Abstract
Fifty-one transfusion-dependent iron-loaded adult patients (38 with thalassemia major) were treated with the orally active iron chelator deferiprone (1,2 dimethyl-3-hydroxypyrid-4-one, L1) at a dose of 75 mg/kg/d (range, 50 to 79). Twenty patients discontinued the drug and five died after a mean of 18.7 months (range, 4 to 35). Of the 20, 5 had arthropathy, 5 had gastrointestinal symptoms, 4 had a rising serum ferritin, 3 had agranulocytosis or neutropenia, 1 had tachycardia, 1 had renal failure, and 1 went abroad. Twenty-six patients continued deferiprone for a mean of 39.4 months (range, 12 to 49). Among these patients, there was no overall significant change in serum ferritin (initial mean, 2,937 μg/L; range, 980 to 5,970; final mean, 2,323 μg/L; range, 825 to 5,970) or in urine iron excretion (initial mean, 31.2 mg/24 h; range, 16.3 to 58.2; final mean, 32.1 mg/24 h; range, 9.4 to 75.8), implying no overall change in iron stores. When the patients who had received deferiprone for longer than 3 years were considered separately, there was also no significant change in serum ferritin or urinary iron excretion. The initial serum ferritin levels in the 26 patients who continued deferiprone treatment were significantly lower than in those who discontinued the drug (P < .01). The liver iron content in 17 patients who had received deferiprone for 24 to 48 months ranged from 5.9 to 41.2 mg/g dry weight, 50% having levels above 15.0 mg, a level associated with a high risk of cardiac disease due to iron overload. In this study the drug caused fewer side effects and was more effective at maintaining iron status among patients previously well chelated and with lower initial serum ferritin levels.
ONLY ONE DRUG, deferoxamine mesylate (DFX), is widely available for chelating iron from patients with refractory anemias, such as thalassemia major, who require regular blood transfusions. Iron accumulates in such patients at a rate of about 0.5 mg/kg/d and subcutaneous DFX 20 to 50 mg/kg/d administered over 8 to 12 hours is sufficient to produce iron balance in most of these patients with a body iron burden about 5 to 10 times the normal level.1 DFX is unavailable to many patients worldwide because it is too expensive; also, patients may develop local or generalized sensitivity to the drug or may develop toxic side effects such as growth failure, deformities of the long bones and spine, and hearing and visual problems. These side effects occur, however, largely in patients administered excessive doses of DFX in the face of low iron burden. Many patients find difficulty in complying with daily subcutaneous DFX therapy, which is burdensome, painful, and time-consuming. Noncompliance becomes a major problem, particularly in adolescents, leading to iron induced cardiac damage and death.2,3 Calcium diethylenetriamine penta-acetic acid has been used as an alternative to DFX but it also has to be administered parenterally and it causes excessive zinc excretion. A potential orally active alternative to DFX is 1,2-dimethyl-3-hydroxypyrid-4-one (L1, deferiprone). Short-term clinical studies have shown the drug to be effective but to have toxic side effects including agranulocytosis, arthropathy, zinc deficiency, and gastrointestinal side effects.4-7 We now report the efficacy and side effects of deferiprone in a long-term trial of therapy in 51 transfusion-dependent patients.
MATERIALS AND METHODS
Fifty-one iron-overloaded regularly transfused patients who were unable to take DFX or not compliant with DFX were included in the trial. Thirty-eight patients (36 splenectomized) had β-thalassemia major (TM), 1 had hemoglobin E/beta thalassemia, and 1 had sickle cell/β-thalassemia. This group included 13 women and 27 men, mean age of 30.5 years (range, 22 to 38). Additional patients included 4 with sickle cell anemia (2 women, 32 and 63 years and 2 men, 18 and 32 years), 3 with sideroblastic anemia (1 woman, 46 years and 2 men, 16 and 45 years), and 4 men with myelodysplastic syndrome, mean age of 71.5 years (range, 58 to 83).
