1-antisense producer clones have been previously described.27 Retroviral constructs MFG–GM-CSF,19 MFG–IL-4,19 and murine MFG–TNF-α (Dranoff and Mulligan, unpublished data) and CRIP producer clones, secreting high titers of recombinant retroviruses encoding GM-CSF, IL-4, and TNF-α, have been previously described.19 Empty MFG vector was used for the preparation of mock viruses.
Infection of AML cells.
Infection of AML cells with recombinant viruses has been previously described.27 Briefly, AML cells (5 × 105/mL) were exposed to viral supernatant for 12 to 24 hours in the presence of 8 to 10 μg/mL polybrene and 15% WEHI-3B conditioned media, cultured in fresh media for an additional 24 hours, and then used for in vivo immunizations. In some experiments, a purified population of B7.2-expressing AML cells was used. To purify B7.2+ AML cells, infected cells were stained with a B7.2-specific (GL1) monoclonal antibody (MoAb; PharMingen, San Diego, CA), labeled with goat-antirat IgG Microbeads (Milteny Biotec, Sunnyvale, CA), and selected using magnetic MiniMacs separation columns (Milteny Biotec). Isolated cells were left in culture for 12 to 14 hours and were then used for in vivo immunizations. Flow cytometry analysis (fluorescence-activated cell sorting [FACS]) showed that these cells were greater than 95% pure and appeared to be viable by exclusion of trypan blue and forward/side scatter analysis.
Lymphokine enzyme-linked immunosorbent assays (ELISAs).
Levels of GM-CSF, IL-4, and TNF-α secreted by the infected AML cells cultured for 48 hours at 106 cells/mL were determined using a sandwich ELISA using specific antimurine MoAbs for capture and detection (PharMingen). A color reaction was developed using streptavidin-conjugated horseradish peroxidase (Genzyme, Cambridge, MA), followed by tetramethylbenzidine (TMB) peroxidase substrate (Kirkegaard & Perry Laboratories Inc, Gaithersburg, MD). The MoAbs used for capture and detection were the following: for GM-CSF, purified MP1-22E9 and biotin-conjugated MP1-31G6; for IL-4, purified 11B11 and biotin-conjugated BVD6-24G2; and for TNF-α, purified MP6-XT22 and biotin-conjugated MP6-XT3. Recombinant mouse GM-CSF (rGM-CSF) with a specific activity of 104 U/μg and mouse rIL-4 with a specific activity of 104 U/μg were obtained from PharMingen. Mouse rTNF-α with a specific activity of 2 × 105 U/μg was obtained from Genzyme.
Western blotting.
Total cell lysates from spleen AML cells or control cells were prepared as previously described.35 Ba/F3 cells, transduced with the murine GM-CSF receptor (kindly provided by Bernard Mathey-Prevot, Dana-Farber Cancer Institute), were used as a positive control, and WEHI-3B cells were used as a negative control. Proteins (40 μg of protein/lane) were fractionated by electrophoresis on a 12% sodium dodecyl sulfate (SDS)-polyacrylamide gel and transferred to nitrocellulose membranes for immunoblotting. The membranes were blocked for 1 hour in 5% nonfat dry milk at room temperature and probed with rabbit antiserum against the mouse epitope corresponding to carboxy terminus of GM-CSFRα (Santa Cruz Biotechnology Inc, Santa Cruz, CA) for 45 minutes at room temperature (0.5 μg/mL). The membranes were then incubated in Tris buffered saline, 0.05% Tween-20 (TBST) and horseradish peroxidase-conjugated antirabbit antibody (1:5,000 dilution). Protein bands were detected by use of chemiluminescent techniques according to the manufacturer's instructions (Amersham Life Science, Little Chalfont, UK).
Immunostaining and flow cytometry analysis.
Cells were stained as previously described.27 The following antibodies (PharMingen) were used in this study: CD3 (145-2C11), CD4 (RM4-5), CD8a (53-6.7), αβTCR (H57-597), γδTCR (GL3), Gr-1 (RB6-8C5), CD2 (RM2-5), CD5 (53-7.3), CD18 (C71/16), CD11b (M1/70), CD25 (7D4), CD45 (30F11.1), CD44 (IM7), CD45R/B220 (RA3-6B2), CD54 (3E2), CD62L (MEL-14), CD69 (H1.2F3), CD80 (1G10), CD86 (GL1), and CD95 (Jo2).
In vivo immunization studies.
SJL/J mice or Swiss nu/nu mice were injected IV with live or irradiated (3,200 cGy from a 137Cs source) transduced AML cells (B7.1-, B7.2-, GM-, IL-4–, TNF-α–AML). We have previously shown that irradiation of AML cells with 3,200 cGy abrogates their tumorigenicity.27 In most of the experiments, 105 transduced AML cells were used and diluted in 200 to 300 μL of phosphate-buffered saline.
Statistical analysis.
Most individual experiments consisted of 10 mice per treatment group. The data analyzed represent the results of one or two individual experiments. Cytokine values secreted by transduced AML cells are the mean ± standard error of the mean (SEM).
