Abstract
Cell adhesion molecules have a key role in the migration of T cells to inflammatory foci. However, the effect of the endothelial-lymphocyte interaction on the activation of the latter cells remains unresolved. We have studied the effect of resting and stimulated endothelial cells (ECs) on the activation of peripheral blood T cells (PBTLs), as assessed by the expression of CD69 and CD25 activation antigens. The incubation of PBTLs with tumor necrosis factor-–activated EC monolayers, either alive or fixed, induced the expression of CD69 but not CD25, preferentially in the CD8+CD45RO+ cell subset. Furthermore, it induced the production of cytokines such as IFN-γ, but not that of interleukin-2 (IL-2) and IL-4. EC treated with other stimuli such as IL-1β, IFN-γ, or lipopolysaccharide also showed the same proactivatory effect on T cells. Lymphocyte activation was almost completely inhibited by blocking anti-CD18 and anti–intercellular adhesion molecule-1 (anti–ICAM-1) monoclonal antibodies (MoAbs), but only slightly affected by MoAbs against CD49d, vascular cell adhesion molecule-1, and anti–IL-15. In addition, the interaction of PBTL with immobilized ICAM-1 induced CD69 expression in the same memory T-cell subset. IL-15 induced T-cell activation with expression of CD69 and CD25, and production of IFN-γ, and its effect was additive with that triggered by cell adhesion to either EC or immobilized ICAM-1. The transmigration of PBTLs through either confluent EC monolayers or ICAM-1–coated membranes also induced efficiently the expression of CD69. When IL-15 was used as chemoattractant in these assays, a further enhancement in CD69 expression was observed in migrated cells. Together these results indicate that stimulated endothelium may have an important role in T-cell activation, through the lymphocyte function antigen-1/ICAM-1 pathway, and that IL-15 efficiently cooperates in this phenomenon. These observations could account for the abundance of CD69+ cells in the lymphocytic infiltrates of several chronic inflammatory diseases.
THE DEVELOPMENT AND progression of chronic, immune-mediated inflammatory diseases is dependent on the persistent infiltration of mononuclear cells into the affected tissues.1 Although different cell types have been identified in inflammatory infiltrates, T cells seem to play a central role in the initiation and perpetuation of chronic inflammation.2 Adhesion receptors, including the lymphocyte function antigen-1 (LFA-1; CD11a/CD18) and very late antigen-4 (CD49d/CD29) integrins, mediate the firm adhesion and transmigration of T cells through activated endothelial cells (ECs) by binding to their counter-receptors, intercellular adhesion molecule-1 (ICAM-1)/ICAM-2 and vascular cell adhesion molecule-1 (VCAM-1).3,4 In addition, adhesion molecules play an important role in signal transduction and in the costimulation of T cells during their activation through the TCR/CD3 complex.5 6
Interleukin-15 (IL-15) is synthesized by several cell types and is involved in the proliferation and activation of T cells.7,8This cytokine also induces inflammatory cell recruitment in vivo and T-cell migration in chemotactic assays in vitro.9-11 In addition, IL-15 has a noticeable effect on lymphocyte polarization and redistribution of adhesion molecules and chemokine receptors.12,13 The widespread tissue expression of IL-15 mRNA is not consistent with IL-15 protein synthesis because this cytokine seems to be subjected to a significant posttranscriptional regulation.14,15 These multiple levels of regulation prevent undesirable IL-15 expression in tissues. IL-15 has been detected at sites of chronic inflammation, such as the rheumatoid arthritis (RA) synovium,16 where it is involved in the recruitment and activation of T cells, thus facilitating macrophage activation and tumor necrosis factor-α (TNF-α) synthesis, which is crucial for joint destruction.17 In this regard, it has been proposed that T-cell–macrophage interactions are mediated by the LFA-1/ICAM-1 adhesion pathway and the binding of CD69, which is expressed at high levels in T cells from chronic inflammatory lesions, with its putative ligand.17
The phenotype of T cells that have migrated to chronic inflammatory sites is uncommon and somehow paradoxical; these cells show an increased expression of CD69 and CD45RO with a weak expression of the intermediate activation antigen CD25.1,18,19 The phenotype of these infiltrating T cells could be explained by their selective migration from the peripheral blood during the recirculation of these cells. Conversely, the phenotype of these cells may be acquired during their recruitment through the activated endothelium at inflamed tissues. In this regard, it has been reported that the majority of T cells in the rheumatoid synovium are nonspecifically recruited bystander T lymphocytes.2 However, the possible role of the endothelium in the activation of T cells that migrate to inflammatory foci is still under discussion.20-23
In this study, we used an in vitro model to analyze the effect of endothelium on the activation of peripheral blood T cells (PBTLs). We found that TNF-α–activated endothelium induces the expression of CD69 and synthesis of IFN-γ on PBTLs and that this effect is mediated through the LFA-1/ICAM-1 interaction. The role of IL-15 in the induction of T-cell activation in the presence or in the absence of ECs or ICAM-1 was also analyzed. Our results indicate that the transmigration through endothelium in response to IL-15 may account for the antigen-independent activation of T cells observed in chronic inflammation.
MATERIALS AND METHODS
Reagents, cytokines, monoclonal antibodies (MoAbs), and protein substrata.
Recombinant human (rh)IL-15, and rhMIP-1α (purity >98%, endotoxin level <0.1 ng/mg cytokine) were obtained from PeproTech EC Ltd (London, UK); rhTNF-α (specific activity 5 × 107U/mg, purity >95%) was provided by Genetech (San Francisco, CA); rhIFN-γ (specific activity 4.75 × 107 U/mg) was purchased from Genzyme Diagnostics (Cambridge, MA); rhIL-1β (specific activity 4 × 108 U/mg) was obtained from Promega (Madison, WI); and lipopolysaccharide (LPS) (Escherichia coli055:B5) and phorbol myristate acetate (PMA) were purchased from Sigma Chemical Co (St Louis, MO). Brefeldin A and the calcium ionophore A23187 were obtained from Calbiochem (La Jolla, CA).
