Abstract
X-linked severe combined immunodeficiency (X-SCID) is characterized by an absent or diminished number of T cells and natural-killer (NK) cells with a normal or elevated number of B cells, and results from mutations of the γc chain. The γc chain is shared by interleukin-2 (IL-2), IL-4, IL-7, IL-9, and IL-15 receptors. Recently, a survival signal through the IL-7 receptor (IL-7R) chain was shown to be important for T-cell development in mice and was suggested to contribute to the X-SCID phenotype. In the present study, we examined function of a mutant γc chain (A156V) isolated from an X-SCID patient and found that T cells expressing the mutant γc chain were selectively impaired in their responses to IL-4 or IL-7 compared with the wild-type γc chain expressing cells although responses to IL-2 or IL-15 were relatively maintained. The result shows that IL-4– and/or IL-7–induced signaling through the γc chain is critical for T-cell development and plays an important role in the development of the X-SCID phenotype.
MUTATIONS OF THE γc chain result in X-linked severe combined immunodeficiency (X-SCID), and represent about half the cases of severe-combined immunodeficiency. The characteristic immunological findings in X-SCID are profound impairment of both cellular and humoral immunity due to the absence or markedly diminished number of T cells and natural-killer (NK) cells together with abnormal B-cell function.1,2 Initially, the γc chain was cloned as a third subunit of the interleukin-2 (IL-2) receptor.3,4Subsequently, the γc chain has been shown to participate in the IL-4, IL-7, IL-9, and IL-15 receptor systems.5-11 Thus the profound immunological defects in X-SCID patients were hypothesized as the results of combined signaling defects through a wide range of receptors that use the γc chain. However, recent studies, using mice in which the genes for these cytokines and their receptors have been ablated, suggested more selective defects in cytokine signaling are important for the development of X-SCID phenotype. Gene disruption of either IL-7 or the IL-7–receptor (IL-7R) α subunit leads to severe perturbation of T and B lymphopoiesis similar to that found in γc chain–deficient mice.12-16 In addition, expression of bcl-2, which mediates a survival signal through the IL-7 receptor, rescued T-cell development in IL-7Rα chain knockout mice.17,18 NK cell development was disrupted in IL-2Rβ–deficient mice and in γc-deficient mice but not in IL-2–deficient mice.14-16,19,20 Because the IL-15R consists of IL-2Rβ and γc chains, which are also signaling components of the IL-2 receptor, in addition to a unique IL-15Rα chain, IL-15 is a candidate for an essential cytokine in NK cell development.21,22 In contrast, IL-2 and IL-4 double knockout mice do not show early developmental defects of the immune system indicating that IL-2 and IL-4 are not essential for the development of the immune system in mice.23 The importance of IL-7 and IL-7Rα for T-cell development in humans has also been described and it has been suggested that defects in the IL-7 system contributes to the X-SCID phenotype.24 25 Therefore it is important to examine the function of mutant γc chains isolated from X-SCID patients to confirm this hypothesis.
In the present study, we examine a mutant γc chain isolated from an X-SCID patient, which has an amino acid substitution in the extracellular domain of the γc chain, and show that IL-4– and IL-7–induced signals are selectively diminished in the transfectant cells stably expressing the mutant γc chain compared with the cells expressing the wild-type γc chain. These results show that IL-4 and/or IL-7 play a crucial role in T-cell development and contributes to the X-SCID phenotype.
MATERIALS AND METHODS
The patient, a 3-month-old male, was referred to our hospital with intractable diarrhea, wasting, and pneumonia. His maternal cousin died in early infancy due to fungal infection. In his peripheral blood, there were no detectable circulating T cells although the number of B cells was normal (560/μL). The responsiveness of the lymphocytes to phytohemagglutinin (PHA), concanavalin A (ConA), and mixed lymphocyte culture was markedly reduced. NK activity of the patient was comparable to normal controls. He died of respiratory failure 2 weeks after admission. The mutation in the γc chain of the patient was described previously.26 Briefly, the patient had a C to T point mutation at nucleotide position 481, resulting in one amino acid substitution of valine for alanine (A156V) in the extracellular domain of the γc chain.