RESULTS
Infection of AML cells.
AML cells were exposed to E86-B7.2-sense or E86-B7.2-antisense viral supernatants as described in the Materials and Methods. Expression of B7.2 on infected, unselected AML cells was confirmed by surface staining and flow cytometry (Fig 1A). Transduction of AML cells with the MFG-cytokine retroviral constructs resulted in secretion of the gene products and did not alter their in vitro growth characteristics after 3 to 4 days of culture (data not shown). The amount of cytokines produced by cytokine-transduced AML cells (cytokine-AML) was evaluated using specific ELISA assays (Fig1B). The cytokine levels were comparable to production levels reported in other tumor vaccine models. A sample of some recent reports is given in Table 1.36-39 Irradiation of cytokine-AML cells (3,200 cGy) did not abrogate cytokine secretion in vitro for at least 4 days (data not shown). AML cells in this model express the GM-CSF receptor, which is downregulated when the cells are cultured in the presence of IL-3 (Fig 1C), because GM-CSF and IL-3 cross-compete for cellular binding to AML cells.40 41
(A) CD86 expression on infected AML cells. Spleen AML cells were infected with either CD86-sense (a) or CD86-antisense (b) producer clones as described in the Materials and Methods. (□) Control IgG (rat IgG-PE); (▩) CD86-PE (anti-B7.2) MoAb. The hidden portion of the control curve in (a) drops monotonically as a function of fluorescence intensity. (B) Cytokine production by transduced AML cells. Levels of GM-CSF, IL-4, and TNF-α secreted by retrovirally transduced, unselected AML cells cultured for 48 hours at 106 cells/mL were determined by sandwich ELISA using specific antimurine MoAbs for capture and detection. Data are shown as the mean ± SD of six independent experiments. (C) AML cells express GM-CSF receptor. Total cell lysates (40 μg of protein/lane) from spleen AML cells from two different mice (lanes 3 and 4) or control cells (lanes 1 and 5) were fractionated by electrophoresis on a 12% SDS-polyacrylamide gel, transferred to nitrocellulose membrane, and probed with polyclonal antibody against mouse GM-CSFRα as described in the Materials and Methods. AML cells cultured for 24 hours in the presence of IL-3 downregulate GM-CSFR expression (lane 2).
(A) CD86 expression on infected AML cells. Spleen AML cells were infected with either CD86-sense (a) or CD86-antisense (b) producer clones as described in the Materials and Methods. (□) Control IgG (rat IgG-PE); (▩) CD86-PE (anti-B7.2) MoAb. The hidden portion of the control curve in (a) drops monotonically as a function of fluorescence intensity. (B) Cytokine production by transduced AML cells. Levels of GM-CSF, IL-4, and TNF-α secreted by retrovirally transduced, unselected AML cells cultured for 48 hours at 106 cells/mL were determined by sandwich ELISA using specific antimurine MoAbs for capture and detection. Data are shown as the mean ± SD of six independent experiments. (C) AML cells express GM-CSF receptor. Total cell lysates (40 μg of protein/lane) from spleen AML cells from two different mice (lanes 3 and 4) or control cells (lanes 1 and 5) were fractionated by electrophoresis on a 12% SDS-polyacrylamide gel, transferred to nitrocellulose membrane, and probed with polyclonal antibody against mouse GM-CSFRα as described in the Materials and Methods. AML cells cultured for 24 hours in the presence of IL-3 downregulate GM-CSFR expression (lane 2).
B7.2-AML cells have reduced tumorigenicity but do not elicit systemic immunity.
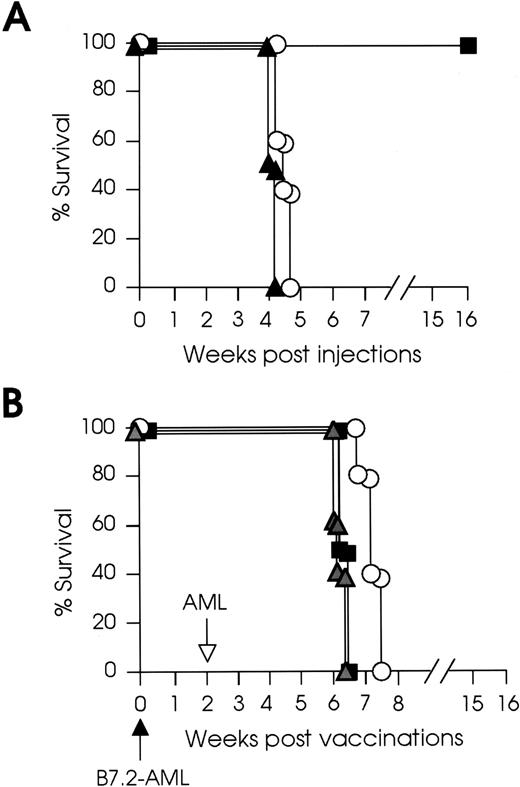
We have previously shown that one IV injection of irradiated B7.1-AML cells can protect mice from subsequent challenge with wild-type AML cells and that one exposure to irradiated, B7.1-AML cells can cure leukemic mice vaccinated up to 1 week after leukemia inoculation (early vaccination), whereas after 2 weeks of leukemic inoculation (late vaccination) the same vaccine only delays tumor growth.27To evaluate the role of B7.2 expression on the leukemic cell growth, mice were injected IV with increasing numbers of live B7.2-AML cells and their clinical outcome was monitored. As shown in Fig2A, mice injected with 105B7.2-AML cells rejected their tumor, whereas mice injected with 106 B7.2-AML cells developed lethal leukemia. Flow cytometry showed a consistent population of AML cells (20% to 25%) not expressing B7.2 after retroviral infection (Fig 1A). Therefore, we tested if mice injected with 5 × 105 purified B7.2-AML cells would reject their leukemia. All mice in this experiment developed lethal leukemia at the expected interval (data not shown). We next examined if immunization with irradiated B7.2-AML cells could elicit systemic immunity and protect mice against subsequent challenge with wild-type AML cells. Mice were immunized with irradiated (3,200 cGy) 105 or 2 × 106 B7.2-AML cells and 2 weeks later were challenged with live 105 wild-type AML cells. As shown in Fig 2B, challenge was lethal to both groups of vaccinated mice, and even vaccinations with as high as 2 × 106 irradiated B7.2-AML cells only prolonged survival for 5 to 7 days.
