Abstract
The inhibition of cyclooxygenase does not fully account for the spectrum of activities of nonsteroidal antiinflammatory drugs. It is evident, indeed, that regulation of inflammatory cell function may contribute in explaining some of the effects of these drugs. Tissue recruitment of T cells plays a key role in the development of chronic inflammation. Therefore, the effects of salicylates on T-cell adhesion to and migration through endothelial cell monolayers on collagen were analyzed in an in vitro static system. Aspirin and sodium salicylate reduced the ability of unstimulated T cells to adhere to and transmigrate through cytokine-activated endothelium. Although salicylates did not modify the expression of integrins on T cells, they blunted the increased adherence induced by the anti-β2monoclonal antibody (MoAb) KIM127 and prevented the appearance of an activation-dependent epitope of the CD11/CD18 complex, recognized by the MoAb 24, induced by contact with endothelial cells. Salicylates also induced an increase of intracellular calcium ([Ca2+]i) and activation of protein kinase C (PKC) in T cells, but not cell proliferation and interleukin (IL)-2 synthesis. The reduction of T-cell adhesiveness appears to be dependent on the increase in[Ca2+]i levels, as it could be reversed by blocking Ca2+ influx, but not by inhibiting PKC. Moreover, ionomycin at concentrations giving an increase in [Ca2+]i similar to that triggered by aspirin, strictly reproduced the T-cell phenotypic and functional changes induced by salicylates. Aspirin reduced T-cell adhesion and migration also ex vivo after infusion to healthy volunteers. These data suggest that the antiinflammatory activity of salicylates may be due, at least in part, to an interference with the integrin-mediated binding of resting T lymphocytes to activated endothelium with consequent reduction of a specific T-cell recruitment into inflammatory sites.
NONSTEROIDAL ANTIINFLAMMATORY drugs (NSAIDs) are very effective in the treatment of inflammatory disorders, although patient compliance is often compromised by NSAID-induced gastric mucosal injury.1 It is thought that the pharmacologic effect of these drugs is mainly due to the inhibition of prostaglandin (PG) synthesis.2 However, the precise mechanism of action of NSAIDs has not been completely clarified, as the inhibition of PG synthesis does not account for the entire spectrum of NSAID antiinflammatory activities.3 Doses of acetylsalicylic acid (aspirin, ASA) necessary to treat chronic inflammatory diseases, indeed, are much higher than those required to inhibit PG synthesis.3 Moreover, there is an increasing body of evidence to suggest that NSAIDs derive significant antiinflammatory effects from non–PG-dependent mechanisms, including perturbation of the cell membrane lipid bilayer, modification of cytokine production, and inhibition of a number of intracellular events including transmembrane anion transport, oxidative phosphorylation in mitochondria, and activation of transcription factor nuclear factor-kB.2-6 None of these, however, fully explains the antiinflammatory action, as well as the side effects, of these drugs.
In recent years, there have been several lines of evidence to support the hypothesis that polymorphonuclear cells (PMN) play a key role in the pathogenesis of NSAID-induced gastric mucosal injury and that PMN adherence to vascular endothelium, mediated by an interaction between integrins and their ligands expressed on activated endothelial cells, is one of the early and pivotal events in the process leading to NSAID-induced gastric damage.7-14
The enhanced leukocyte adherence to endothelial cells induced by NSAIDs, however, appears to represent a paradoxical effect in view of the antiinflammatory action of these drugs. Indeed, leukocyte adhesion to and migration through endothelium represent the initial and fundamental steps in mounting an inflammatory response.15-20 Several adhesion molecules, which bind specific counterreceptors on endothelial cells, are involved in these processes. Among them, integrins, in particular the β2-integrins and the β1-integrin very late antigen (VLA)-4, mediates the firm leukocyte attachment to endothelium, a prerequisite for transendothelial migration and cell extravasation to the inflamed tissues.18-20
These mechanisms regulate adhesion and migration also of T lymphocytes, which play a fundamental role in the development of chronic inflammation, such as synovitis in rheumatoid arthritis.16,21-24 However, data regarding the effects of NSAIDs on T-cell functions and, in particular, on T-cell/endothelium interaction are scanty and controversial.25-29 In the present study, we showed that ASA and sodium salicylate (NaS) can reduce the ability of T lymphocytes to adhere to endothelial cell monolayers and to transmigrate into collagen in an in vitro static model. This inhibitory effect appears to be mediated, at least in part, by a Ca2+-dependent interference with the activation of β-integrins, which mediate T-cell adhesion.
MATERIALS AND METHODS
Cell purification.
Peripheral blood mononuclear cells (PBMC), monocytes, and T cells were isolated as already reported,30 and resuspended in RPMI-1640 supplemented with 10% fetal calf serum (FCS), 4 mmol/L L-glutamine, 100 U/mL penicillin, and 100 μg/mL streptomycin (complete medium) (GIBCO-BRL, Gaithersburg, MD). Platelets and monocyte contamination in each purified T-cell suspension, as assessed by microscope examination and nonspecific esterase staining, was less than 1%.
Monoclonal antibodies (MoAbs) and reagents.