Cell lines.
A human T-cell line, ED40515(−), is derived from the peripheral blood of a patient with adult T-cell leukemia.26The T-cell line expresses the IL-2Rα, IL-2Rβ, IL-4Rα, and IL-15Rα chains but not the γc or IL-7Rα chain endogenously (Fig 1). The T cells were cultured in RPMI 1640 medium containing 10% fetal calf serum, penicillin, streptomycin, and gentamycin at 37°C in 10% CO2. Expression vectors for the wild-type γc chain or mutant γc chain (A156V) from the X-SCID patient and the human IL-7Rα chain were stably transfected into ED40515(-) cells along with pSV2neo by electroporation followed by selection in the medium containing G418 (GIBCO BRL, Grand Island, NY) as described previously.26
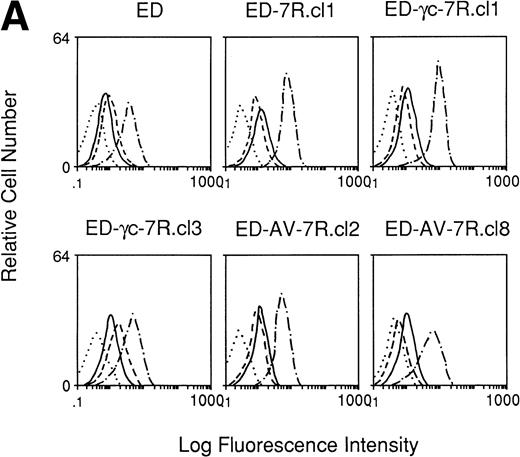
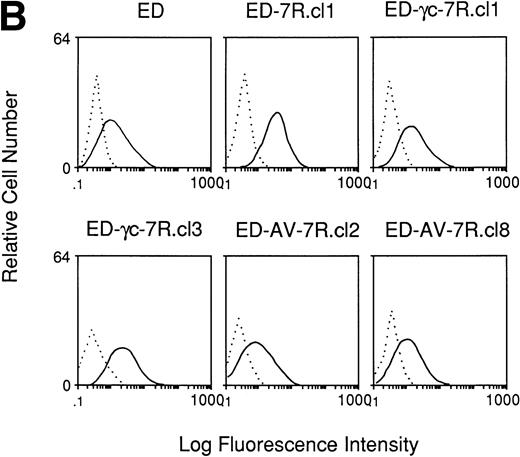
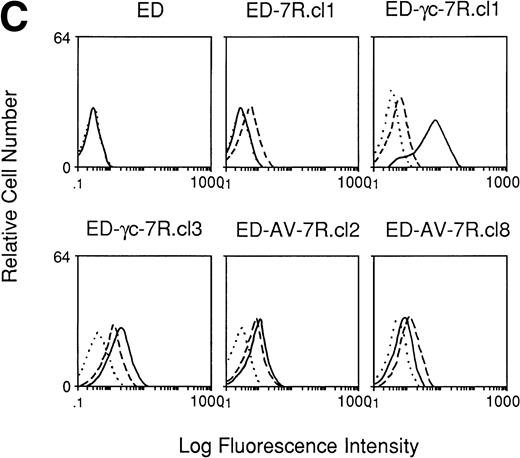
Immunofluorescence staining of receptors on ED40515(-) cells and transfected derivatives. (A) Cells were stained with an anti–IL-15 MoAb, M110 (· · · ·), anti–IL-2Rβ MoAb, TU27 (– · – ·), anti–IL-4R MoAb (—) or anti–IL-15R MoAb, M162 (– – –), followed by PE-conjugated antimouse IgG. (B) FITC-conjugated anti–IL-2R MoAb ( – ) or FITC-conjugated control IgG1 (· · · ·) were used for staining of these cells. (C) Cells were treated with a biotin-conjugated antihuman γc chain MoAb, TUGh4 (—), antihuman IL-7R chain MoAb (– – –) or without antibody (· · · ·) followed by streptavidin-phycoerythrin staining.