B7.2-AML cells have reduced tumorigenicity but do not elicit systemic immunity. (A) SJL/J mice (8 to 10 mice for each type of experiment) were injected IV with 105 or 106B7.2-AML cells or 105 control cells. These experiments were repeated twice. Mice injected with (▪) 105 B7.2-AML cells rejected their tumor, whereas mice injected with (○) 106B7.2-AML or (▴) control cells developed lethal leukemia. (B) SJL/J mice were immunized IV with (▪) 105 irradiated (3,200 cGy) B7.2-AML or (○) 2 × 106 B7.2-AML cells or (▵) control cells (solid arrow) and 2 weeks later challenged with 105 live wild-type AML cells (open arrow). Challenge was lethal to all groups of vaccinated mice. Vaccinations with 2 × 106 irradiated B7.2-AML cells prolonged survival for 5 to 7 days.
B7.2-AML cells have reduced tumorigenicity but do not elicit systemic immunity. (A) SJL/J mice (8 to 10 mice for each type of experiment) were injected IV with 105 or 106B7.2-AML cells or 105 control cells. These experiments were repeated twice. Mice injected with (▪) 105 B7.2-AML cells rejected their tumor, whereas mice injected with (○) 106B7.2-AML or (▴) control cells developed lethal leukemia. (B) SJL/J mice were immunized IV with (▪) 105 irradiated (3,200 cGy) B7.2-AML or (○) 2 × 106 B7.2-AML cells or (▵) control cells (solid arrow) and 2 weeks later challenged with 105 live wild-type AML cells (open arrow). Challenge was lethal to all groups of vaccinated mice. Vaccinations with 2 × 106 irradiated B7.2-AML cells prolonged survival for 5 to 7 days.
Finally, we examined whether B7.2-AML cells could rescue leukemic mice with very small leukemic burden. Mice were injected with 104 AML cells (lowest tumorigenic number) and immunized 2 days later with live or irradiated 105 B7.2-AML cells. All mice in this experiment developed lethal leukemia after 5 weeks (data not shown). Taken together, these results show that, in this AML model, expression of B7.2 on the AML cells can initiate significant tumor-killing mechanisms, thus reducing their tumorigenicity. However, B7.2-AML cells (at least the numbers used in this study) do not induce protective or therapeutic immunity.
Tumorigenicity and immunogenicity of cytokine-AML cells.
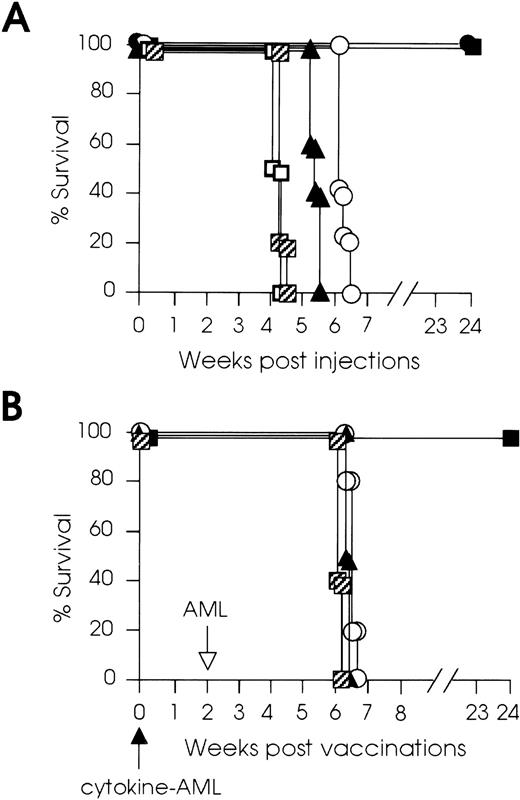
To evaluate if cytokine gene transduction of AML cells would have any effect on their tumorigenicity and immunogenicity, groups of mice were injected with live 105 to 106 GM-AML, IL-4–AML, or TNF-α– AML cells or with mock-infected control AML cells. Mice did not develop any signs of toxicity and only mice injected IV with live 105 to 106 GM-AML cells developed a transient increase of the white blood cell count (up to 18 × 103/μL, from the normal 10 to 12 × 103/μL), between weeks 2 and 3 after tumor inoculation. All mice inoculated with 105 cytokine-AML (GM-, IL-4–, or TNF-α–AML) cells rejected their tumors (Fig3A). From the groups of mice inoculated with live 106 cells, only the GM-AML group rejected the leukemic cells, whereas IL-4–AML— or TNF-α–AML—injected mice only had prolonged survival for 1 to 2 weeks (Fig 3A).