The 36 splenectomized TM patients were administered transfusions of red blood cells (RBCs) 3 to 4 U monthly to raise their hemoglobin (Hb) levels from 9.0 to 15.0 g/dL; overall yearly mean of Hb was 12.0 g/dL. Their blood consumption ranged from 150 to 200 mL/kg/body weight of RBCs per year. Two nonsplenectomized TM patients required 250 to 300 mL/kg/body weight of RBCs per year. Patients with sickle cell/β-thalassemia required 260 mL/kg/body weight of RBCs per year to achieve an Hb S concentration of less than 30%. In one patient with Hb E/β-thalassemia the Hb level ranged from 7 to 12.0 g/dL, the patient requiring only 120 mL/kg/body weight of RBCs per year. In the 11 nonthalassemic patients, RBC requirements were similar to those of nonsplenectomized thalassemic patients. Deferiprone was administered orally in a total daily dose of 75 mg/kg/body weight (range, 50 to 79 mg/kg) at least an hour before food every 8 to 12 hours. Deferiprone was manufactured according to published methods and marketed by Lipomed (Basel, Switzerland) and Vitra (Clavering, Essex, UK) Pharmaceutical Companies. The study was approved by the Ethical Committees of the Royal Free and Whittington Hospitals and exemption from license certificate was obtained from the Medical Control Agency, London, UK. Written informed consent was obtained from each patient.
At each monthly visit detailed clinical examination was performed and laboratory tests included full blood count, liver and renal function, serum zinc and calcium levels, serum immunoglobulins, CD4/CD8 lymphocyte numbers and ratio, and antinuclear and rheumatoid factor. Leukocyte ascorbic acid was measured every six months in all patients and those with low levels were given oral vitamin C (200 mg/d) with their daily dose of deferiprone. Urine zinc excretion was measured every three months. The patients were monitored for side effects; in particular, musculoskeletal complaints were noted and joints were carefully examined for warmth, crepitus, synovial swelling, effusion, and by the patellar compression test for retropatellar tenderness and stability. Special investigations of the painful joints included plain x-ray, magnetic resonance imaging, and isotope bone scans. Cardiac function was monitored by annual multiple uptake gated acquisition (MUGA) scans of the heart, and measuring the left ventricular ejection fraction at rest and under stress. Compliance to deferiprone was not assessed by computerized containers but we checked that patients had used up supplies and new prescriptions were administered with only a sufficient amount of drug until the next appointment.
We assessed the efficacy of deferiprone treatment by monthly measurements of serum ferritin concentration and of 24-hour urinary iron excretion. In 17 patients on long-term deferiprone (mean, 39.4 months; range, 24 to 48) hepatic iron concentrations were measured, using chemical analysis of tissue iron obtained by liver biopsy.8
RESULTS
Patients withdrawn from long-term therapy.
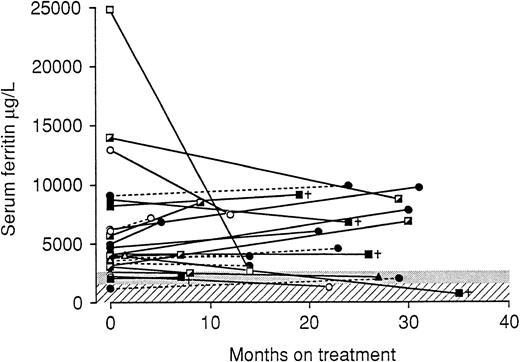
Of the 51 patients, 25 (49%) discontinued deferiprone or died after a mean of 18.7 months (range, 4 to 35). The reasons for stopping treatment in 20 of the patients are shown in Table1. All five patients with arthropathy had TM. Their mean serum ferritin levels at the start of deferiprone treatment was 4,192 μg/L (range, 1182 to 9060). Arthropathy caused discontinuation of deferiprone during the second or third year of therapy. Joint symptoms had usually been present for several weeks and in these cases did not improve with lowering the dose of deferiprone to 50 mg/kg/d. The knee joints were mainly affected and the clinical symptoms were of stiffness, crepitus, and effusion. Special tests including plain radiography, magnetic resonance imaging, and isotope scans were unhelpful in elucidating the pathophysiology of the arthropathy. There was no correlation between the presence of antinuclear factor (ANF) and rheumatoid factor antibodies in the plasma of these patients suffering from arthropathy compared with those without. There was also no statistical significant difference between serum ferritin levels between the two groups.