The following murine MoAbs to human antigens were used: the anti-CD3 (Leu 4, phycoerythrin [PE] or peridinin chlorophyll protein [PerCP] conjugated), anti-CD4 (Leu3a, PE conjugated), anti-CD8 (Leu2a, PE conjugated), anti-CD14 (LeuM3, PE conjugated), anti-CD25 (anti–IL-2R, fluorescein isothiocyanate [FITC] conjugated), anti-CD45RO (Leu45RO, PE conjugated), anti–HLA-DR (HLA-DR, FITC conjugated). All were purchased from Becton Dickinson (Mountain View, CA). The anti-CD69 (TP1/55, biotin conjugated), anti-CD14 (MO2), anti-CD16 (KD1), anti-CD19 (Bu12), anti–ICAM-1 (RR1/1, kindly provided by Dr R. Rothlein, Boehringer Ingelheim, Ridgefield, CT), anti–VCAM-1 (4B9, a generous gift of Dr J. Harlan, University of Washington, Seattle, WA), anti-CD18 (Lia3/2), anti-CD49d (HP2/1), and the anti-MHC I (W6/32) have been previously described.24-28 The anti–IL-15 MoAb was provided by Immunex (Seattle, WA). The anti–hIL-2 PE (MQ1-17H12), the anti–hIL-4 PE (8D48), the anti–hTNF-α PE (Mab 11), and the anti–hIFN-γ PE (4S.B3) were purchased from Pharmingen (San Diego, CA). P3X63 myeloma protein (IgG1, kappa) was used as negative control in immunofluorescence studies.
Recombinant chimeric ICAM-1-Fc and VCAM-1-4D-Fc, consisting of the total extracellular domains fused to IgG1 Fc fragment, were obtained as described.29 Briefly, COS-7 cells were transiently transfected with pICAM-1-Fc and pVCAM-1-4D-Fc (ICAM-1 and VCAM-1-4D cDNAs cloned in pCD8IgG1). After 4 days, culture supernatants were precipitated with ammonium sulphate, and thereafter chimeric proteins were isolated by using protein A coupled to Sepharose (Pharmacia Fine Chemicals, Uppsala, Sweden). Fibronectin (FN) and Poly-L-Lysine (PLL) were purchased from Sigma, and bovine serum albumin (BSA) from Boehringer Mannheim GmbH (Mannheim, Germany).
Cells and cell lines.
Peripheral blood lymphocytes (PBLs) were isolated from fresh human blood by Ficoll-Hypaque density gradient centrifugation (Pharmacia), followed by two steps of cell adherence on plastic flasks (Costar Corp, Cambridge, MA) at 37°C for 1 hour. Peripheral blood T lymphocytes (PBTLs) for chemotactic assays were purified from PBLs by incubation with a mixture of anti-CD19 (Bu12), anti-CD16 (KD1), and anti-CD14 (MO2) MoAbs for 30 minutes at 4°C. Then, cells were washed twice and incubated with magnetic beads (Dynabeads; Dynal, Oslo, Norway) conjugated with goat anti-mouse IgG, at a 1:20 target/bead ratio for 1 hour on a rotating wheel at 4°C. The negative selected cell population was always >97% CD3+ as assessed by flow cytometry analysis. Isolated cells were washed and resuspended in RPMI 1640 (Flow Lab, Irvine, Scotland) containing 10% fetal calf serum (FCS; Flow Lab) for the assays.
The human dermal microvascular EC line HMEC-1 has previously been described30 and was kindly provided by Drs Ades and Lawley (Centers for Disease Control and Prevention and Emory University School of Medicine, Atlanta, GA). These cells were grown in MCDB 131 medium (GIBCO-BRL, Paisley, Scotland) supplemented with 20% FCS, 10 ng/mL epithelial growth factor (Promega), 1 μg/mL hydrocortisone (Sigma), 20 mmol/L Hepes, and 10 mmol/L L-glutamine. Human umbilical vein endothelial cells (HUVECs) were isolated and cultured as previously described.31 Cells were seeded on tissue culture flasks or dishes coated with gelatin 0.5% and grown in 199 medium (Bio Whitaker, Verviers, Belgium) supplemented with 20% FCS, 50 IU/mL penicillin, 50 μg/mL streptomycin (ICN Biomedicals, Costa Mesa, CA), 250 μg/mL fungizone (Squibb Industria Farmacéutica, Barcelona, Spain), 50 μg/mL EC growth supplement (prepared from bovine brain), and 100 μg/mL heparin (Sigma), and used up to the third passage.
Lymphocyte transmigration assays.
The migration of T cells through a confluent monolayer of HMEC-1 was assayed in chemotaxis Transwell cell culture chambers (Costar), as described.29 The chemotaxis chambers are separated by a polycarbonate membrane of 6.5-mm diameter, 10-μm thickness, and 8-μm diameter pore size. Filters were coated on their upper surface with fibronectin and layered with HMEC-1, and the lower wells of the chambers were then filled with culture medium. The integrity of the EC layer was assessed by diffusion of a trypan blue-albumin complex across the endothelial monolayer, as described.32 Only cell monolayers with permeability ≤0.5% were used for transendothelial migration assays. Each transendothelial migration assay was performed using lymphocytes from a single donor and HMEC-1 cells from the same batch. Additional transmigration assays were performed in Transwell chambers of 3-μm pore size coated with either purified fibronectin (20 μg/mL) or ICAM-1 (20 μg/mL). Transmigration assays were performed in MCDB-131 + RPMI-1640 (1:1) culture media supplemented with 0.5% human serum albumin. A total of 106 T lymphocytes (100 μL) were poured into the upper chamber and 600 μL of medium with different stimuli were deposited in the lower chamber. As control, T cells were incubated with these cytokines in the absence of ECs. PBTLs from the upper and lower chambers as well as from control plates were obtained after 16 hours of incubation at 37°C and 5% CO2, and counted and analyzed for their expression of activation antigens.
Culture of T cells with EC and protein substrata, detection of intracellular cytokines, and immunofluorescence flow cytometry analysis.