Tumorigenicity and immunogenicity of cytokine-AML cells. (A) SJL/J mice (8 to 10 mice for each type of experiment) were injected IV with 105 or 106 live GM-AML, IL-4–AML, or TNF-α–AML cells (cytokine-AML). Control mice were injected with 105 or 106 mock-infected AML cells. All mice injected with 105 cytokine-AML (•) and 106GM-AML cells (▪) rejected their leukemia. Mice injected with 105 (▨) or 106 (□) control cells developed leukemia at the expected interval. Mice injected with 106IL-4–AML (▴) had 1 week and those injected with 106TNF-α–AML cells (○) had 2 weeks of prolonged survival. (B) SJL/J mice (8 to 10 mice for each type of experiment) were vaccinated IV (solid arrow) with 105 irradiated (3,200 cGy) GM-AML (▪), IL-4–AML (▴), or TNF-α–AML cells (○) or mock-infected control cells (▨) and were challenged 2 weeks later (open arrow) with 105 live wild-type AML cells. GM-AML–vaccinated mice survived tumor challenge, whereas challenge was lethal to all other groups of mice.
Tumorigenicity and immunogenicity of cytokine-AML cells. (A) SJL/J mice (8 to 10 mice for each type of experiment) were injected IV with 105 or 106 live GM-AML, IL-4–AML, or TNF-α–AML cells (cytokine-AML). Control mice were injected with 105 or 106 mock-infected AML cells. All mice injected with 105 cytokine-AML (•) and 106GM-AML cells (▪) rejected their leukemia. Mice injected with 105 (▨) or 106 (□) control cells developed leukemia at the expected interval. Mice injected with 106IL-4–AML (▴) had 1 week and those injected with 106TNF-α–AML cells (○) had 2 weeks of prolonged survival. (B) SJL/J mice (8 to 10 mice for each type of experiment) were vaccinated IV (solid arrow) with 105 irradiated (3,200 cGy) GM-AML (▪), IL-4–AML (▴), or TNF-α–AML cells (○) or mock-infected control cells (▨) and were challenged 2 weeks later (open arrow) with 105 live wild-type AML cells. GM-AML–vaccinated mice survived tumor challenge, whereas challenge was lethal to all other groups of mice.
We next examined if vaccinations of mice with irradiated cytokine-AML cells could elicit systemic immunity. Groups of mice were immunized with irradiated 105 cytokine-AML (GM-, IL-4–, or TNF-α–AML) cells and were challenged 2 weeks later with 105 live wild-type AML cells. As shown in Fig 3B, only GM-AML–vaccinated mice developed protective immunity and survived the tumor challenge, whereas the challenge was lethal to all mice immunized with IL-4–AML or TNF-α–AML cells. To determine whether higher numbers of irradiated IL-4– or TNF-α–AML cells could elicit protective immunity, the same experiments were repeated with irradiated 2 × 106 IL-4– or TNF-α–AML cells. All animals in these experiments succumbed to subsequent challenge with 105 live wild-type AML cells (data not shown). These results clearly show variability in the efficacy of the 3 different cytokine vaccines in the same AML model. Whereas significant tumor-cell killing mechanisms appear to follow each of the cytokine vaccines at low tumor cell doses (Fig 3A), the ability to elicit protective immunity is restricted to GM-AML cells (Fig 3B).
Rejection of GM-AML cells is not T-cell–dependent.
In an attempt to confirm that 105 GM-AML cells were as leukemogenic as wild-type AML cells, we injected Swiss nu/nu mice with 105 GM-AML or mock-infected cells. We have previously shown that 105 B7.1-AML cells are equally as tumorigenic as wild-type AML cells in these mice. Surprisingly, all nude mice injected with GM-AML cells remained healthy and tumor-free, whereas mice injected with control cells developed leukemia (Fig4). This clinical outcome indicated that either 105 GM-AML cells had lost their tumorigenicity or effector cells other than T cells were responsible for their rejection in nude mice. To address this question, we irradiated SJL/J mice (600 cGy TBI) and injected them 2 days later with 105 GM-AML or wild-type AML cells. Both groups of irradiated SJL/J mice developed lethal leukemia, clearly indicating that 105 GM-AML were equally leukemogenic as wild-type AML cells (Fig 4).