Immunofluorescence staining of receptors on ED40515(-) cells and transfected derivatives. (A) Cells were stained with an anti–IL-15 MoAb, M110 (· · · ·), anti–IL-2Rβ MoAb, TU27 (– · – ·), anti–IL-4R MoAb (—) or anti–IL-15R MoAb, M162 (– – –), followed by PE-conjugated antimouse IgG. (B) FITC-conjugated anti–IL-2R MoAb ( – ) or FITC-conjugated control IgG1 (· · · ·) were used for staining of these cells. (C) Cells were treated with a biotin-conjugated antihuman γc chain MoAb, TUGh4 (—), antihuman IL-7R chain MoAb (– – –) or without antibody (· · · ·) followed by streptavidin-phycoerythrin staining.
Cytokines and antibodies.
Purified human recombinant IL-4 was purchased from Pepro Tech (Rocky Hill, NJ), and purified human recombinant IL-2, IL-7, and IL-15 were provided by Ajinomoto Corp (Kanagawa, Japan), Sterling Research Group (Malvern, PA), and Immunex Corp (Seattle, WA), respectively. A rat antihuman γc chain monoclonal antibody (MoAb), TUGh4, and a mouse antihuman IL-7Rα MoAb (Immunex Corp) were conjugated to NHS-LS-biotin (Pierce Chemical Co, Rockford, IL) as described previously.26 A mouse antihuman IL-15Rα MoAb (M162) and a mouse antihuman IL-15 MoAb (M110) were provided by Immunex Corp, and a mouse antihuman IL-4Rα MoAb, fluorescein isothiocyanate (FITC)-conjugated antihuman IL-2Rα MoAb, R-Phycoerythrin–conjugated antimouse IgG and rabbit antimouse Jak3 polyclonal antibodies were purchased from Genzyme (Cambridge, MA), Coulter Corp (Miani, FL), Sigma Chemical Company (St Louis, MO), and Santa Cruz Biotechnology Inc (Santa Cruz, CA), respectively.
Immunofluorescence staining.
The method for immunofluorescence staining was the same as described previously.11 Briefly, 2 × 105 cells were incubated with the first MoAbs for 45 minutes at 4°C. After being washed twice, the cells were incubated with the R-Phycoerythrin– conjugated antimouse IgG or streptavidin-phycoerythrin (Becton Dickinson, San Jose, CA) for 30 minutes at 4°C except for staining of IL-2Rα chain. After being washed twice, the cells were analyzed with an EPICS flow cytometer (Coulter).
Detection of tyrosine phosphorylated Jak3.
Cells were starved for 24 hours in RPMI 1640 media containing 0.02% bovine serum albumin (BSA) followed by stimulation with the indicated amounts of IL-2, IL-4, IL-7, and IL-15 for the indicated times. The cells were lysed with a buffer containing 1% NP-40, 10 mmol/L Tris-HCl (pH7.5), 150 mmol/L NaCl, 1 mmol/L EDTA, 1% Aprotinin, 2 mmol/L Na3 VO4 , 2 mmol/L phenylmethyl sulfonyl fluoride (PMSF) , 0.1 mmol/L Na2MoO4, and 10 mmol/L NaF for 30 minutes at 4°C. After centrifugation, the supernatants were precleared by incubation with protein-A Sepharose CL-4B (Pharmacia, Piscataway, NJ) overnight. The samples were then immunoprecipitated with rabbit antihuman Jak3 polyclonal antibodies for 2 hours at 4°C. The immunoprecipitates were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to Hybond-enhanced chemiluminescence (ECL) membrane (Amersham, Arlington Heights, IL). To detect the phosphotyrosine content, the membrane was sequentially bound with an antiphosphotyrosine MoAb, 4G10 (Upstate Biotechnology Inc, Lake Placid, NY) at a 1:1000 dilution and peroxidase-conjugated sheep antimouse immunoglobin (Ig) (Amersham) at a 1:3000 dilution. The secondary antibody bound to the membrane was detected by ECL (Amersham).