Confluent EC cultures plated in 24-well plates (Costar) precoated with 0.5% gelatin were stimulated with TNF-α (20 ng/mL), IL-1β (1 ng/mL), IFN-γ (250 U/mL), or LPS (50 ng/mL) for 20 hours at 37°C to induce a maximal expression of the adhesion molecules ICAM-1 and VCAM-1. In most of the assays, the EC monolayers were then fixed with 1% formaldehyde for 10 minutes and then extensively washed with Tris buffer saline. PBLs were then added at 5 × 105cells/well and incubated for 18 hours. Afterwards, cells were collected, and when indicated, adherent and nonadherent PBLs were carefully separated as previously described.23 In the rest of the assays a population enriched in adherent cells (70% to 80%) was analyzed. To study the effect of the interaction of T cells with different protein substrata on the expression of activation antigens, 24-well plates were coated with different concentrations of purified proteins in 0.1 mol/L Tris pH 8.2 and incubated at 4°C for 16 hours. Plates were washed and used in the assay, as stated above. For the detection of the production of cytokines, T cells were incubated for 48 hours with different stimuli and brefeldin A (1 μg/mL) was added during the last 10 hours of culture to inhibit the secretion of cytokines. PBLs were stimulated with PMA (50 ng/mL) and the calcium ionophore A23187 (1 μmol/L) in the presence of brefeldin A for 10 hours and used as positive control for the detection of IL-2, TNF-α, and IFN-γ. PBLs were activated with anti-CD3 and cultured with IL-2 and IL-4 for 48 hours before stimulating them with PMA and ionophore in the presence of brefeldin A as stated above for obtaining the positive control for the production of IL-4.
Lymphocytes were collected after the assays and incubated for 30 minutes at 4°C in phosphate-buffered saline (PBS) with the primary MoAb, washed twice in PBS, 2% normal human serum, 0.1% sodium azide, and then incubated for 30 minutes at 4°C with the appropriate secondary antibody: FITC-conjugated rabbit anti-mouse F(ab′)2 (Dako, Glostrup, Denmark), PE-conjugated avidin (Pierce, Rockford, IL), or FITC-conjugated avidin D (Vector, Burlingame, CA). Then, cells were additionally labeled with PE-, FITC-, and PerCP-conjugated MoAbs. For intracellular cytokine staining, the collected cells were first stained for the cell surface markers (biotinylated CD69 plus avidin-FITC and CD3 PerCP) and then fixed in 4% paraformaldehyde and permeabilized with 0.1% saponin. Then the anti-cytokine PE MoAbs were incubated for 30 minutes at 4°C in the presence of 0.1% saponin, washed, and analyzed. A minimum of 5,000 cells was analyzed by two- or three-color immunofluorescence on a FACScan flow cytometer (Becton Dickinson) using the Lysis II software.
RESULTS
Effect of ECs on the expression of activation markers by PBTLs.
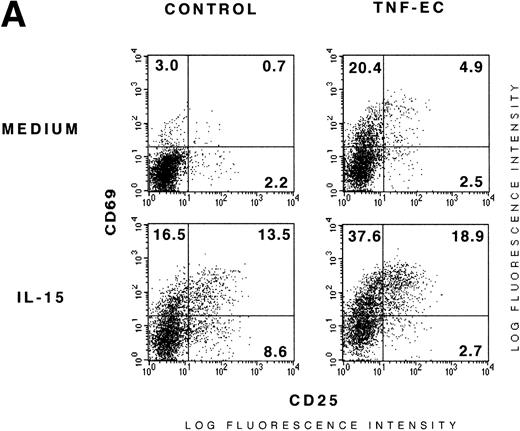
We examined the influence of endothelium on the activation state of PBTLs, monitorized by the expression of CD69, CD25, and HLA-DR. There was a significant increase in CD69 expression on PBTLs after their coculture with TNF-α–activated HUVEC monolayers for 18 hours, whereas nonstimulated EC did have a weak effect (Fig 1A and Table 1). To determine whether the effect of TNF-α–activated endothelium on T lymphocytes was mediated through adhesion molecules or soluble factors secreted by ECs, we studied the induction of activation markers in both adherent and nonadherent PBTLs (Table 1). We found that the T cells that were unable to adhere to activated ECs only showed a slight increase in the expression of CD69, whereas the adhered lymphocytes showed a noticeable increase in the expression of CD69 as well as a modest but consistent enhancement in HLA-DR+ cells (Table 1). The expression of CD97, another early activation antigen, was upregulated in the same manner as CD69 (data not shown). Additional experiments showed that culture supernatants from either resting or TNF-α–activated EC failed to induce CD69 expression on PBTLs (not shown). The induction of CD69 expression by TNF-α–activated ECs in PBTLs was independent of the concentration of monocytes present in the cell cocultures (data not shown). The expression of CD25 was not induced in either adherent or nonadherent cells (Fig 1A and Table 1). We therefore focused our studies in a population enriched in adherent cells (70% to 80%) in the rest of the assays.