Anti-CD3 was purified from supernatant of hybridoma cells obtained from the American Type Cell Culture Collection (Rockville, MD). The anti–L-selectin MoAb DREG-200 was kindly supplied by Dr Dorian O. Haskard (Rheumatology Unit, Hammersmith Hospital, London, UK). Anti-CD29 (4B4) was purchased from Coulter Immunology (Hialeah, FL), anti-CD11a (IOT16) and anti-CD18 (IOT18) from Immunotech (Marseille, France), anti-CD11b (OKM1) from Ortho Diagnostic Systems Inc (Raritan, NJ), anti-CD11c (Leu-M5) from Becton Dickinson (San Jose, CA), and anti-CD49d from Dakopatts (Copenhagen, Denmark). The KIM127 MoAb, stimulating CD18-dependent cell adhesion,31 was kindly provided by Dr Martyn Robinson (Celltech Therapeutics Ltd, Berkshire, UK). The anti-β1 integrin MoAb TS 2/16 was kindly donated by Dr Francisco Sanchez-Madrid (Hospital da la Princesa, Madrid, Spain).32 The MoAb 24, recognizing an activation-dependent epitope of all subunits of CD11a/CD18 complex,33 was a kind gift of Dr Nancy Hogg (Imperial Cancer Research Fund, London, UK). Human recombinant (r) tumor necrosis factor-α (TNF-α) (specific activity, 6.8 × 107 U/mg) was graciuosly provided by Dr E. Allievi (Knoll Farmaceutici S.p.A., Milan, Italy). Human r interleukin-1β (IL-1β) (specific activity, 1.3 × 107 U/mg), phorbol myristate acetate (PMA), and ionomycin were purchased from Sigma Chemical Co (St Louis, MO). The kinase inhibitors staurosporin, H-7 and calphostin C, were obtained from Biomol (Plymouth Meeting, PA). Type I collagen solution extracts from porcine skin (Cellmatrix I-A) were purchased from Nitta Gelatin, Inc (Osaka, Japan). Endothelial cell growth factor was purified from bovine hypothalamus extract, as described.34 ASA and NaS were purchased from Sigma. Because it is thought that a total serum salicylate concentration of 250 to 350 μg/mL is associated with optimal antiinflammatory effects,35 a final concentration of 300 μg/mL for both drugs was chosen for the experiments. In some of these, 30 and 600 μg/mL final concentrations were also used to evaluate the dose-dependency of the observed results.
Cell phenotype.
T-cell surface phenotyping was performed with a two-color immunofluorescence staining technique using isotype-specific goat antimouse antibodies (Southern Biotechnology Associates, Birmingham, AL) conjugated with either fluorescein or phycoerythrin as developing reagents for each MoAb. This procedure has been described in detail elsewhere.30 For the evaluation of salicylates' activity on the expression of adhesion molecules on the T-cell surface, parallel experiments using PBMC simultaneously stained with anti-CD3 and the specific antiadhesion molecule MoAb were performed to rule out nonwanted effects on membrane molecules induced by T-cell purification procedures. Because no phenotypic differences between T-cell and PBMC suspensions were found, only the results obtained with purified T-cell samples were given. Negative controls and tests to prove the specificity of the isotype-specific antisera were performed for each experiment as described.30
Culture of human umbilical vein endothelial cells (HUVEC).
Endothelial cells were harvested from HUVEC treated with 0.1% collagenase (Type I; Boehringer Mannheim, Mannheim, Germany), by a previously described method.36 Cells were grown on 5% gelatin-coated 25-cm2 culture flask (Falcon; Becton Dickinson) in M-199 (Sigma) supplemented with 20% FCS, antibiotics, 90 μg/mL porcine intestinal heparin (Sigma), and 100 μg/mL endothelial cell growth factor. Cells were passaged using trypsin-EDTA (GIBCO). Identification of cultured endothelial cells was confirmed by their cobblestone structure and by immunohistochemistry, using a rabbit antihuman von-Willebrand factor antibody (Dakopatts) and fluorescein isothiocyanate (FITC)-conjugated goat antirabbit IgG antibody. Nearly 100% of the cells showed a positive staining. These experiments used cells in passages 2 to 3 only. To prepare the collagen-coated wells, the concentration of collagen in the aqueous stock solution (3 mg/mL) was adjusted to 1 mg/mL with pH 3.0 HCl/distilled water. Collagen gels were prepared in a 15-mL polystyrene tube (Falcon) by rapidly mixing 8 vol of the diluted collagen solution, 1 vol of 10× M199, and 1 vol of 0.2 mol/L HEPES plus 0.08 N NaOH/distilled water. A total of 100 μL of the solution was seeded into each well of a 24-well plate (Falcon) and incubated at 37°C until the solution became gel. A total of 500 μL of HUVEC suspensions containing 2 × 105 cells were added to the collagen-coated 24-well plate. Culture media was changed every 3 days.
T-cell adhesion to and migration through HUVEC monolayers cultured on collagen gels in an in vitro static experimental system.
HUVEC monolayers were precultured for at least 3 days on collagen gels in the plastic 24-well plates before treatment with rTNF-α (10 ng/mL) or rIL-1β (10 IU/mL), as already described.37 After washing, the HUVEC monolayers were incubated with T-cell suspensions (2.0 × 106/well) at 37°C. At the selected times, unbound T cells were removed from the surface of the HUVEC monolayers by gently washing with warmed M-199 + 0.1% bovine serum albumin (BSA). The HUVEC were then incubated for 20 minutes at 37°C with 0.4% EDTA in phosphate-buffered saline (PBS) to remove adherent T cells. Almost all adherent T cells could be detached from the surface of HUVEC with this treatment. Monolayers were then treated for another 30 minutes with 0.4% EDTA to remove HUVEC from the surface of collagen gels, this process being monitored with phase microscopy to confirm removal of HUVEC. After monolayers were washed out with PBS, the collagen gels containing migrating T cells were treated with 0.05% collagenase/Hanks' balanced salt solution (HBSS) at 37°C for 3 minutes two to three times with continuous pipetting to release the T cells. After each pipetting with collagenase, FCS (10% at final concentration) was added to the solution containing cells to diminish the enzyme activity. The number of adherent and migrating T cells was counted by hemocytometer and analyzed by flow cytometry. No changes in the expression of CD3 and other adhesion molecules were found on T cells after collagenase treatment.
Cell proliferation assay.
In vitro T-cell proliferation (5 × 104/well) was performed in triplicate in complete medium in 96-well round-bottomed microwell plates (Nunc, Roskilde, Denmark), as described.30For positive controls, anti-CD3 was placed in a 96-well flat bottom microtiter plate (No. 3596; Costar, Data Packaging Corp, Cambridge, MA) and incubated at room temperature for 1 hour. The wells were then washed twice in medium to remove nonadherent MoAb before T cells were added. A total of 20 IU/mL of human rIL-2 (Janssen, Beerse, Belgium; specific activity, 9.0 × 106 U/mg) was added to plastic immobilized anti-CD3 MoAb to obtain full proliferation in highly purified T-cell cultures. This was measured by (3H)-TdR incorporation (0.5 Ci, specific activity, 25 Ci/mmol; Amersham Int, Amersham, UK) during the last 6 hours of culture and counting in a liquid scintillation counter. In some experiments, a minimal amount of autologous monocytes (1% to 2% in the final cell suspension), instead of rIL-2, was added to purified T-cell cultures.