IL-4 and IL-7 binding.
Radiolabeling of human IL-7, binding conditions, and Scatchard analysis were as described previously.11125I-labeled IL-4 was purchased from Amersham. For binding experiments, 1 × 106 cells were incubated with 125I-labeled IL-4 or IL-7 for 2 hours at 4°C in the presence of 0.02% sodium azide and then separated by 1% sucrose. A 200-fold excess of corresponding ligand was used for cold competition. The radioactivity in the cell fraction was measured and the ligand binding was analyzed by Scatchard plot.
RESULTS
Establishment of T-cell transfectants stably expressing the γc and IL-7Rα chains.
From the results of disruption of the IL-7 and IL-7Rα genes, IL-7 has been shown to play a crucial role in the development of T cells in mice.12,13 However, it is difficult to examine the signaling ability of the mutant γc chain in T cells obtained from X-SCID patients because the numbers of T cells are markedly reduced in these patients.1 Thus, we transfected the IL-7Rα chain cDNA alone or in combination with the wild-type or mutant γc chain cDNA into a T-cell line ED40515(−), which lacks endogenous expression of the γc and IL-7Rα chains on the cell surface (Fig 1C). Stable transfectant clones were selected by limiting dilution. Expression of the exogenously introduced γc and IL-7Rα chains was confirmed by flow cytometry with an antihuman γc chain MoAb, TUGh4, and an antihuman IL-7Rα MoAb, respectively (Fig 1C). The stable transfectant clones were termed ED-7R, ED-γc-7R, and ED-AV-7R, which express IL-7Rα chain alone, or along with the wild-type or mutant γc chain, respectively. Expression of endogenous IL-2Rα, IL-2Rβ, IL-4Rα, and IL-15Rα chains was shown in Fig 1A.
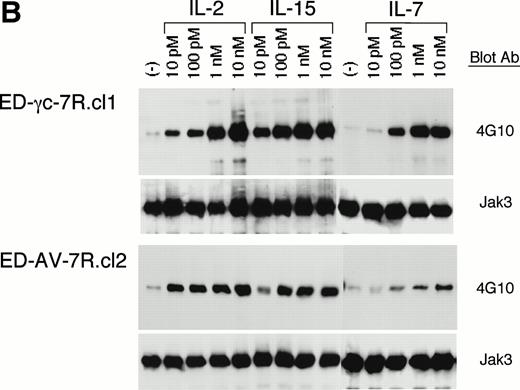
Attenuated IL-4– and IL-7–induced tyrosine phosphorylation of Jak3 in ED cells expressing the mutant γc chain.