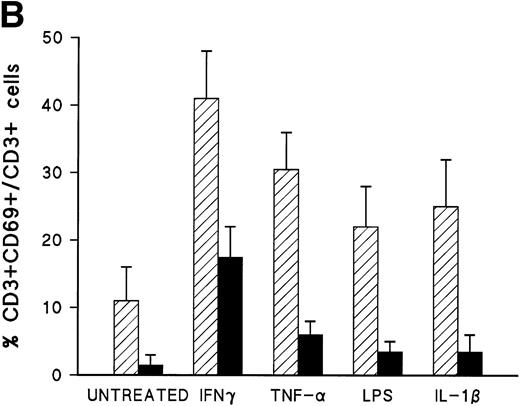
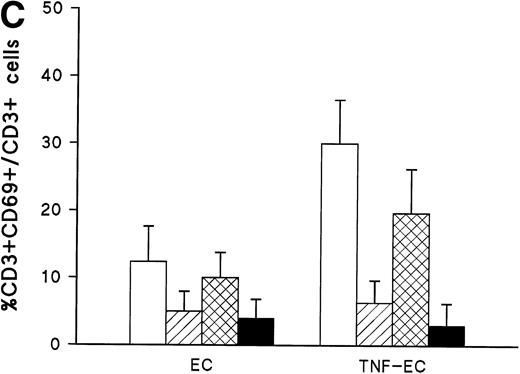
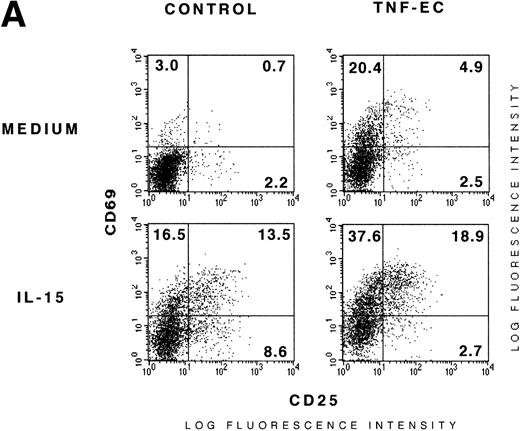
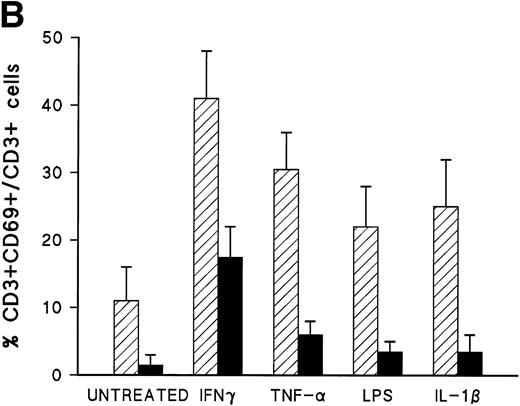
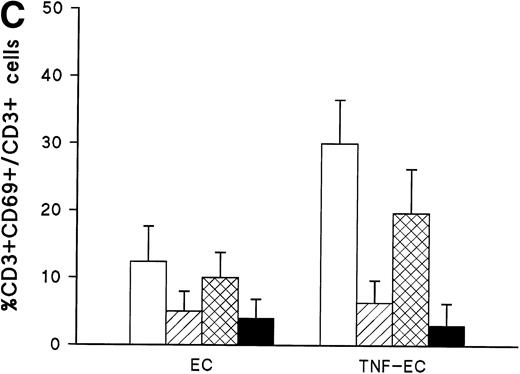
ECs induce the expression of CD69 on PBTLs. (A) ECs induce the expression of CD69 but not CD25 on PBTLs. PBLs were incubated alone (control) or on fixed TNF-–activated EC monolayers (TNF-EC). After 18 hours of culture, CD69 and CD25 expression on CD3+ cells was analyzed. Dotted lines represent negative control corresponding to P3X63. Numbers correspond to the percent of positive cells. A representative experiment out of three is shown. (B) Induction of CD69 T-cell expression by ECs activated with different stimuli. ECs were incubated with medium alone (untreated) or with IFN-γ (250 U/mL), TNF- (20 ng/mL), LPS (50 ng/mL), and IL-1β (1 ng/mL) for 20 hours at 37°C, fixed, and extensively washed. Then, PBLs pretreated or not with the blocking anti–ICAM-1 RR1/1 MoAb were added to wells containing medium or fixed HUVEC. After 18 hours, CD69 expression in CD3+ T cells was measured. The percentage of induction over the control level is shown as arithmetic mean ± 1 standard deviation (SD). The results correspond to three independent experiments. (▨), EC; (▪), EC + anti–ICAM-1. (C) Effect of adhesion receptor blockade on EC-mediated activation of T cells. PBLs preincubated 30 minutes at 4°C with blocking anti-CD18 Lia3/2 and anti-CD49d HP2/1 MoAbs were added to confluent monolayers of resting and TNF-–activated ECs and incubated for 18 hours. Then, the expression of CD69 on CD3+ cells was analyzed by two-color flow cytometry. Control cells corresponded to PBLs incubated in the absence of ECs. The percentage of induction over the control level is shown as arithmetic mean ± 1 SD, and the results correspond to three independent experiments. (□), no MoAb; (▨), anti-CD18; (▩), anti-CD49d; (▪), anti-CD18 + anti-CD49d.
ECs induce the expression of CD69 on PBTLs. (A) ECs induce the expression of CD69 but not CD25 on PBTLs. PBLs were incubated alone (control) or on fixed TNF-–activated EC monolayers (TNF-EC). After 18 hours of culture, CD69 and CD25 expression on CD3+ cells was analyzed. Dotted lines represent negative control corresponding to P3X63. Numbers correspond to the percent of positive cells. A representative experiment out of three is shown. (B) Induction of CD69 T-cell expression by ECs activated with different stimuli. ECs were incubated with medium alone (untreated) or with IFN-γ (250 U/mL), TNF- (20 ng/mL), LPS (50 ng/mL), and IL-1β (1 ng/mL) for 20 hours at 37°C, fixed, and extensively washed. Then, PBLs pretreated or not with the blocking anti–ICAM-1 RR1/1 MoAb were added to wells containing medium or fixed HUVEC. After 18 hours, CD69 expression in CD3+ T cells was measured. The percentage of induction over the control level is shown as arithmetic mean ± 1 standard deviation (SD). The results correspond to three independent experiments. (▨), EC; (▪), EC + anti–ICAM-1. (C) Effect of adhesion receptor blockade on EC-mediated activation of T cells. PBLs preincubated 30 minutes at 4°C with blocking anti-CD18 Lia3/2 and anti-CD49d HP2/1 MoAbs were added to confluent monolayers of resting and TNF-–activated ECs and incubated for 18 hours. Then, the expression of CD69 on CD3+ cells was analyzed by two-color flow cytometry. Control cells corresponded to PBLs incubated in the absence of ECs. The percentage of induction over the control level is shown as arithmetic mean ± 1 SD, and the results correspond to three independent experiments. (□), no MoAb; (▨), anti-CD18; (▩), anti-CD49d; (▪), anti-CD18 + anti-CD49d.