Assay for IL-2 secretion.
A commercially available radioimmunoassay (RIA) kit was used to detect IL-2 levels in filtered cell culture supernatants after 48-hour cultures (Medgenix Diagnostics SA, Fleurus, Belgium), according to manufacturer's instructions.
Intracellular [Ca2+]i measurement.
Concentration of [Ca2+]i was measured in T-cell suspensions using fura-2/AM (Sigma), a Ca2+fluorescent ester chelator and indicator.38 T cells (1 × 106/mL) were suspended in standard incubation solution, 5 mmol/L fura-2/AM was added, and incubated at 37°C for 30 minutes. Cells were washed twice in iced buffer solution, resuspended in either standard medium or in a Ca2+-free medium containing 1 mmol/L EGTA (Sigma) and transferred in a quartz cuvette under continuous stirring with the temperature thermostatically maintained at 37°C. Fluorescence was measured by a Hitachi 2000 spectrophotometer (Pabisch, Milan, Italy) by adjusting the excitation wavelengths sequentially at 340- and 380-nm and the emission wavelengths at 510 nm. Levels of [Ca2+]i were calculated according to Tsien et al.39 The fura-2/AM-Ca2+ signal was calibrated at the end of each experiment by adding 125 μmol/L digitonin followed by 2.5 mmol/L EGTA in Tris base, pH 8.3. The [Ca2+]i levels were measured in resting T cells (basal) or in T cells stimulated with different concentrations of ionomycin, ASA, or NaS. To ascertain whether salicylates increased Ca2+ influx, manganese (Mn2+) was used as a Ca2+surrogate.40 Fura-2–loaded cells were resuspended in a Ca2+-free buffer and stimulated with ASA or NaS. Fluorescence was excited at 360 nm, ie, the isosbestic wavelenght at which Ca2+ does not affect fura-2 fluorescence and changes in fluorescence intensity are only caused by Mn2+quenching. Emission was recorded at 505 nm. Maximal Mn2+quenching was calibrated in each preparation at the end of recording with digitonin.
Evaluation of protein kinase C (PKC) activity.
PKC activity was evaluated by a previously described method using the binding of [20(n)-3H]-phorbol-12,13-dibutirrate ([3H]PdBu) (Amersham Int; specific activity, 16.2 Ci/mmol) to intact cells and based on the principle that some of the phorbol esters can interact with the site for diacylglycerol on PKC.41 T cells (2 × 106/mL) were washed with Locke's solution and incubated for 30 minutes with the same solution containing 10 nmol/L of [3H]PdBu. PKC activity was evaluated using adequate negative and positive controls represented respectively by the nonactivated enzyme and by the enzyme maximally activated with 100 μmol/L of norepinephrine. Nonspecific binding was determined in the presence of 1 μmol/L unlabeled PMA. After incubation, T cells were washed with cold Locke's solution, dried, and resuspended in 0.5% Triton. Aliquots of each suspension were used for liquid scintillation counting. Staurosporin (1 nmol/L), H-7 (100 μmol/L), or calphostin C (1 μmol/L) were used in the assay as PKC inhibitors, when indicated.
In vivo experimental infusion of aspirin.
After giving informed consent, three healthy volunteers had a sample of venous blood taken. Then, 500 mg of aspirin (lysine acetylsalicylate, Aspegic; Synthelabo, Milan, Italy) was injected intravenously over 1 to 2 minutes and other blood samples were taken 30 and 120 minutes after the injection to analyze T-cell adhesion and migration ability, as described above.
Statistical analysis.
Owing to the nonnormal distribution of samples, the Kruskal-Wallis analysis of the variance was adopted for the statistical evaluation of the results. Values of P < .05 were chosen for rejection of the null hypothesis.
RESULTS
Effect of salicylates on T-cell capacity to adhere to HUVEC and migrate into collagen.
Unstimulated T lymphocytes, when exposed for 30 minutes to unstimulated HUVEC monolayers, had a low adhesive (mean ± standard error of mean [SEM], 10% ± 5%) and migratory ability (0.2% ± 0.2%). HUVEC activation by rTNF-α led to a significant increase in adhesiveness and migration of T cells, which was detectable 1 hour after triggering (16% ± 3% and 1.3% ± 0.7%; P < .01) and which was maximal 4 hours after addition of the cytokine (26% ± 8% and 4.7% ± 3%; P < .001). Similar results were obtained when rIL-1 was used as HUVEC activating stimulus (data not shown). The binding was mainly mediated by both β2- and β1-integrins, as T-cell/HUVEC interaction was markedly reduced by saturating concentrations of anti-CD18 (−73.9%) or anti-CD29 MoAbs (−60.7%). An almost complete inhibition of T-cell adhesion to endothelium was obtained when anti-CD18 and anti-CD29 were used together in the in vitro assay (−93.8%). L-selectin instead had a minor role in the attachment of T cells to HUVEC in this experimental condition, as the anti–L-selectin MoAb DREG-200 only marginally inhibited T-cell binding to HUVEC (−12.6%).
Experiments were then designed to determine the effects of ASA or NaS on adhesion and migration of resting T cells. As our preliminary data showed that negligible numbers of T cells adhered to and migrated through unstimulated HUVEC, we used only activated HUVEC. Preincubation of resting T lymphocytes with either ASA or NaS for 30 minutes resulted in a dose-dependent decrease in adherence to HUVEC monolayers with an inhibitory effect plateauing at 300 μg/mL (Table 1). A more prolonged incubation with ASA or NaS (1 to 2.5 hours) had similar inhibitory effects, while a shorter incubation (15 minutes) led to a lesser inhibition of T-cell adherence to HUVEC (data not shown). ASA or NaS treatment produced also a dose-dependent reduction of T-cell migratory capacity (Table 1). No effects were obtained by pretreatment of HUVEC with various concentrations of the two drugs for different incubation times (data not shown).