To investigate the signal transducing ability of the mutant γc chain, the ED transfectant cells were stimulated with IL-2, IL-4, IL-7, and IL-15. Tyrosine phosphorylation of Jak3 was evaluated as a representative parameter of signaling through the γc chain for the following reasons: Jak3 is the only known signaling molecule directly associated with the γc chain, all cytokines using the γc chain induce rapid tyrosine phosphorylation of Jak3, and a human Jak3-deficiency disease has similar clinical features to a human γc chain–deficient disease, X-SCID.1 27-33
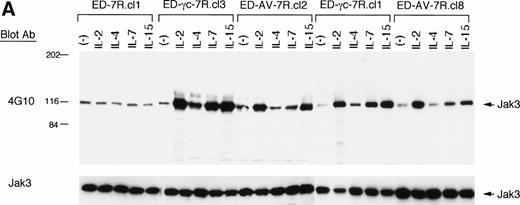
Antiphosphotyrosine immunoblot analysis of Jak3 immunoprecipitates from ED-γc-7R.cl1 and ED-γc-7R.cl3 cells, which express the wild-type γc and IL-7Rα chains, showed phosphorylation of Jak3 in response to 10 nmol/L of IL-2, IL-4, IL-7, and IL-15 (Fig 2A). In contrast, diminished tyrosine phosphorylation of Jak3 on IL-4 or IL-7 stimulation was observed in ED-AV-7R.cl2 and ED-AV-7R.cl8 cells, which express the mutant γc and IL-7Rα chains, although IL-2 or IL-15 induced significant tyrosine phosphorylation of Jak3 (Fig 2A). Such tyrosine phosphorylation of Jak3 was not observed in parental ED40515(−) cells or in ED-7R.cl1 cells after IL-2, IL-4, IL-7, and IL-15 stimulation (Fig 2A and data not shown). Because we observed a minor increase in tyrosine phosphorylation of Jak3 in ED-AV-7R clones in response to 10 nmol/L of IL-7, while this increase was not observed after 10 nmol/L of IL-4 stimulation in these lines, we compared the dose response of IL-7 on tyrosine phosphorylation of Jak3 between ED-γc-7R.cl1 and ED-AV-7R.cl2 cells (Fig 2B). The total phosphotyrosine content of Jak3 increased in proportion to the concentration of IL-7 in ED-γc-7R.cl1 cells. In ED-AV-7R.cl2 cells, in contrast, IL-7 stimulation resulted in only minor increases in Jak3 tyrosine phosphorylation, even at concentrations as high as 10 nmol/L (Fig 2B). As shown in Fig 1, ED-γc-7R.cl1 cells express smaller numbers of IL-7Rα chains than ED-AV-7R.cl2 cells. The results indicate that even with smaller numbers of IL-7Rα chain, the wild-type γc chain is capable of transducing a stronger signal than the mutant γc chain associated with relatively larger numbers of IL-7Rα chains. In contrast, IL-2 or IL-15 stimulation of ED-AV-7R.cl2 cells gave a more robust phosphorylation of Jak3 even at concentrations as low as 100 pmol/L, similar to the wild-type γc chain-expressing ED-γc-7R.cl1 cells. Taken together, these results show that the mutation in the γc chain impairs IL-4 and IL-7 signaling much more than signaling through the IL-2 or IL-15 receptors.
IL-4– and IL-7–induced tyrosine phosphorylation of Jak3 kinase is attenuated in the cells expressing the transfected mutant γc chain obtained from the X-SCID patient. (A) ED-7R.cl1 cells, ED-γc-7R.cl1 cells, ED-γc-7R.cl3 cells, ED-AV-7R.cl2 cells, and ED-AV-7R.cl8 cells were stimulated with 10 nmol/L of IL-2, IL-4, IL-7, and IL-15 for 15 minutes. The cell lysates were immunoprecipitated with anti-Jak3 polyclonal antibodies, separated by SDS-PAGE, and transferred to membranes. Phosphotyrosine was detected by antiphosphotyrosine MoAb, 4G10. The filters were reprobed with the anti-Jak3 polyclonal antibodies to determine the amount of Jak3 in each lane. (B) ED-γc-7R.cl1 cells and ED-AV-7R.cl2 cells were stimulated with various concentration of IL-2, IL-7, and IL-15 for 15 minutes. The cell lysates were immunoprecipitated with anti-Jak3 polyclonal antibodies, and phosphotyrosine-containing proteins were detected by immunoblotting with 4G10. The position of Jak3 is shown by the arrow. Molecular sizes are indicated on the left (in kD).