Four TM patients stopped deferiprone treatment because of rising serum ferritin levels. Their mean initial serum ferritin level of 4,925 μg/L had increased to 7,569 μg/L. The mean urinary iron excretion in these four patients was 9.1 mg/24 h (range, 5.6 to 18.5). Their blood consumption was not significantly different from that of the other TM patients. One 63-year-old myelodysplastic patient developed agranulocytosis after 6 weeks of deferiprone therapy (79 mg/kg/d). Details of this patient have been reported elsewhere.9 His neutrophil count recovered after 7 days. Two TM patients developed neutropenia (<1.5 × 109/L) after 13 and 22 months of therapy. Both were administered a much lower dose of deferiprone but developed a second decrease in neutrophils which recovered on stopping deferiprone therapy.9 Severe gastrointestinal symptoms such as nausea, anorexia, or vomiting necessitated the discontinuation of deferiprone therapy in five patients. Two of these patients had poor renal function; one with sickle cell anemia and chronic glomerulonephritis; the other with myelodysplasia was 82 years old.
Fatalities during the study.
Five patients died, four of congestive heart failure due to iron overload. Their mean serum ferritin at the time of death was 5,112 μg/L (range, 2,100 to 9,060) (Table 2). The fifth patient died of adult respiratory distress syndrome. She had received deferiprone for 35 months and her serum ferritin level at the time of death was 720 μg/L. None of these patients had neutropenia. The 23-year-old male patient with TM and diabetes mellitus died of bronchopneumonia and cardiac failure. Four months before his death deferiprone treatment was stopped and an attempt was made to reintroduce subcutaneous DFX with poor compliance. The initial MUGA scan showed moderately severe cardiomyopathy with a left ventricular ejection fraction (LVEF) of 55% at rest and 40% on cold stress, and 2 years later (2 months before he died), LVEF was 54% decreasing to 42% on cold stress.
The 24-year-old female patient with TM and diabetes mellitus was admitted to the hospital with high fever, and septicemia was diagnosed. Her cardiac condition rapidly deteriorated and she died of heart failure secondary to iron overload. The MUGA scan remained unchanged, showing moderately severe cardiomyopathy initially with an LVEF of 48% at rest and 40% on cold stress, a year later with an LVEF of 46% at rest and 40% on cold stress.
The 30-year-old male thalassemia patient, noncompliant to DFX, with diabetes mellitus, gonadal failure, and hypothyroidism, was taken off deferiprone treatment 4 months before his death. He was admitted with a short history of breathlessness and irregular heart beat. His cardiac condition rapidly deteriorated despite continuous intravenous DFX treatment and he died of congestive heart failure. His MUGA scan did not show deterioration from a moderately severe cardiomyopathy on routine yearly testing, initially LVEF 51% at rest falling to 43% on stress and at 2 years, 49% at rest falling to 41%.
The 48-year-old patient with congenital sideroblastic anemia had taken deferiprone irregularly for 2 months before he died because of anorexia, nausea, and joint pains. He contracted an infection and 2 days before he died, developed cardiac failure. His MUGA scan, which initially showed moderately severe cardiomyopathy (LVEF 60% at rest decreasing to 52% on stress), had remained consistent throughout the study. He had shown pulmonary hypertension with pulmonary artery systolic pressure of 99 mm Hg and concentric left and right ventricular hypertrophy.
Patients continuing to take deferiprone.