Effect of salicylates on T-cell integrin expression.
In an attempt to investigate the molecular basis of the inhibitory activity of ASA and NaS, we analyzed the expression of integrins, which play a key role in endothelial/T-cell interaction in an in vitro static system,42 43 on unstimulated T cells. Flow cytometry analysis showed that the basal expression of CD11b (mean fluorescence intensity [MFI], 91 ± 18) was slightly, but significantly, increased after treatment for 30 minutes with 300 μg/mL or 600 μg/mL of ASA (+12.8% ± 4% and +13.8% ± 3%, respectively;P < .05) or NaS (+10.1% ± 4% and +12.5% ± 4%; P < .05), whereas CD18, CD11a, CD11c, CD29, and CD49d molecule expression was unchanged (data not shown).
Effect of salicylates on integrin activation.
Our phenotypic data do not explain the negative interference by ASA or NaS on the firm T-cell/endothelium adhesion obtained in our in vitro model. The lack of quantitative changes in surface expression of integrins, however, does not rule out a possible interference by salicylates with qualitative changes of the molecules, as it is known that the conformational state of integrins plays a critical role in the adhesion of T cells to endothelium.15,16 Thus, to verify the effect of salicylates on integrin function, we used the anti-β2 MoAb KIM127 and the anti-β1 TS2/16, able to directly induce the active conformation of the respective molecules.31 32 A strong enhancement of T-cell adhesion and migration was induced by the anti-β2, while a minor, but significant, increase in adhesion was obtained with the anti-β1 MoAb (Table 2). Pretreatment with ASA (Table 2) or NaS (data not shown) of T cells prevented the enhancement in adhesion triggered by these stimulating MoAbs. It is worth noting that salicylates were also able to significantly reduce T-cell migration induced by the KIM127 MoAb, thereby suggesting an effect of the drug on β2-mediated binding.
On the basis of these results, as well as previous observation showing an induction of integrin activation on the surface of PMN by simple contact with activated endothelium and/or platelets,44 we wondered whether the attachment of resting T lymphocytes to activated endothelial cells is able to activate integrins and whether salicylates can block this activation. To test this hypothesis, we analyzed the expression of an activation-dependent epitope of the CD11/CD18 complex, recognized by the MoAb 24,33,45 46 on the surface of T cells before and after adhesion to and transmigration through HUVEC. The results reported in Table 3 show that the 24 epitope was undetectable on unstimulated T cells, but it significantly increased on T cells adherent to activated HUVEC. Interestingly, maximal antigen expression was displayed by the migrated T-cell fraction. Neither ASA nor NaS induced the 24 epitope on the surface of unstimulated T cells. However, T-cell preincubation with 300 μg/mL ASA for 30 minutes strongly reduced the expression of 24 epitope triggered by the contact with HUVEC on both adherent and migrated cell fractions (Table 3). NaS preincubation gave similar results (data not shown). Thus, taken together, our data suggest that salicylates are able to decrease the adhesion of resting T cells to cytokine-activated HUVEC by preventing T-cell integrin activation induced by contact with endothelium.
Effect of salicylates on [Ca2+]ilevels and PKC activation.
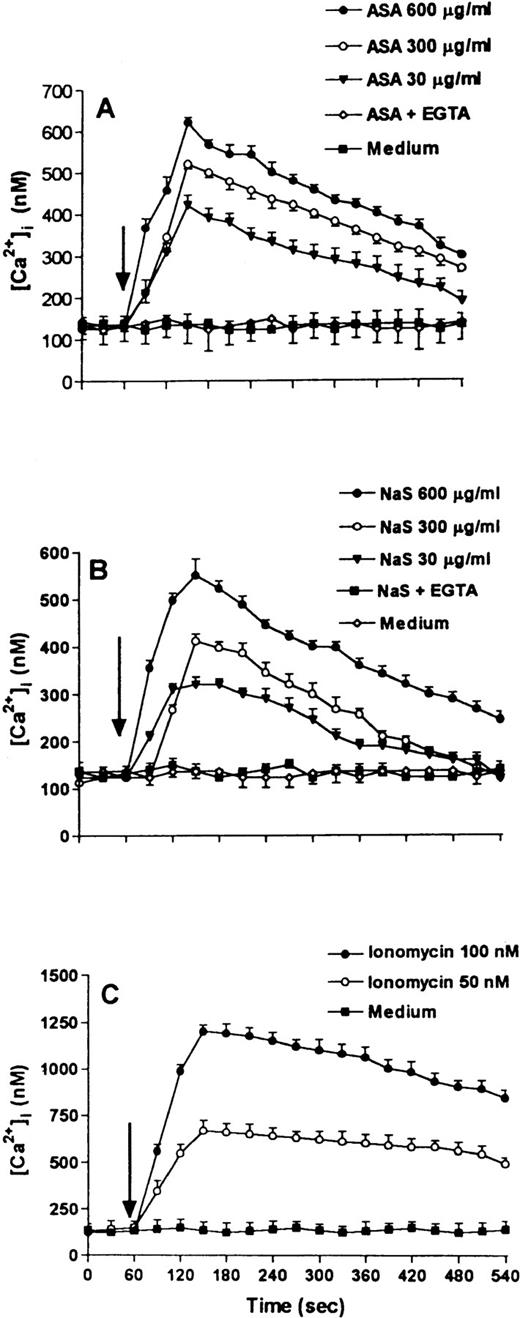
Several studies have shown that changes in the integrin conformational state on T cells are modulated by intracellular signals triggered by activating stimuli.47,48 Therefore, we were interested in evaluating whether salicylates are able to elicit intracellular events, which usually follow T-cell activation.49 As shown in Fig 1A and B, both ASA and NaS were able to induce a dose-dependent increase of [Ca2+]i, which reached a maximal increase of fivefold to sixfold over basal with 600 μg/mL ASA or NaS.