IL-4– and IL-7–induced tyrosine phosphorylation of Jak3 kinase is attenuated in the cells expressing the transfected mutant γc chain obtained from the X-SCID patient. (A) ED-7R.cl1 cells, ED-γc-7R.cl1 cells, ED-γc-7R.cl3 cells, ED-AV-7R.cl2 cells, and ED-AV-7R.cl8 cells were stimulated with 10 nmol/L of IL-2, IL-4, IL-7, and IL-15 for 15 minutes. The cell lysates were immunoprecipitated with anti-Jak3 polyclonal antibodies, separated by SDS-PAGE, and transferred to membranes. Phosphotyrosine was detected by antiphosphotyrosine MoAb, 4G10. The filters were reprobed with the anti-Jak3 polyclonal antibodies to determine the amount of Jak3 in each lane. (B) ED-γc-7R.cl1 cells and ED-AV-7R.cl2 cells were stimulated with various concentration of IL-2, IL-7, and IL-15 for 15 minutes. The cell lysates were immunoprecipitated with anti-Jak3 polyclonal antibodies, and phosphotyrosine-containing proteins were detected by immunoblotting with 4G10. The position of Jak3 is shown by the arrow. Molecular sizes are indicated on the left (in kD).
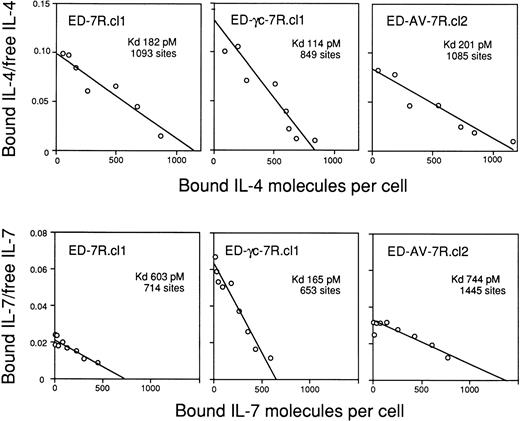
Scatchard plot analyses of 125I-labeled IL-4 and IL-7 binding to the ED40515 (-) and its transfected derivatives expressing IL-7R alone or with the wild-type or mutant γc chain. The cells were incubated with 125I-IL-4 or125I-IL-7 and binding site and kD values were calculated by Scatchard analysis.
Scatchard plot analyses of 125I-labeled IL-4 and IL-7 binding to the ED40515 (-) and its transfected derivatives expressing IL-7R alone or with the wild-type or mutant γc chain. The cells were incubated with 125I-IL-4 or125I-IL-7 and binding site and kD values were calculated by Scatchard analysis.
The mutant γc chain did not contribute to IL-4 and IL-7 binding affinity.
The transfected cell lines were further examined for their125I-IL-4 and 125I-IL-7 binding abilities. The apparent numbers of ligand-binding sites and binding affinities on the cell surfaces of the transfectants were calculated by Scatchard analysis. ED-γc-7R.cl1 cells displayed a single affinity of 114 pmol/L and 849 sites and of 165 pmol/L and 653 sites to IL-4 and IL-7, respectively, whereas ED-AV-7R.cl2 cells bound IL-4 and IL-7 with a kd of 201 pmol/L and 1085 sites and of 744 pmol/L and 1445 sites, respectively (Fig 3). Because the binding affinities of ED-AV-7R.cl2 cells to IL-4 and IL-7 were similar to those of ED-7R.cl1 cells (182 pmol/L, 1093 sites and 603 pmol/L, 714 sites, respectively), the mutant γc chain was unable to increase the binding affinity of IL-4 and IL-7 in these cells (Fig 3).