Next, we assayed whether ECs activated by stimuli other than TNF-α were also able to induce CD69 expression in PBTLs. ECs were activated for 20 hours with the indicated stimuli and then fixed, before the incubation with PBLs. As shown in Fig 1B, the stimulation of HUVEC by IFN-γ, LPS, and IL-1β also enabled them to induce the expression of CD69 on T cells. We next characterized by three-color flow cytometry analysis the subset of PBTLs that was preferentially activated by ECs. We found that a larger fraction of CD8+ cells expressed CD69 as compared with CD4+ lymphocytes (Table 2). However, because CD4+ cells are more abundant, both cell subsets comparably contributed to the pool of CD3+ CD69+lymphocytes. On the other hand, CD45RO+ cells were more responsive to ECs compared with the reciprocal CD45RO− subset (Table 2).
Involvement of the LFA-1/ICAM-1 adhesion pathway on the activation of T cells.
The above data prompted us to explore the role of β2 and β1 integrins in CD69 induction by using blocking MoAbs. The blockade of the LFA-1/ICAM-1 adhesion pathway by the anti-CD18 Lia3/2 MoAb or the anti–ICAM-1 RR1/1 MoAb abrogated the activation of PBTLs by ECs activated with different stimuli. In contrast, the anti-CD49d HP2/1 and the anti–VCAM-1 4B9 MoAb only slightly affected the expression of CD69 (Fig 1B and C and Table 3). The inhibitory effect of anti–ICAM-1 MoAb was partial in the case of IFN-γ–activated endothelium, and was increased by the addition of MoAb anti–LFA-3 and anti-CD2 (data not shown). These effects were observed in cell cocultures with both intact and fixed ECs. A blocking anti–major histocompatibility class I (anti–MHC class I) MoAb did not display any significant effect (Table 3).
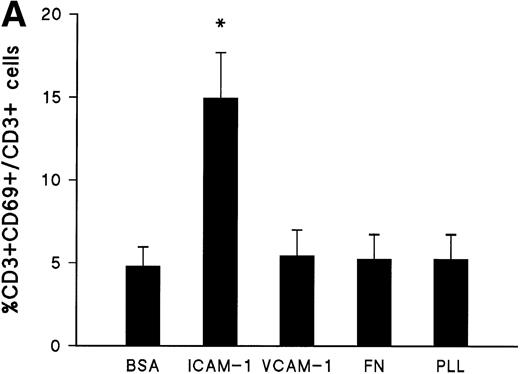
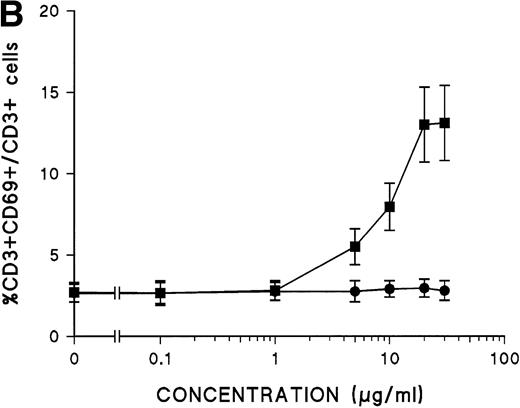
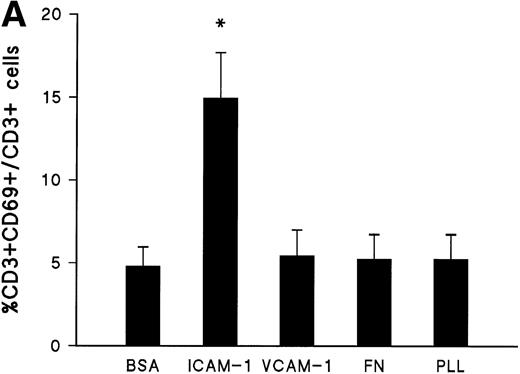
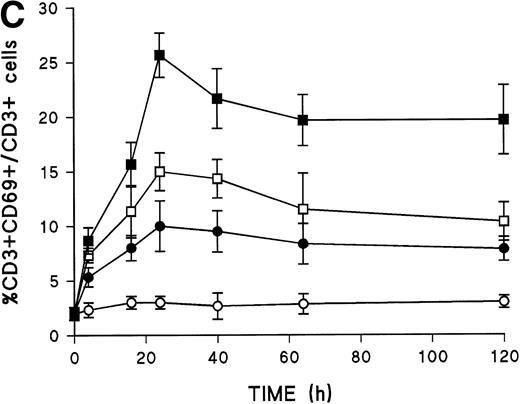
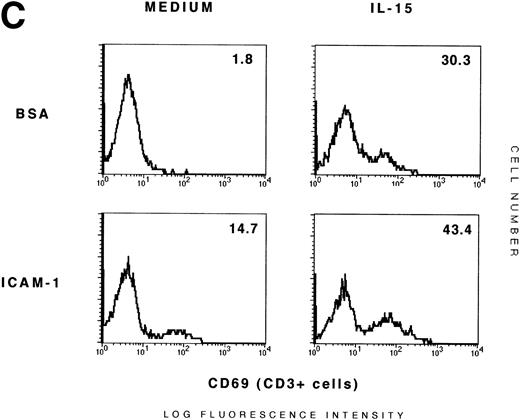
To further confirm the involvement of LFA-1/ICAM-1 adhesion pathway on the activation of PBTLs on interaction with endothelium, we studied the effect of purified EC adhesion molecules on the expression of CD69 by T cells. As shown in Fig 2A, the binding of T cells to immobilized ICAM-1 also induced a significant expression of CD69, an effect that was abolished by a blocking anti-CD18 MoAb (data not shown). In contrast, other adhesion receptor ligands such as VCAM-1 and FN as well as other substrata such as BSA or PLL did not affect CD69 expression (Fig 2A and B). The expression of CD69 induced by interaction with ICAM-1 was dose dependent with an evident effect at 5 μg/mL of ICAM-1 and a maximal induction at 20 μg/mL (Fig 2B). In contrast, the induction of CD25 expression was not observed under these experimental conditions, at any of the doses of ICAM-1 tested (data not shown). Kinetics studies on CD69 expression by PBTLs in response to ICAM-1 showed a slight increment after 4 hours of incubation, reaching a maximum at 24 hours, and remaining significantly elevated for several days (Fig 2C). The phenotypic characterization of CD69+ T lymphocytes activated by ICAM-1 also showed a predominance of CD8+ and CD45RO+ cells (Table2).