Time-course of Ca2+-mobilization induced by ASA (A), NaS (B), or ionomycin (C) in T cells loaded with Fura 2/AM. Cells were incubated in complete medium and stimulated after 60 seconds (arrow) with different concentrations of salicylates or ionomycin. Results of experiments in which T cells were incubated in Ca2+-free medium in the presence of 1 mmol/L EGTA are also shown (A and B). Data are expressed as the mean SEM of 20 determinations.
Time-course of Ca2+-mobilization induced by ASA (A), NaS (B), or ionomycin (C) in T cells loaded with Fura 2/AM. Cells were incubated in complete medium and stimulated after 60 seconds (arrow) with different concentrations of salicylates or ionomycin. Results of experiments in which T cells were incubated in Ca2+-free medium in the presence of 1 mmol/L EGTA are also shown (A and B). Data are expressed as the mean SEM of 20 determinations.
Ionomycin induced a concentration-dependent increase of [Ca2+]i level, the effect being detectable at 1 nmol/L and maximal at 100 nmol/L (data not shown). Fig 1C shows that the magnitude of [Ca2+]i increase obtained with optimal ASA or NaS concentrations was reproduced by the effect of suboptimal concentration of ionomycin (50 nmol/L).
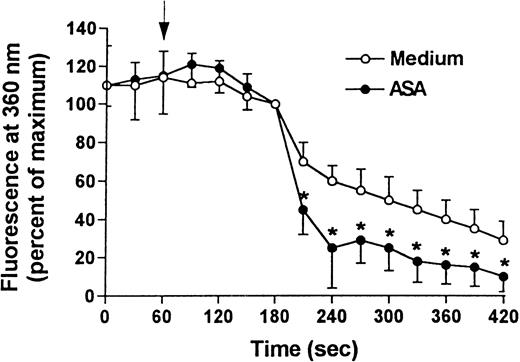
Salicylate-induced [Ca2+]i mobilization was largely dependent on a Ca2+ inflow, as demonstrated by the rapid quenching of fura-2 signals induced by adding Mn2+ to the extracellular medium (Fig 2) and by the fact that the [Ca2+]i increase was completely abolished by preincubating the cells with 1 mmol/L of EGTA (Fig 1A and B).
Effect of Mn2+ addition to Fura 2/AM-loaded T cells incubated with ASA. Mn2+ was used as substitute for Ca2+ and the more pronounced the quenching of the Fura 2/AM signal, the higher the Mn2+ influx. Cells were incubated in a Ca2+-free medium and stimulated (arrow) with ASA or no agent (medium). After incubation for 60 seconds, 25 μmol/L Mn2+ was added to the cell suspension. Fluorescence intensity was normalized to 100% just before Mn2+addition. Data are expressed as the mean SEM of 10 determinations. (*)P < .01
Effect of Mn2+ addition to Fura 2/AM-loaded T cells incubated with ASA. Mn2+ was used as substitute for Ca2+ and the more pronounced the quenching of the Fura 2/AM signal, the higher the Mn2+ influx. Cells were incubated in a Ca2+-free medium and stimulated (arrow) with ASA or no agent (medium). After incubation for 60 seconds, 25 μmol/L Mn2+ was added to the cell suspension. Fluorescence intensity was normalized to 100% just before Mn2+addition. Data are expressed as the mean SEM of 10 determinations. (*)P < .01
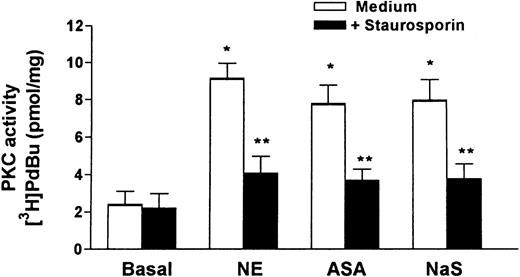
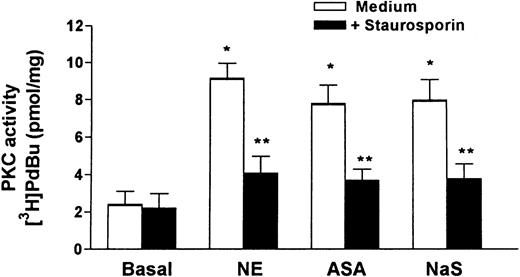
As Fig 3 shows, the incubation of T cells with 300 μg/mL of ASA or NaS led to a significant activation of PKC, close to the maximum obtained with norepinephrine, which was abolished by the PKC inhibitor staurosporin. Two other PKC inhibitors, H7 and calphostin C, were also able to inhibit the PKC stimulation produced by ASA and NaS to a similar extent (data not shown). Significant PKC activation was also obtained with 30 or 600 μg/mL of both drugs (data not shown).
Effect of ASA and NaS on PKC activity in T lymphocytes. Positive controls were represented by maximal PKC activation obtained with 100 μmol/L norepinephrine (NE). Data are expressed as the mean SEM of four separate experiments. P < .001 versus basal values (*) or versus the respective values obtained with medium alone (**).
Effect of ASA and NaS on PKC activity in T lymphocytes. Positive controls were represented by maximal PKC activation obtained with 100 μmol/L norepinephrine (NE). Data are expressed as the mean SEM of four separate experiments. P < .001 versus basal values (*) or versus the respective values obtained with medium alone (**).
Effect of EGTA and PKC inhibitors on adhesive and migratory ability of salicylate-treated T cells.
To check whether [Ca2+]i increase and/or PKC activation were relevant for the observed inhibition by salicylates of T-cell adhesion and migration, experiments using the Ca2+ chelator EGTA, as well as different PKC inhibitors, were performed (Table 4). The ASA-induced decrease of T-cell adhesiveness and migration was almost completely reversed by the addition of EGTA, whereas staurosporin, calphostin C, or H7 did not significantly affect the functional T-cell changes induced by ASA. Overlapping results were obtained in similar experiments using NaS instead of ASA (data not shown).
Modulatory effect of [Ca2+]i increases on β2-integrin induced T-cell function.