Rejection of GM-AML cells is not T-cell–dependent. (A) Swiss nu/nu mice, in groups of 6, were injected IV with 105GM-AML cells (□) or 105 mock-infected control cells (•). The former group rejected their tumor, whereas the latter group developed lethal leukemia. (B) SJL/J mice, in groups of 6, were irradiated (600 cGy TBI) and injected 2 days later with 105GM-AML cells (○) or mock-infected control cells (▵). Both groups of SJL/J mice developed lethal leukemia.
Rejection of GM-AML cells is not T-cell–dependent. (A) Swiss nu/nu mice, in groups of 6, were injected IV with 105GM-AML cells (□) or 105 mock-infected control cells (•). The former group rejected their tumor, whereas the latter group developed lethal leukemia. (B) SJL/J mice, in groups of 6, were irradiated (600 cGy TBI) and injected 2 days later with 105GM-AML cells (○) or mock-infected control cells (▵). Both groups of SJL/J mice developed lethal leukemia.
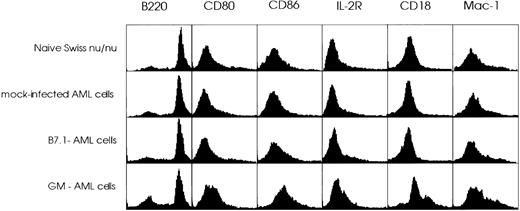
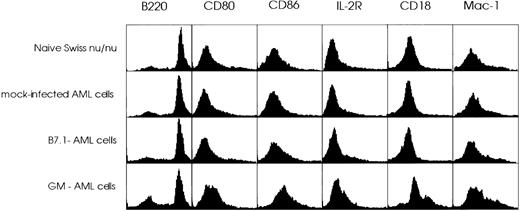
We next examined if we could detect by flow cytometry any cell population changes in the spleens of nude mice that reject GM-AML cells. Swiss nu/nu mice were injected with live GM-AML or B7.1-AML cells (previously shown to be leukemogenic). Control mice were injected with mock-infected AML cells. The spleens were removed 3 days later, and spleen mononuclear cells were stained with the MoAbs described in the Materials and Methods directed against a wide range of hematopoietic subsets. There were no differences observed for 14 of 20 surface markers studied (including the T-cell markers CD3, CD4, and CD8 that were negative) between naive and experimental mice. However, GM-AML–injected mice showed an increased expression of CD80, CD86, IL-2R, CD18, and Mac-1. In addition, a larger population of cells (25.31% v 18.51% in naive mice) was negative for the B-cell–specific marker B220 (Fig 5). These data clearly show that injection of nude mice with GM-AML cells leads to an influx of non-B cells in the spleen of the animals. Most likely, the majority of these cells are of myeloid-monocytic origin, expressing APC/monocytic activation markers such as CD80, CD86, and IL-2R.
FACScan analysis of spleen cells from Swiss nu/nu mice. Swiss nu/nu mice, in groups of 3, were injected IV with live 105 GM-AML or B7.1-AML or mock-infected AML cells. Three days later, their spleen cells were stained with a panel of 20 MoAb as described in the Materials and Methods and compared with spleen cells from naive Swiss nu/nu mice. A total of 10,000 cells were analyzed by FACS for each sample. GM-AML–injected mice showed a higher population of cells negative for B220 (25.31% v 18.51% in naive mice) and increased expression of CD80, CD86, IL-2R, CD18, and Mac-1.
FACScan analysis of spleen cells from Swiss nu/nu mice. Swiss nu/nu mice, in groups of 3, were injected IV with live 105 GM-AML or B7.1-AML or mock-infected AML cells. Three days later, their spleen cells were stained with a panel of 20 MoAb as described in the Materials and Methods and compared with spleen cells from naive Swiss nu/nu mice. A total of 10,000 cells were analyzed by FACS for each sample. GM-AML–injected mice showed a higher population of cells negative for B220 (25.31% v 18.51% in naive mice) and increased expression of CD80, CD86, IL-2R, CD18, and Mac-1.