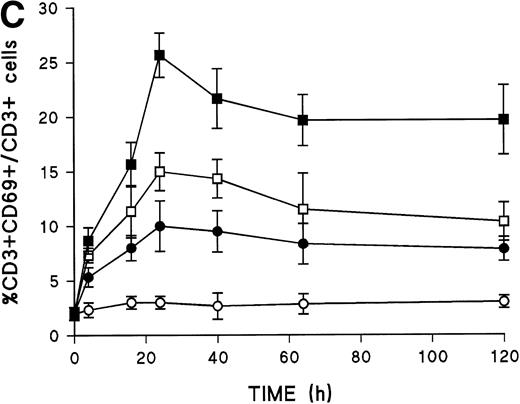
Induction of CD69 expression by T-cell interaction with immobilized ICAM-1. (A) PBLs were added to wells precoated with BSA (1%), rsICAM-1 (20 μg/mL), rsVCAM-1 (20 μg/mL), FN (20 μg/mL), and PLL (40 μg/mL). After 18 hours of incubation at 37°C, CD69 expression was measured in CD3+ cells by two-color flow cytometry. The results of three independent experiments are depicted as arithmetic mean ± 1 SD. *, P < .01 compared with BSA (Mann-Whitney U test). (B) ICAM-1 dose-dependent T-cell activation. PBLs were incubated on wells precoated with different concentrations of rsICAM-1 (▪) or rsVCAM-1 (•). After 18 hours, CD69 expression was analyzed in CD3+ cells. The results of four independent experiments are represented as arithmetic mean ± 1 SD. (C) Kinetics analysis of CD69 T-cell expression induced by rsICAM-1 and IL-15. PBLs were incubated on BSA (1%) or rsICAM-1 (20 μg/mL) precoated wells, and then IL-15 (5 ng/mL) was added where indicated. After 4, 16, 24, 40, 62, and 120 hours, cells were collected and CD69 expression was measured in CD3+ cells. The results of three independent experiments are shown as arithmetic mean ± 1 SD. (○), BSA; (•), ICAM-1; (□), BSA + IL-15; (▪), ICAM-1 + IL-15.
Induction of CD69 expression by T-cell interaction with immobilized ICAM-1. (A) PBLs were added to wells precoated with BSA (1%), rsICAM-1 (20 μg/mL), rsVCAM-1 (20 μg/mL), FN (20 μg/mL), and PLL (40 μg/mL). After 18 hours of incubation at 37°C, CD69 expression was measured in CD3+ cells by two-color flow cytometry. The results of three independent experiments are depicted as arithmetic mean ± 1 SD. *, P < .01 compared with BSA (Mann-Whitney U test). (B) ICAM-1 dose-dependent T-cell activation. PBLs were incubated on wells precoated with different concentrations of rsICAM-1 (▪) or rsVCAM-1 (•). After 18 hours, CD69 expression was analyzed in CD3+ cells. The results of four independent experiments are represented as arithmetic mean ± 1 SD. (C) Kinetics analysis of CD69 T-cell expression induced by rsICAM-1 and IL-15. PBLs were incubated on BSA (1%) or rsICAM-1 (20 μg/mL) precoated wells, and then IL-15 (5 ng/mL) was added where indicated. After 4, 16, 24, 40, 62, and 120 hours, cells were collected and CD69 expression was measured in CD3+ cells. The results of three independent experiments are shown as arithmetic mean ± 1 SD. (○), BSA; (•), ICAM-1; (□), BSA + IL-15; (▪), ICAM-1 + IL-15.
T-cell activation by adhesion molecules and IL-15.
It has been described that IL-15 is a T-cell stimulatory cytokine with chemotactic properties that plays a relevant role in chronic inflammatory processes.17 Chemotactic cytokines seem to act in concert with adhesion molecules to direct extravasation to sites of inflammation.33 We therefore analyzed the effect of IL-15, either alone or in combination with EC or ICAM-1, on the induction of CD69 expression in T cells. We found that this cytokine was able to upregulate the expression of CD69 on T cells in a dose- and time-dependent manner (Figs 2C and 3A), similar to what occurred with the interaction of PBTLs with immobilized ICAM-1. Unlike the former activation, IL-15 was also able to upregulate the expression of CD25. As expected, the effect of IL-15 on PBTLs was prevented by a blocking anti–IL-15 MoAb (Fig 3A). Because it has been reported that IFN-γ and TNF-α stimulate IL-15 production by EC and this IL-15 can be cell-surface associated,11 we studied the contribution of endothelial IL-15 to the induction of CD69 expression. The blocking anti–IL-15 MoAb produced a slight but consistent inhibition in the induction of CD69 by nonfixed TNF-α–activated EC, but no significant inhibitory effect on the activation promoted by fixed TNF-α–activated EC (Fig 3B).