Having shown a role of [Ca2+]i rather than PKC in the observed effect of salicylates on T-lymphocyte adhesion and migration, we first verified whether specific stimulation of β2-integrin is able to increase the [Ca2+]ilevels of resting T lymphocytes and subsequently analyzed the possible influence of salicylates on this intracellular event. The data shown in Fig 4 indicate that the binding of KIM127 MoAb to β2-integrin triggers a significant enhancement of [Ca2+]i levels and that preincubation of T cells with ASA for 30 minutes blunts this increase. Moreover, it is of interest to note that a similar inhibitory effect on the KIM127-induced [Ca2+]i increase was observed when T cells were preincubated for 30 minutes with the suboptimal concentration of ionomycin able to mimic the [Ca2+]i increase induced by ASA (Fig 4).
Effect of ASA or ionomycin pretreatment of T cells on [Ca2+]i mobilization induced by the anti–β2-integrin MoAb KIM127. Cells were incubated with 300 μg ASA, 50 nmol/L ionomycin, or medium for 30 minutes at 37°C, washed, and then tested for mobilization of [Ca2+]i. Arrow indicates addition of KIM127 MoAb (medium [•], ASA [◊], and ionomycin pretreatment [□]) or its solvent (control [⧫]). Data are expressed as the mean SEM of five determinations.
Effect of ASA or ionomycin pretreatment of T cells on [Ca2+]i mobilization induced by the anti–β2-integrin MoAb KIM127. Cells were incubated with 300 μg ASA, 50 nmol/L ionomycin, or medium for 30 minutes at 37°C, washed, and then tested for mobilization of [Ca2+]i. Arrow indicates addition of KIM127 MoAb (medium [•], ASA [◊], and ionomycin pretreatment [□]) or its solvent (control [⧫]). Data are expressed as the mean SEM of five determinations.
Unstimulated T lymphocytes were then pretreated for 30 minutes with a suboptimal concentration of ionomycin, washed, and tested in the adhesion system, as well as analyzed by flow cytometry for the MoAb 24 staining. The simple incubation with this concentration of ionomycin did not induce the activation conformational change of β2-integrin on T-cell surface (Table 5). However, ionomycin pretreatment induced a decrease not only of T-cell adhesion and migration, but also of the binding of MoAb 24 induced by contact with HUVEC on adherent and migrated cell fractions.
In vitro effect of salicylates on T-cell (3H)-TdR incorporation and IL-2 synthesis.
Increase in [Ca2+]i and activation of PKC are usually followed by complete T-cell activation.49Therefore, we analyzed the possibility that salicylates could induce T-cell proliferation and IL-2 production. The basal T-cell (3H)-TdR incorporation with medium alone (620 ± 250 cpm, n = 3) was enhanced by immobilized anti-CD3 MoAb plus monocytes to 1,850 ± 430 (P .01), 7,860 ± 1,290 (P < .001), and 18,380 ± 4,230 cpm (P < .001) after 24, 48, or 72 hours of culture, respectively. Similar results were obtained when rIL-2 was added to immobilized anti-CD3. On the contrary, T-cell incubation with 300 μg/mL of ASA for a period ranging from 6 to 72 hours did not change the basal (3H)-TdR incorporation (715 ± 330 cpm at 24 hours, 760 ± 350 cpm at 48 hours, and 610 ± 290 cpm at 72 hours, not significant [NS]). In addition, no effects were obtained with 30 and 600 μg/mL of ASA. NaS incubation of T cells gave similar results (data not shown). After 48 hours of culture, the levels of IL-2 in the supernatant of T-cell cultures stimulated with immobilized anti-CD3 plus 1% monocytes were increased (14.4 ± 3.9 IU/mL, n = 3) with respect to those detected in the supernatants of resting T cells (<1 IU/mL, P < .001). The incubation with 30 to 600 μg/mL of either ASA or NaS did not induce any detectable IL-2 activity after 6, 12, 24, and 48 hours of culture (<1 IU/mL).
In vivo effect of salicylates on adhesive and migratory ability of T cells.
Finally, we evaluated whether the observed in vitro effects of salicylates on T-cell adhesion and migration were relevant to their antiinflammatory effects in vivo. Adhesion and migration ability of T cells isolated from the peripheral blood of three healthy volunteers before and after intravenous injection of 500 mg of aspirin was examined. T-cell adhesion and migration ability in the in vitro system was significantly decreased 30 minutes after aspirin injection and the inhibitory effect persisted 2 hours after (Fig 5).
Effect of in vivo injection of ASA on adhesive and migratory in vitro ability of T lymphocytes. Data are expressed as the mean SEM of three separate experiments. P < .05 (○) andP < .01 (*) versus basal values (time 0).
Effect of in vivo injection of ASA on adhesive and migratory in vitro ability of T lymphocytes. Data are expressed as the mean SEM of three separate experiments. P < .05 (○) andP < .01 (*) versus basal values (time 0).
DISCUSSION
The present study shows that salicylates, such as ASA or NaS, decrease the ability of unstimulated T cells to adhere to cytokine-activated HUVEC monolayers and transmigrate through them into collagen in an in vitro static model, which simulates vessel wall and extracellular matrix.37 In these experimental conditions, the adhesion of T cells to HUVEC is mainly mediated by surface molecules of the integrin family.42,43 However, our flow cytometry studies showed that salicylates fail to significantly modify the constitutive expression of integrins on the membrane of resting T cells. Moreover, the slight increase in the expression of the CD11b molecule, already demonstrated for PMN,50 cannot account for the observed decrease in T-cell adhesion induced by salicylates.
On the other hand, integrins also exist in either active or inactive state. Activated T lymphocytes exhibit a greater capacity to adhere to and transmigrate through endothelium than resting T cells and this functional characteristic can be largely explained by upregulation of the binding affinity of integrins induced by activation, without changes in the level of surface expression.15,16 We have confirmed that the selective activation of β1- or β2-integrins, induced by specific MoAbs,31,32leads to a significant enhancement of T-cell adhesion to activated HUVEC. As already shown in previous studies, β2-integrins play a prominent role in the firm attachment to HUVEC and transendothelial migration of T cells, as their specific activation leads to a striking increase in adhesion of T cells and is associated with a significant increase in the number of migrated cells.42 The present demonstration that preincubation of T cells with ASA prevents the stimulating effects of anti-β2 MoAb on adhesion and migration suggests that salicylates block the integrin conformational changes induced by T-cell activation.