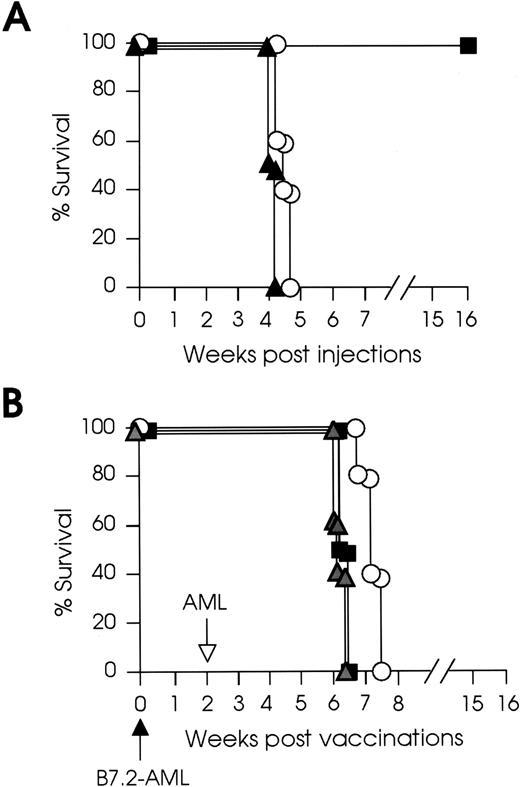
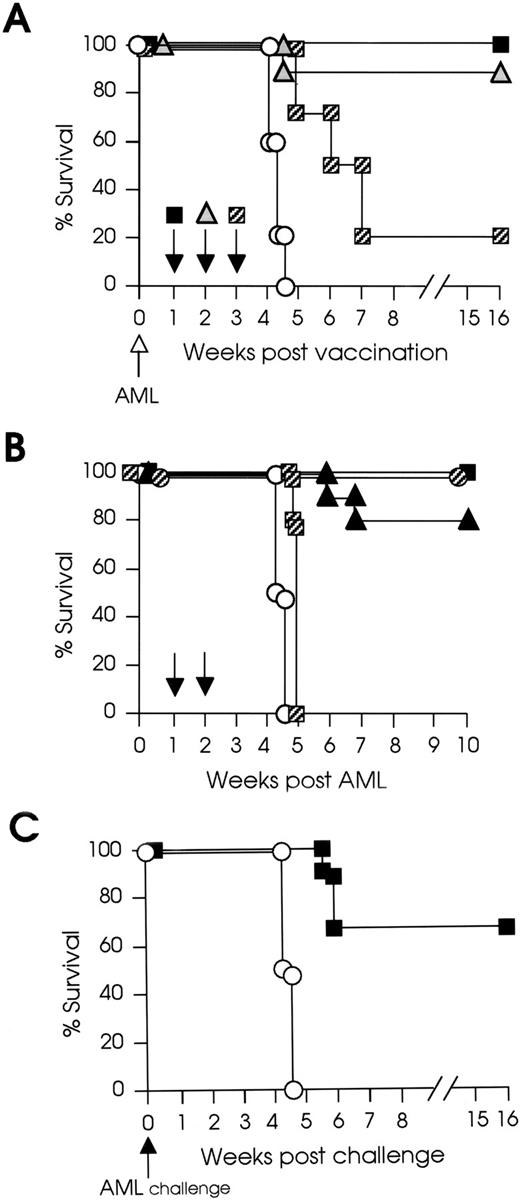
GM-AML vaccines cure mice with larger tumor burden than B7.1-AML vaccines and elicit leukemia-specific memory cells. Experiments were designed to evaluate the effectiveness of different cytokine vaccines in leukemic mice and to compare them with B7.1-AML vaccines that can only cure mice with small (1 week) leukemic burden.27 Mice were inoculated with 105wild-type AML cells and 1 week later were immunized with irradiated 105 GM-, IL-4–, or TNF-α–AML cells. All mice vaccinated with IL-4–AML or TNF-α–AML cells developed lethal leukemia at the expected interval (data not shown), whereas 100% of mice vaccinated with irradiated GM-AML rejected their tumor. We then examined if GM-AML vaccines administered 2 or 3 weeks after tumor inoculation were able to rescue mice from lethal leukemia. In this experiment, 90% of mice vaccinated at week 2 and 20% of mice vaccinated at week 3 rejected their leukemia and remained tumor-free for an observation period of 4 months (Fig 6
A). To directly compare the effectiveness of B7.1-AML and GM-AML vaccines in this model, we performed a head-to-head comparison of the vaccines in the same experiment. Mice were injected with 105 AML cells and 1 or 2 weeks later they were vaccinated with irradiated 105B7.1-AML or GM-AML cells; nonvaccinated leukemic mice and leukemic mice injected with mock-infected AML cells were used as control. All mice vaccinated at week 1 with either B7.1-AML or GM-AML cells rejected their leukemia. Vaccinations with B7.1-AML cells at week 2 had no effect on survival and 100% of the mice developed lethal leukemia. On the contrary, vaccinations with GM-AML cells at week 2 resulted in 80% cure and 20% prolonged survival of leukemic mice (Fig 6B). These results clearly show that, in the SJL/J AML model, GM-AML vaccines provide more potent antileukemia immunity than do B7.1-AML vaccines. In an attempt to investigate if leukemia rejection by SJL/J mice involved immune mechanisms leading to leukemia-specific memory, mice that had been rescued by week 2 GM-AML vaccines were challenged 4 months later with 105 wild-type AML cells. This experiment showed that 67% of the mice had developed immunologic memory that enabled them to survive the AML challenge (Fig 6C).