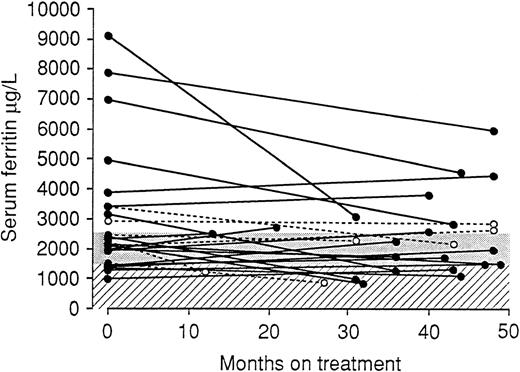
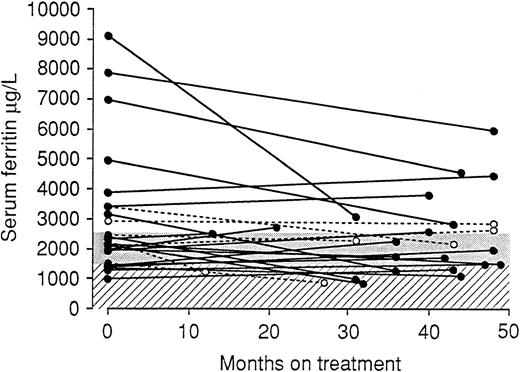
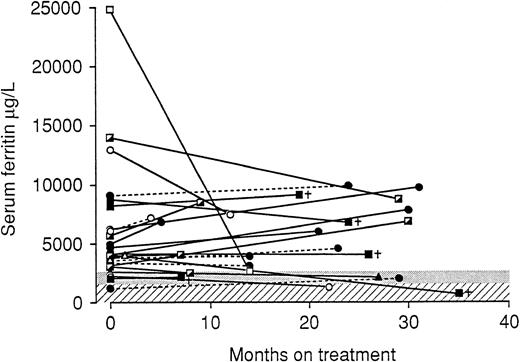
Twenty-six patients (20 TM, 1 sickle cell anemia, 1 sickle/β-thalassemia, 1 Hb E/β-thalassemia, 2 sideroblastic anemia, and 1 myelodysplastic syndrome) have taken deferiprone for a mean of 39.4 months (range, 12 to 49). We have analyzed RBC consumption in milliliters per kilogram per year for the 26 patients whose serum ferritin levels are given in Fig1. There was no significant correlation between RBC consumption and initial or final serum ferritin or with the liver iron levels in 17 patients (see Fig 3). The initial mean serum ferritin level was 2,937 μg/L (range, 980 to 9,090) and at the end of the study 2,323 μg/L (range, 825 to 5,970), with no significant change (Fig 1). Fifteen patients have taken deferiprone for more than 36 months without significant change in serum ferritin and urine iron excretion. Among the 17 patients with initial serum ferritin levels less than 2,500 μg/L, three rose to above this level. In the remaining nine patients serum ferritin levels initially ranged from 2,920 to 9,090 μg/L. In all but one patient final values were still above 2,500 μg/L (range, 1,250 to 5,972). The initial serum ferritin levels in these 26 patients were significantly lower than in the 25 patients who died or discontinued deferiprone, mean, 5,095 μg/L (range, 2,170 to 13,900) (P < .01) (Fig2), or than in the 20 patients who discontinued deferiprone considered alone (P < .01).
The initial and final serum ferritin concentrations in 26 patients who continue deferiprone therapy for a mean of 39.4 (range, 12 to 49) months. (○), Chronic liver disease caused by hepatitis C; threshold of effective treatment: (▧), USA; (▨), WHO.
The initial and final serum ferritin concentrations in 26 patients who continue deferiprone therapy for a mean of 39.4 (range, 12 to 49) months. (○), Chronic liver disease caused by hepatitis C; threshold of effective treatment: (▧), USA; (▨), WHO.