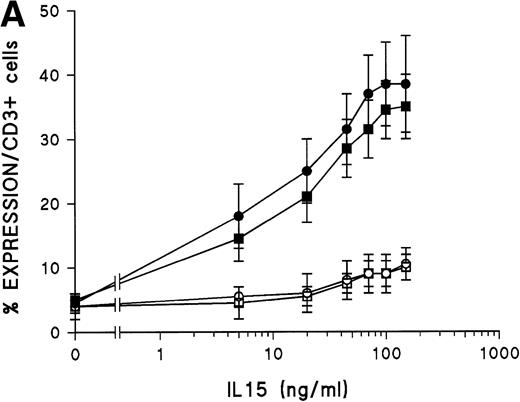
Effect of IL-15 in the activation of PBTLs. (A) Dose-dependent effect of IL-15 on the expression of CD25 (▪) and CD69 (•) by PBTLs. PBLs were incubated with IL-15 (5, 20, 45, 70, 100, or 150 ng/mL) by 18 hours in the absence (closed symbols) or presence (open symbols) of a blocking anti–IL-15 MoAb (5 μg/mL). Then, the expression of CD25 and CD69 was analyzed in CD3+ cells by two-color flow cytometry. The results of three independent experiments are shown as arithmetic mean ± 1 SD. (B) Contribution of endothelial IL-15 to the induction of CD69 in T cells. PBLs were cocultured with nonfixed (left) or fixed (right) TNF-–activated endothelium for 18 hours in the presence or absence of a blocking anti–IL-15 MoAb (5 μg/mL) and/or a blocking anti-CD18 MoAb. Then, the expression of CD69 was analyzed in CD3+ cells by two-color flow cytometry. The results of three independent experiments are shown as arithmetic mean ± 1 SD. *, P < .05 compared with untreated (Mann-Whitney U test).
Effect of IL-15 in the activation of PBTLs. (A) Dose-dependent effect of IL-15 on the expression of CD25 (▪) and CD69 (•) by PBTLs. PBLs were incubated with IL-15 (5, 20, 45, 70, 100, or 150 ng/mL) by 18 hours in the absence (closed symbols) or presence (open symbols) of a blocking anti–IL-15 MoAb (5 μg/mL). Then, the expression of CD25 and CD69 was analyzed in CD3+ cells by two-color flow cytometry. The results of three independent experiments are shown as arithmetic mean ± 1 SD. (B) Contribution of endothelial IL-15 to the induction of CD69 in T cells. PBLs were cocultured with nonfixed (left) or fixed (right) TNF-–activated endothelium for 18 hours in the presence or absence of a blocking anti–IL-15 MoAb (5 μg/mL) and/or a blocking anti-CD18 MoAb. Then, the expression of CD69 was analyzed in CD3+ cells by two-color flow cytometry. The results of three independent experiments are shown as arithmetic mean ± 1 SD. *, P < .05 compared with untreated (Mann-Whitney U test).
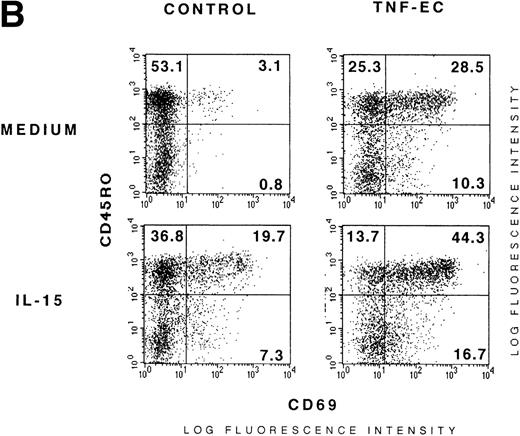
IL-15 and EC had an apparent additive effect on the induction of CD69, but not CD25 (Table 3 and Fig4A). This cooperative induction was preferentially exerted on the CD45RO+ subset of T cells (Fig 4B). This cytokine also collaborated with immobilized ICAM-1 to induce CD69 in T cells (Fig4C). The expression of CD69 obtained by the cooperative effect of EC and IL-15 was reverted to the levels induced by IL-15 alone by anti-CD18 MoAb, weakly affected by anti-CD49d MoAb, and not inhibited by the anti–VCAM-1 and anti–MHC class I MoAbs (Table 3).
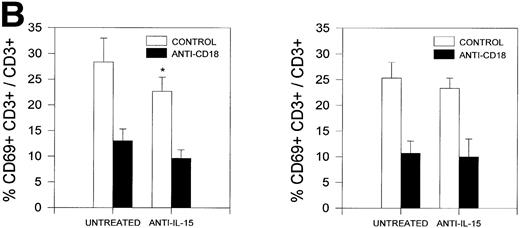
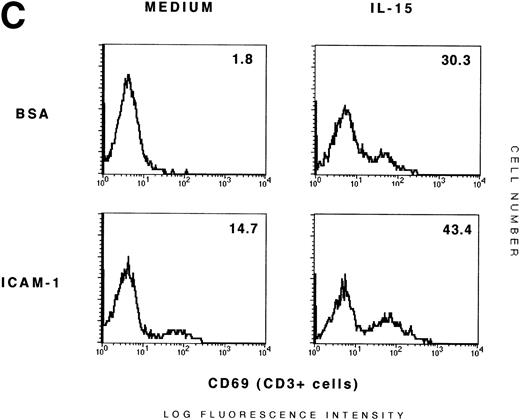
IL-15 cooperates with TNF-–activated ECs and ICAM-1 in the induction of CD69 T-cell expression. (A) Activated ECs do not enhance the induction of CD25 promoted by IL-15 in T cells. PBLs incubated in the presence or absence of fixed TNF-–activated ECs (TNF-EC and control, respectively) were stimulated for 18 hours in the presence or absence of IL-15 (15 ng/mL). Cells were collected and CD69/CD25 expression of CD3+ cells was analyzed by three-color flow cytometry. Numbers correspond to the percent of positive cells. A representative experiment out of three is shown. (B) Additive effect of IL-15 and activated ECs on the induction of CD69 in CD45RO memory T cells. PBLs were incubated alone (control) or on fixed TNF-–activated EC monolayers in the presence or absence of IL-15. After 18 hours of culture, CD69/CD45RO expression of CD3+cells was analyzed by three-color flow cytometry. Numbers correspond to the percent of positive cells. A representative experiment out of three is shown. (C) Additive effect of IL-15 and ICAM-1 on the induction of expression of CD69 by T cells. PBLs were plated on BSA (1%) or ICAM-1 (20 μg/mL) precoated wells in the presence or absence of IL-15 (25 ng/mL). After 18 hours, cells were collected and CD69 expression in CD3+ T cells was measured and is shown as percentage of positive T cells. A representative experiment out of five is shown.