The in vivo activation of T cells can be triggered by different mechanisms at the site of inflammation.51,52 Among these, the simple contact with endothelium seems to play a major role in inducing activation antigens on leukocyte surface.44,53 We have shown that the attachment to HUVEC induces the expression on the T-cell surface of a β2 integrin activation epitope, which is correlated with optimal adhesive function.33,45,46 This novel observation adds further knowledge on the effect of endothelium/T-lymphocyte interaction. In this setting, it is tempting to speculate that activation of β2-integrins induced by HUVEC enhances not only adhesive, but also migratory capacity of T lymphocytes, as our experiments have shown that the expression of the neo-epitope recognized by the 24 MoAb was maximal in the migrated cell fraction. Thus, our results, showing that salicylates block the HUVEC-induced appearance of the 24 epitope on T cells, strongly suggest that these drugs can interfere with the recruitment of T lymphocytes toward inflammatory sites by preventing the conformational change of β2-integrins induced by contact with endothelial wall. We cannot rule out that the inhibitory effects of salicylates could be also exerted on other surface molecules involved in emigration. Among these, for example, CD31/platelet-endothelial cell adhesion molecule-1 (PECAM-1) seems to play a key role in the process of diapedesis between endothelial cells.15 However, PECAM-1 seems to be preferentially involved in the emigration of PMN, monocytes, and only a subset of activated T cells,15 54thereby suggesting a minor role of this molecule in the migratory ability of the whole T-cell population.
An expanding literature indicates that integrin activation is dependent on signals coming from the extracellular environment, but is also regulated by intracellular events in an “outside-in” and inside-out” signaling system able to modulate cell adhesion and behavior.15,17,47,48,52 It is of interest that some NSAIDs exert an inhibitory activity on the activation of PMN produced by proinflammatory mediators by interfering with early events of signal transduction.55,56 Moreover, it has been proven that aspirin-like drugs, including sodium diclofenac, indomethacin, or piroxicam, induce an increase in [Ca2+]i, as well as a transient activation of PKC in human T lymphocytes.28 57 The latter observations have been confirmed by the present study using salicylates.
Because it is known that both iCa2+ and PKC are implicated in the regulation of cell adhesion,47,48,52 58 we attempted to address the question of whether the salicylate-induced activation of these twin intracellular signals has a biologic relevance in reducing integrin-mediated adhesiveness of T cells. EGTA, blocking Ca2+ influx, completely reversed the inhibitory effects of salicylates on T-cell adhesion and migration. On the contrary, different PKC inhibitors, with various degrees of selectivity, were unable to restore normal adhesion and migration of T cells treated with ASA or NaS. This suggests that the salicylate-triggered decrease in adhesion and migration of T lymphocytes is a Ca2+, rather than PKC-dependent, phenomenon.
There is now evidence that Ca2+ is a significant player in a complex, feedback coordinated, signaling repertoire, which can modulate leukocyte adhesion. The β2-integrin binding, for example, triggers rapid mobilization of [Ca2+]i,59,60 and, on the other hand, cell adhesion via β2-integrins is directly modulated by changes in [Ca2+]ilevels.61 Some of our experimental observations support the link between the increase of [Ca2+]i and the decrease of integrin-mediated T-cell adhesion induced by salicylates. ASA or NaS inhibit integrin-mediated adhesion of T cells to HUVEC, as well as [Ca2+]i increase induced by MoAb stimulation of β2-integrin. In addition, a concentration of ionomycin, which gives an increase in [Ca2+]i similar to that triggered by salicylates, is able to reduce the expression of 24 epitope elicited by HUVEC, as well as the adhesion and migration of T cells. Interestingly, this concentration of ionomycin, similar to salicylates, does not induce the β2-integrin activation conformational epitope. In contrast, higher ionomycin concentrations (≥100 nmol/L) induce significant binding of the MoAb 24 on T-cell surface (unpublished personal data, November 1997) and enhance β-integrin–mediated T-cell adhesion to endothelium.61 62
Taken together, our data indicate that the inhibitory effect exerted by salicylates on the adhesion of resting T cells to HUVEC may be mediated by triggering a Ca2+ flux, which makes the cell unresponsive to the subsequent Ca2+-mediated integrin activation induced by endothelial contact. In this context, the demonstration that [Ca2+]i depletion in T cells prevents an increase in cell adhesion triggered by anti-CD3 or anti-CD2 MoAbs would agree with this hypothesis.62
PKC and [Ca2+]i play a crucial role in T-cell activation, as they are the two main second messengers generated by the activation of the phosphatidylinositol pathway, which takes place after T-cell receptor stimulation.49,63 However, our data demonstrate that neither ASA nor NaS promote significant T-cell proliferation or IL-2 synthesis. It is conceivable that, depending on the nature of the stimulating ligand, rise in [Ca2+]i and activation of PKC not necessarily lead to the entire range of the T-cell functional repertoire, but may selectively activate a discrete response of T lymphocytes. This is consistent with recent observations showing that the degree of T-cell activation is dependent on the kinetics and the extent of [Ca2+]i elevation and on the type of PKC isoform involved.64 65
The pharmacologic and clinical relevance of these data may be considerable. The present results, showing that ASA or NaS are able to reduce the capacity of circulating resting T lymphocytes to adhere to and transmigrate through endothelial cells activated by proinflammatory cytokines, indicate that salicylates may exert an inhibitory effect on the aspecific recruitment of T cells, which have the potential to contribute to the augmentation and persistence of the inflammatory process. This activity might also be of some relevance to the known protective effect of ASA against ischemic cardiovascular diseases in view of the involvement of extravasated T cells in the processes leading to atheroma formation and plaque disruption.66 In this setting, it is worth noting that our in vitro results were strictly reproduced by the in vivo administration of antiinflammatory doses of ASA to healthy volunteers, where a very strong inhibitory effect on the capacity of circulating T cells to attach to and migrate through endothelium was seen. These findings are in apparent contrast with previous studies showing an increase of PMN adhesion to gut endothelium induced by ASA.8-12 However, the effects of ASA on leukocytes may be tissue-specific or vary according to the activation state of endothelium. In addition, the enhanced PMN adhesion is usually not associated with increased migration (Gerli R., et al, manuscript in preparation).12 It is interesting to note that NaS, which does not share either the cyclooxygenase inhibition or the ulcerogenic actions of ASA,67-69 does not enhance leukocyte adherence to gut endothelium,12 but, like ASA, reduces adherence and migration of T cells. This suggests that the observed effects on T-cell adhesion and migration are probably not dependent on the inhibition of cycloxygenase and PG metabolism. This concept seems to be also supported by the present observation that the ASA or NaS concentrations exerting maximal T-cell inhibition were equivalent to the higher concentrations leading to optimal antiinflammatory effects in vivo, rather than to those sufficient to inhibit PG production.35
In conclusion, we have shown that salicylates can interrupt the activation of β2-integrins on T lymphocytes with consequent reduction of their capacity to adhere to and migrate through endothelium. This effect appears to be mediated by a drug-induced increase in [Ca2+]i. Although NSAIDs are able to enhance [Ca2+]i in several cell types,38 the mechanism of [Ca2+]imobilization is unclear. In human lymphocytes, ASA induces alterations in membrane fluidity, suggesting that partitioning of salicylates into plasma membrane lipids might increase cell-membrane permeability.28,57 70 Compatible with these findings is our observation showing that exposure to salicylates stimulates mainly Ca2+ inflow.