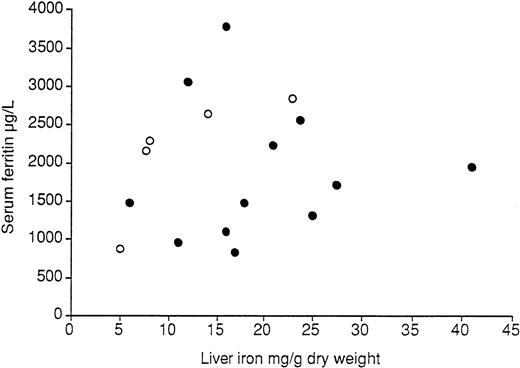
The serum ferritin and liver iron concentrations (measured during the same admission) in 17 TM patients who underwent liver biopsy after 2 to 4 years of deferiprone therapy. (○), Chronic liver disease caused by hepatitis C. Liver iron: 1 mg/g = normal; >22 mg/ g = cirrhosis develops with time.
The serum ferritin and liver iron concentrations (measured during the same admission) in 17 TM patients who underwent liver biopsy after 2 to 4 years of deferiprone therapy. (○), Chronic liver disease caused by hepatitis C. Liver iron: 1 mg/g = normal; >22 mg/ g = cirrhosis develops with time.
The initial and final serum ferritin concentrations in 25 patients who discontinued deferiprone therapy. (▵), Agranulocytosis; (---○), renal failure; (—•), increasing ferritin; (▪†), death; (┌), nausea; (—○), neutropenia; (□), tachycardia; (––•), anthropathy; (▴), went abroad; threshold of effective treatment: (▧), USA; (▨), WHO.
The initial and final serum ferritin concentrations in 25 patients who discontinued deferiprone therapy. (▵), Agranulocytosis; (---○), renal failure; (—•), increasing ferritin; (▪†), death; (┌), nausea; (—○), neutropenia; (□), tachycardia; (––•), anthropathy; (▴), went abroad; threshold of effective treatment: (▧), USA; (▨), WHO.
Figure 3 shows the chemical liver iron content and serum ferritin levels taken at the time of biopsy in 17 iron-overloaded TM patients. The mean liver iron content was 17.4 mg/g dry weight (range, 5.9 to 41.2). Two patients had a liver iron content below 7.0 mg/g dry weight, which has been considered the threshold where life expectancy is not affected. Five patients had liver iron content between 7.9 and 14.1 mg/g dry weight and the remaining 10 patients had a liver iron content above 15.0 mg/g dry weight, ie, falling within the range that has been associated with cardiac disease. Overall, the serum ferritin and chemical liver iron values did not correlate. Five of 17 patients had chronic liver disease caused by hepatitis C virus (HCV). There was no correlation between serum ferritin and liver iron in the 12 patients without cirrhosis or hepatitis C infection. Five of the patients were hepatitis C-RNA positive and these all showed cirrhosis of the liver. Among the 12 patients who were anti-HCV and hepatitis C-RNA negative, the liver biopsy samples showed that none had cirrhosis and they showed either no fibrosis (11 patients) or mild fibrosis (1 patient). This patient began with the highest initial serum ferritin level, 9,087 μg/L.
Urine iron excretion in response to deferiprone among the 26 patients initially ranged from 16.3 to 58.2 mg/24 h (mean, 31.2). There was no significant overall change in urine iron excretion among the 26 patients who had received treatment for a mean of 39.4 months. The mean urine iron excretion at the end of the study was 32.1 mg/24 h (range, 9.4 to 75.8). There was also no overall change in urine iron excretion in the 15 patients who had received deferiprone for more than 36 months (Table 3).
Regular blood counts were performed in all patients during the study period. No changes in renal function, white blood cell, or platelet counts were observed in the 26 patients. No changes were seen in aspartate aminotransferase and alanine aminotransferase levels except for the six patients with chronic hepatitis C, where fluctuating liver enzyme levels were observed. During treatment with deferiprone, marginally low serum zinc levels developed in eight patients. All eight had biochemical evidence of diabetes or insulin dependent diabetes. These patients were given oral zinc supplements (220 mg/d). MUGA scan results showed no significant change at rest and on stress between initial and final values in the 26 patients.