GM-AML vaccines cure mice with larger tumor burden than B7.1-AML vaccines and elicit leukemia-specific memory cells. (A) SJL/J mice were inoculated with live 105wild-type AML cells (open arrow). One (▪), 2 (▵), or 3 weeks (▨) later (10 mice per group), they were immunized with 105irradiated (3,200 cGy) GM-AML cells. Five control mice (○) were not vaccinated after leukemia inoculation. (B) Mice were inoculated with live 105 wild-type AML cells, and 1 or 2 weeks (solid arrows) later, they were immunized with 105 irradiated GM-AML or B7.1-AML cells (10 mice per group). Nonvaccinated leukemic mice and leukemic mice injected with mock-infected AML cells were used as control (○). All mice vaccinated at week 1 with either B7.1-AML (○) or GM-AML (▪) cells rejected their leukemia. All mice vaccinated at week 2 with B7.1-AML (▨) cells developed lethal leukemia. Vaccinations with GM-AML cells at week 2 (▴) resulted in 80% cure and 20% prolonged survival. (C) SJL/L mice (9 mice) that had been rescued by week 2 GM-AML vaccine were challenged 4 months later with 105 wild-type AML cells (solid arrow). Six of nine vaccinated mice (67%; ▪) survived the challenge with AML cells. Control mice (○) developed lethal leukemia.
GM-AML vaccines cure mice with larger tumor burden than B7.1-AML vaccines and elicit leukemia-specific memory cells. (A) SJL/J mice were inoculated with live 105wild-type AML cells (open arrow). One (▪), 2 (▵), or 3 weeks (▨) later (10 mice per group), they were immunized with 105irradiated (3,200 cGy) GM-AML cells. Five control mice (○) were not vaccinated after leukemia inoculation. (B) Mice were inoculated with live 105 wild-type AML cells, and 1 or 2 weeks (solid arrows) later, they were immunized with 105 irradiated GM-AML or B7.1-AML cells (10 mice per group). Nonvaccinated leukemic mice and leukemic mice injected with mock-infected AML cells were used as control (○). All mice vaccinated at week 1 with either B7.1-AML (○) or GM-AML (▪) cells rejected their leukemia. All mice vaccinated at week 2 with B7.1-AML (▨) cells developed lethal leukemia. Vaccinations with GM-AML cells at week 2 (▴) resulted in 80% cure and 20% prolonged survival. (C) SJL/L mice (9 mice) that had been rescued by week 2 GM-AML vaccine were challenged 4 months later with 105 wild-type AML cells (solid arrow). Six of nine vaccinated mice (67%; ▪) survived the challenge with AML cells. Control mice (○) developed lethal leukemia.
DISCUSSION
In this report we expanded our studies on gene immunotherapy in a primary murine AML model. Our previous work has shown that leukemia growth per se does not induce T-cell unresponsiveness or a Th2 cytokine profile and that B7.1-AML vaccines can cure leukemic mice without a large leukemic burden. We investigated here the possibility of using either B7.2- or cytokine-transduced AML cells (GM-CSF, IL-4, and TNF-α) as more effective vaccines. Our results clearly show that, in this AML experimental model, there is dissociation between tumor-killing and vaccine-induced tumor immunity and that, from the molecules studied, only GM-CSF can cure leukemic mice with considerable leukemic burden and elicit protective memory immune responses. Furthermore, we show that the antitumor activity of GM-CSF is present in nude mice, indicating that cell populations other than T cells are involved in GM-AML cell elimination. Several questions arise from our data. (1) Why are tumor-cell–induced B7.1 and B7.2 costimulatory signals different in the same AML model, in that B7.2 is not inducing T-cell–mediated antileukemia protective and therapeutic immunity? (2) Why are IL-4– and TNF-α–AML cells ineffective in providing antileukemia immunity? (3) Why can GM-CSF vaccines fight a larger tumor burden than B7.1-AML vaccines? (4) Why do not all GM-CSF–vaccinated leukemic mice develop antileukemia memory?
There is increasing evidence that the two-signal axiom does not completely cover the complex process of T-cell activation and that CD28 ligation is not necessary for initial T-cell activation and proliferation but is required for cell survival.42-44Indeed, a sequential multiple-step model for T-cell activation has been proposed.45 According to this model, primary costimulatory signals can be delivered by several adhesion and costimulatory molecules, and continued and prolonged B7/CD28 interaction leads to optimal T activation by inducing cytokine gene transcription and cytokine mRNA stabilization.44-46 These observations support our reported data that AML growth induces activation of T cells in the initial stages of leukemia, despite the fact that AML cells in the SJL/J model do not express B7 family costimulatory molecules.30 Another recently reformed concept is that, although the costimulatory molecules B7.1 and B7.2 both bind to CD28 and CTLA-4, their binding with these receptors mediates distinct biologic functions.43,44 As opposed to the widely demonstrated positive effect of CD28 ligation in T-cell activation and survival, it has been reported that CTLA-4 costimulation delivers downregulatory signals, either by inhibiting signaling through the TCR,47 provoking an active CTLA-4–mediated apoptotic death,48 or by inducing cell cycle arrest in G1/G0.49 It has also been reported that, although B7.1 and B7.2 have the same high affinity for CTLA-4, this receptor on T cells may have a differential response to B7.1 and B7.2 ligation.50,51 However, these differences between the two costimulatory molecules cannot directly address the question as to why B7.1 costimulation, when provided by engineered tumor cells, is superior to B7.2 in several tumor models. It has been hypothesized that B7.2 costimulation may promote a Th2-type cytokine profile of T cells.28,52 In studies comparing immune parameters of mice vaccinated with various types of vaccines, we could not confirm a Th2 cytokine profile in B7.2-AML–vaccinated mice (K. Dunussi-Joannopoulos, unpublished data). Moreover, it has been recently shown that B7.1 and B7.2 do not appear to selectively regulate Th1 versus Th2 differentiation.53 In the SJL/J AML model, B7.1-AML costimulation is capable of eliciting leukemia-specific immunity and leukemia-specific memory CTLs, whereas B7.2-AML costimulation is not providing protective or therapeutic antileukemia immunity. We speculate that the differential clinical outcome mirrors a positive B7.1/CD28 signal, leading to clonal CTL expansion, and a negative B7.2/(CTLA-4?) signal resulting in absence (elimination?) of leukemia-specific T-cell responses. A recent report that treatment of mice with CTLA-4 MoAb prevented tumor outgrowth and induced the regression of established tumors54 strongly suggests that, at least in tumor models, a negative signal mediated by CTLA-4 plays a more decisive role than a positive signal mediated by CD28. However, this phenomenon still suffers from lack of cellular and structural detail.