DISCUSSION
Cytokines are a series of soluble proteins that play important roles in immune regulation and their signals are mediated through their specific receptors. X-SCID is the first example of an immunodeficiency disease that is caused by mutation of a cytokine receptor, the γc chain, and so far about 150 mutations have been reported in the database at the website http://www.nhgri.nih.gov/DIR/LGT/SCID.34 Recently, a human Jak3-deficiency disease that has similar clinical features to X-SCID has been described.32,33 Because Jak3 kinase is the only known molecule directly associated with the γc chain, and the phenotypes of X-SCID and Jak3 deficiency are similar, the γc-Jak3 signaling pathway has been suggested to be crucial for T-cell development and to contribute to the X-SCID phenotype.30-33In this report, we show that IL-4– or IL-7– but not IL-2– or IL-15–induced tyrosine phosphorylation of Jak3 was diminished in ED transfectant cells expressing the mutant γc chain obtained from an X-SCID patient. Because the mutation of the γc chain is located in the extracellular domain, the different levels of tyrosine phosphorylation of Jak3 are likely due to different ligand-binding abilities of the mutant γc chain. The γc chain binds ligands together with their private receptor subunits, although it does not bind any known cytokines by itself.3-10 The γc chain has two predicted discrete folding domains consisting of seven β-strands like other type-I cytokine receptors.35,36 This double-barrel structure is connected by a hinge region in which the conserved Ala156-Pro157 residues in the γc chain immediately precede the first β-strand of the C-terminal domain. Helical cytokines bind to the N-terminal barrel of the extracellular domain of their receptors. Because the mutation in the X-SCID patient is located at Ala156 in the γc chain, the angle of the double-barrel structure may be altered and ligand-binding properties could be affected. As shown in the previous report, ED cells expressing the mutant γc chain could not bind IL-2 in the presence of anti–IL-2Rα MoAb, H31 although they bound IL-2 with comparable affinity to ED cells expressing the wild-type γc chain.26In the present study, we showed that the binding affinities of ED cells expressing the mutant γc chain to IL-4 and IL-7 are affected. The IL-15Rα chain by itself binds IL-15 with high affinity in the absence of other subunits21,22 and once the IL-15Rα chain associates with the IL-2R/IL-15R βγ heterodimer, low concentrations of IL-15 might be able to transduce a signal through the mutant γc chain. Interestingly, our patient has normal NK activity in his peripheral blood. Taken together with our observation that the mutant γc chain could transduce an IL-15–induced signal, the mutant γc chain might be partially functional for NK–cell development and as a result, the X-SCID patient might have his own NK cells. Of note, there is a report of X-SCID patients with identical genotype, one with and others without NK cells and NK activities.37 Factors other than the γc chain might influence NK–cell development or alternatively, maternal NK cells might have been transplacentaly transfused into the peripheral blood of the X-SCID patient as previously described for T cells of X-SCID and SCID patients.38
In the present study, we show that IL-4– and IL-7–induced signals are particularly attenuated, compared with IL-2 and IL-15, in the ED transfectant cells stably expressing the mutant γc and IL-7Rα chains. The result shows that IL-4 and/or IL-7 plays a crucial role in T-cell development and contributes to the X-SCID phenotype. As described above, IL-7 has been shown to be important factor for T-cell development in mice.12,13 In contrast, thymus and T-cell subsets develop normally in IL-4–knockout mice indicating that IL-4 is not essential for development of immune system in mice.39In addition, although IL-4 stimulation of X-SCID B cells did not result in Jak3 phosphorylation, other IL-4 substrates including Jak1, IRS-1, and STAT6 were phosphorylated.40 Thus, IL-7 is more likely to play an important role in T-cell development and to contribute to the X-SCID phenotype than IL-4. However, we could not rule out the possibility that not only IL-7 but also IL-4 contribute to the X-SCID phenotype. Further analyses of mutant γc chains obtained from X-SCID patients and the identification of individuals with mutations in these genes will be needed to address this issue.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Satoru Kumaki, MD, Department of Pediatric Oncology, Institute of Development, Aging and Cancer, Tohoku University, 4-1 Seiryo-Machi, Sendai 980-8575, Japan; e-mail:kumakis@europa.idac.tohoku.ac.jp.