DISCUSSION
The results of this study show that long-term (more than 4 years) iron chelation therapy is feasible using the orally active drug deferiprone. They also confirm the findings of previous studies in which different side effects of deferiprone therapy have been reported.9-11
Our earliest short-term clinical trials showed that 24-hour urine iron excretion equivalent to that induced by subcutaneous DFX (40 to 50 mg/kg administered over 8 to 10 hours) could be achieved with 100 mg/kg deferiprone given in two to four doses each day.12,13 No change in overall mean serum ferritin levels was achieved in up to 1 year of treatment.14 A number of subsequent abstracts showed decreases in serum ferritin levels, particularly in patients starting with high serum ferritin levels.10,11,15,16 One study, published only in abstract form, reported that deferiprone (75 mg/kg/d) was more effective in treating TM over 1- to 2-year periods than was subcutaneous DFX.17 A subsequent abstract by the same investigators showed that hepatic iron concentration was in an optimal range after 2 years of therapy in 64% of patients receiving DFX, but in only 7% of patients receiving deferiprone.18This same group reported decreases in liver iron in 10 previously poorly chelated patients with initial liver iron levels above 80 μmol/g wet weight treated with deferiprone for 1 to 3 years. There was a decrease from a mean of 125.3 ± 11.5 to 60.3 ± 9.6 μmol, 8 of the 10 patients achieving a level less than 80 μmol/g.19 In a further 11 patients, previously better chelated, liver iron content remained below 80 μmol/g. These workers also reported among the 21 patients a significant decrease in mean serum ferritin concentration from 3,975 to 2,546 μg/L. Because of these encouraging results and because of our previous experience of important side effects with deferiprone at a dose of 100 mg/kg/d, we chose for the present long-term study deferiprone doses of 75 mg/kg/d, in the hope of experiencing fewer side effects without significant loss of efficacy.
The serum ferritin concentration is a relatively inaccurate measure of body iron burden compared with liver iron estimation. Nevertheless, the results here show that for the 15 patients who have taken the drug constantly for over 3 years, there has been no significant change in serum ferritin concentration or in urine iron excretion in response to deferiprone, implying no significant overall change in iron stores. Deferiprone, therefore, has been effective in these patients at balancing iron input from blood transfusions by iron excretion in the urine. This is consistent with a mean urinary excretion of about 25 mg/24 h in these patients, representing 0.5 mg/kg/24 h for a 50-kg individual. Whether additional iron excretion occurs through the stools in response to deferiprone is uncertain.
The results of our liver iron estimations were disappointing. Among the 17 patients tested, after a mean of 40 months therapy (range, 27 to 49 months) only 2 showed liver iron levels below 7 mg/g, a level considered safe,20 while 8 had levels above 15 mg/g, levels at which liver and cardiac damage are likely to occur.21 In a group of 12 patients who had received subcutaneous DFX for 4 to 8 years, we found 50% had liver iron levels less than 7 mg/g.1 Moreover, in contrast to Olivieri et al,19 we found no significant correlation between serum ferritin and liver iron. Nine of the 15 patients who have received deferiprone for more than 3 years show serum ferritin levels over 2,500 μg/L, a level taken by some to indicate inadequate chelation therapy.22 The discrepancies between our results and that reported by Olivieri et al19 may be more apparent than real. In both studies, the majority of patients starting therapy with serum ferritin levels greater than 2,500 μg/L still showed levels in this range after several years of therapy. Also, the majority of previously poorly chelated patients in both studies showed hepatic iron levels greater than 15 mg/g dry weight after more than 2 years of deferiprone therapy.
Our study included a substantial number of nonthalassemic patients, but overall there were no significant differences either in efficacy or incidence of side effects among the 40 patients with thalassemia syndromes or the 11 patients with other diseases. Our liver biopsy samples showed no evidence of direct toxicity of the drug to hepatic cells. Fibrosis was mild in only 1 of 12 patients without hepatitis C infection. Among the hepatitis C positive patients, the appearances were consistent with changes known to be associated with the virus infection.