We are aware that our system, exploring only intermediate steps in T-cell/endothelium interaction, does not allow to rule out an interference of salicylates with other phases of the adhesion cascade. In this context, results from our laboratories appear to confirm that these drugs exert inhibitory effects on T-cell rolling along the vessel wall through an interference with L-selectin. Further definition of the influence of different NSAIDs on the ability of T lymphocytes to adhere to endothelial cells will provide new insights into the mechanisms of action of aspirin and its derivatives.
ACKNOWLEDGMENT
We thank Dr Dorian O. Haskard (Rheumatology Unit, Hammersmith Hospital, London, UK) for providing the DREG-200 (anti–L-selectin) MoAb, Dr Martyn Robinson (Celltech Therapeutics Ltd, Berkshire, UK) for the anti-β2 integrin MoAb KIM127, Dr Francisco Sanchez-Madrid (Hospital da la Princesa, Madrid, Spain) for the anti-β2integrin MoAb TS 2/16, and Dr Nancy Hogg (Leukocyte Adhesion Laboratory, Imperial Cancer Research Fund, London, UK) for the MoAb 24.
Address reprint requests to Roberto Gerli, MD, Institute of Internal Medicine and Oncological Sciences, Center for the Study of Rheumatic Diseases, Policlinico di Monteluce, I-06122 Perugia, Italy.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.

![Fig. 4. Effect of ASA or ionomycin pretreatment of T cells on [Ca2+]i mobilization induced by the anti–β2-integrin MoAb KIM127. Cells were incubated with 300 μg ASA, 50 nmol/L ionomycin, or medium for 30 minutes at 37°C, washed, and then tested for mobilization of [Ca2+]i. Arrow indicates addition of KIM127 MoAb (medium [•], ASA [◊], and ionomycin pretreatment [□]) or its solvent (control [⧫]). Data are expressed as the mean SEM of five determinations.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/92/7/10.1182_blood.v92.7.2389/3/m_blod41911004x.jpeg?Expires=1770494169&Signature=hNesQ6RmGMy~aiHsoBB4KFSbhs0rbBdmlr7twUAxTsto6A84ork1c7HRT57FqKGnf1DSK37jWQQFuw1ZrpIJsbWkxWdJPBPnGPjpwLdNNfNOKZIHnBPi5mjHWVX3R-tt48Kda-gCyRZLx4tgdwrADlUZteSRjVt51w-E6qksNx2BXWnyNNoKSWgNNePzWzhj9Gtqa~LHfI0okY5wTzDu9JrTX4ZZfOLPCYf3-j~CsfjBOq7HVec82rBy0xxFJJoorEJ1CZx~PetVjK4JEjrD4LCNaRuvxfIqmXltbo3nPHb4f9WUT6DNjBLe-ARO50UZytO1W-GygTZcfODZ1snTiw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)




![Fig. 4. Effect of ASA or ionomycin pretreatment of T cells on [Ca2+]i mobilization induced by the anti–β2-integrin MoAb KIM127. Cells were incubated with 300 μg ASA, 50 nmol/L ionomycin, or medium for 30 minutes at 37°C, washed, and then tested for mobilization of [Ca2+]i. Arrow indicates addition of KIM127 MoAb (medium [•], ASA [◊], and ionomycin pretreatment [□]) or its solvent (control [⧫]). Data are expressed as the mean SEM of five determinations.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/92/7/10.1182_blood.v92.7.2389/3/m_blod41911004x.jpeg?Expires=1770494170&Signature=qye3dbTiQGw-KSPrV-GvbvN-nsi2W4vqULNSUFlGhO5rmRdU9p78KYC~5EeKQBYXzF~7~7HP4zJ-jaHPgL15i0E13KVMl879Y9LZs6VCaMF0k1LxsP2YWMrCBQiuoPCaHSaogyeniOwJtBSKYaTI7SRmS7rtQJOSfKeum6SC330jGy0Be3t4UJLxdKVuMlNDWZffVVnqodTHKdZHblJvvjrFMNYnddIJvBhHcWQMbgtX1DwT4w8e-w0Nt4a0xwb8b~vqXf~D6xpmzEPR5NPQSKgryFXHqOJjtAVqMLPU6~1xUfqhT0GRDzRPcFXtS0STPeTq0ufshgLIbYqSRetCfA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