Another issue for discussion is the efficacy of cytokine gene immunotherapy in murine AML. Studies in murine, mostly nonhematopoietic, tumor models have shown that certain cytokines produced by genetically engineered tumor cells lead to decreased tumorigenicity and increased immunogenicity of the transduced tumor cells.15-19 A variety of cytokines have been described that augment host antitumor immunity. We show that secretion of the cytokines GM-CSF, IL-4, or TNF-α in this AML model is each able to initiate immune responses that inhibit the in vivo growth of transduced AML cells. However, the desirable clinical outcome of tumor vaccines, ie, recruitment of tumor-specific protective and therapeutic immunity, was only achieved with GM-CSF gene immunotherapy, which suggests that tumor growth inhibition and antitumor immunity may be mediated by different cell populations in cytokine tumor models.55Activated natural killer cells, macrophages, neutrophils, and eosinophils may be involved in direct killing of cytokine-AML cells, as shown by GM-AML cell experiments. Rejection of GM-AML cells in Swiss nude mice correlates with detection of a non-B–cell splenic population expressing myeloid and activated monocytic/APC surface markers, confirming that T cells are not necessary for tumor rejection. Participation of both innate and T-cell–mediated immunity in GM-CSF immunotherapy may partially explain its superiority as compared with B7.1-AML vaccines in this experimental AML model. On the contrary, the lack of immunogenicity of the IL-4– or TNF-α–AML cells (at least the numbers used in this study) suggests that the cytokines released by transduced cells may initiate rapid tumor clearance mechanisms, possibly resulting in limited loading of APCs with tumor antigen(s) and ineffective priming of leukemia-specific CTLs.21Alternatively, mechanisms of T-cell immunosupression may govern this outcome. We are currently investigating immune parameters in cytokine-AML–vaccinated mice and the role of combined cytokine gene immunotherapy in the SJL/J AML model.
The introduction of the hematopoietic cytokine GM-CSF into treatment regimens for AML raised concerns several years ago, because it was well established that AML progenitor cells require hematopoietic growth factors (HGF) for survival and proliferation,56,57 although they usually show little maturation under the influence of these regulators.58 The demonstration in the early 1990s that HGF could shorten the duration of neutropenia after intensive chemotherapy for solid tumors provoked the introduction of GM-CSF and G-CSF into AML clinical trials.8 GM-CSF has been used in three general clinical situations in AML: for attenuation of neutropenia, for sensitization of leukemic cells to cytotoxic therapy, and for the induction of terminal differentiation of leukemic cells.4,8The conclusions from numerous clinical trials that have been conducted during the last years are still debatable.4 However, most importantly, early concerns about a possible proliferation of the blasts have not been confirmed.4 8
Several recent studies on tumor models have shown that GM-CSF gene immunotherapy is highly therapeutic.37,59-61 Based on our data on the AML model, a two-step use for GM gene immunotherapy in AML is feasible. First, administration of GM-CSF transduced AML cells during induction as a substitute for the systemic cytokine administration. GM-CSF secretion by AML cells in the bone marrow microenvironment will address the issue of dose limitations raised by the toxic effects of systemic cytokine administration.8When patients are in remission having minimal residual disease, an additional dose(s) of GM-AML vaccines will need to be administered to achieve therapeutic benefits mediated by the immune system. However, certain concerns arise from our observation that long-lasting antileukemia memory was not maintained by all vaccinated mice. Model systems in which the fate of tumor-specific T cells can be monitored in vivo, with or without the presence of tumor antigen(s), would greatly enhance our understanding of tumor-related memory immunity. It may turn out to be necessary that gene immunotherapy-treated patients will need boosts with irradiated, wild-type tumor cells to secure the longevity of tumor-specific immunity.
Supported in part by the Andrew F. Gaffney Foundation.
Address reprint requests to Kyriaki Dunussi-Joannopoulos, MD, PhD, Genetics Institute, 1 Burrt Rd, Andover, MA 01810.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.