The wide variation in iron excretion among the patients may relate partly to a wide range in body iron stores, with iron excretion being greater in those with greater body iron burden.12,13 Iron excretion also relates to the area under the curve of free deferiprone in plasma after a single oral dose.23 The drug is glucuronidated at a different rate in different patients. Efficacy will be affected since glucuronidation inactivates the drug's iron binding site. The lack of efficacy in some patients despite high iron body loads, as in four patients with rising serum ferritin levels during treatment, may be the result of particularly fast glucuronidation of deferiprone.
Nearly 50% of the patients commencing deferiprone discontinued the drug. Overall, these patients initially showed significantly higher iron stores, assessed by serum ferritin, than the patients who were able to continue the drug. Five patients died, but in none could this be attributed a toxic effect of the drug. In four previously, poorly chelated patients, death was due to cardiac disease induced by iron overload. However, these findings imply that deferiprone is inappropriate therapy for patients with iron-induced cardiomyopathy in whom continuous intravenous DFX is needed to cause continuous removal of toxic, nontransferrin-bound iron from plasma. Moreover, substantially more iron excretion can be achieved with continuous DFX administered intravenously than with either intermittent subcutaneous infusion of DFX or with oral doses of deferiprone.
Joint symptoms in association with deferiprone therapy were first reported by Bartlett et al.24 They occurred in up to 33% of patients in the Indian trial,11 a study showing that high doses of deferiprone and greater degrees of iron overload of the patient were both predisposing factors. No relation with changes in ANF or rheumatoid factor titres have been shown in this or any other study, and the mechanism of the damage, whether free radical generation or immunological, remains to be determined.
Agranulocytosis is the most serious complication so far reported with deferiprone therapy. The incidence of this and of lesser degrees of neutropenia as occurred in two patients here (and previously reported9) is not yet determined. It may depend partly on the dose of deferiprone, the iron load of the patient, the patient's ethnic group, and the nature of the underlying disease. Among 13 patients reviewed by Hoffbrand,6 nine were female, suggesting a possible increased susceptibility in females as occurs with other idiosyncratic drug agranulocytosis. Patients with TM, myelodysplasia, and Blackfan-Diamond anemia have all suffered agranulocytosis but all have recovered. Despite experiments designed to elucidate a toxic or immune mediated mechanism, no evidence for either has been established.25 26 The licensing of deferiprone in India and its subsequent widespread use in therapy of thalassemia is likely to result in new cases of agranulocytosis or neutropenia and it is hoped that any such cases will be fully documented and reported. A recently completed multicenter Italian trial will give additional information on the incidence of neutropenia.
Five patients withdrew from the present study because of gastrointestinal symptoms on taking the drug. Two of the patients showed renal impairment at the start of therapy and in one of these, which involved a man of 82 years, pharmacokinetic studies have shown prolonged accumulation of deferiprone-glucuronide in plasma after a single oral dose. A significant correlation between creatinine clearance and area under the curve for the glucuronide derivative in plasma after a single oral dose has been shown.23 It may be that nausea in these two patients was caused by accumulation of the glucuronide in plasma. At all events this side effect, not previously highlighted, resulted in 10% of our patients reverting back to subcutaneous DFX for chelation therapy.
How can we improve on these results? The efficacy of deferiprone is dose related and it might be that increasing the dose from 75 to 100 mg/kg/d in those that can tolerate it may be more effective in some patients. In preliminary studies we have increased the dose of deferiprone to 85 mg/kg in 10 of the 26 patients still taking the drug, with no new side effects and with increased iron excretion. Another possibility is to administer intravenous DFX therapy at the time of blood transfusion and deferiprone between transfusions or to use the newly introduced DFX continuous infusers27 for a day or two each week with chelation with deferiprone on the same and other days, possibly increasing overall iron excretion but reducing side effects of both drugs in this way.
Address reprint requests to A. Victor Hoffbrand, FRCP, Department of Haematology, Royal Free Hospital, Pond St, London, NW3 2QG UK.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.