IL-15 cooperates with TNF-–activated ECs and ICAM-1 in the induction of CD69 T-cell expression. (A) Activated ECs do not enhance the induction of CD25 promoted by IL-15 in T cells. PBLs incubated in the presence or absence of fixed TNF-–activated ECs (TNF-EC and control, respectively) were stimulated for 18 hours in the presence or absence of IL-15 (15 ng/mL). Cells were collected and CD69/CD25 expression of CD3+ cells was analyzed by three-color flow cytometry. Numbers correspond to the percent of positive cells. A representative experiment out of three is shown. (B) Additive effect of IL-15 and activated ECs on the induction of CD69 in CD45RO memory T cells. PBLs were incubated alone (control) or on fixed TNF-–activated EC monolayers in the presence or absence of IL-15. After 18 hours of culture, CD69/CD45RO expression of CD3+cells was analyzed by three-color flow cytometry. Numbers correspond to the percent of positive cells. A representative experiment out of three is shown. (C) Additive effect of IL-15 and ICAM-1 on the induction of expression of CD69 by T cells. PBLs were plated on BSA (1%) or ICAM-1 (20 μg/mL) precoated wells in the presence or absence of IL-15 (25 ng/mL). After 18 hours, cells were collected and CD69 expression in CD3+ T cells was measured and is shown as percentage of positive T cells. A representative experiment out of five is shown.
Induction of T-cell cytokine production by activated endothelium and IL-15.
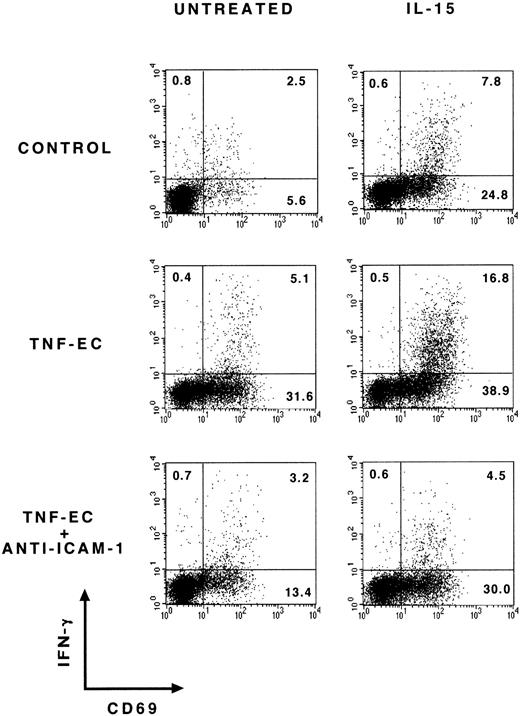
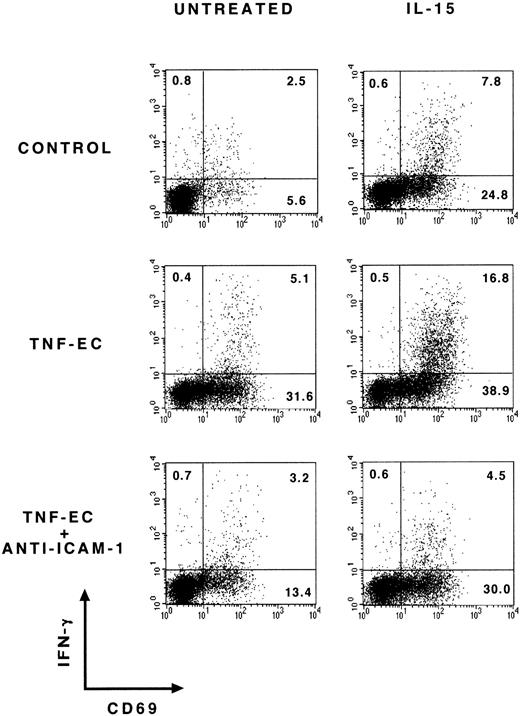
The effect of the interaction between fixed TNF-α–activated endothelium and T cells was also studied by intracellular detection of cytokines with specific MoAbs. As shown in Table 4, neither TNF-α–activated EC nor IL-15 were able to induce the production of IL-2 or IL-4. IL-15 alone induced a mild TNF-α production and a higher synthesis of IFN-γ in T cells. The interaction of T cells with activated EC increased the levels of IFN-γ predominantly in the CD69+ subset of T cells and this effect was additive with that of IL-15 (Table 4 and Fig 5). In addition, a blocking anti-ICAM-1 MoAb was able to inhibit the induction of IFN-γ production by activated EC, further indicating the involvement of the LFA-1/ICAM-1 pathway in the functional activation of these cells (Table 4 and Fig5). Cell cycle analysis in T cells after different periods of incubation with activated EC did not show any increment of cells in M or G2 phases, which is in accordance with the failure to induce T-cell production of IL-2 and IL-4 cytokines (data not shown, and Table4). Hence, the unusual activation state reached by these cells during the interaction with endothelium is not accompanied by cell proliferation.
Production of IFN-γ by T cells in the presence of TNF-–activated ECs and IL-15. PBLs were cultured alone (BSA) or on TNF-–activated ECs (TNF-EC) in the presence or absence of IL-15 (25 ng/mL) and/or anti–ICAM-1. After 48 hours of culture the expression of CD69 and intracellular IFN-γ was measured in T cells. A representative experiment out of four is shown.
Production of IFN-γ by T cells in the presence of TNF-–activated ECs and IL-15. PBLs were cultured alone (BSA) or on TNF-–activated ECs (TNF-EC) in the presence or absence of IL-15 (25 ng/mL) and/or anti–ICAM-1. After 48 hours of culture the expression of CD69 and intracellular IFN-γ was measured in T cells. A representative experiment out of four is shown.
Induction of T-cell activation during transmigration.
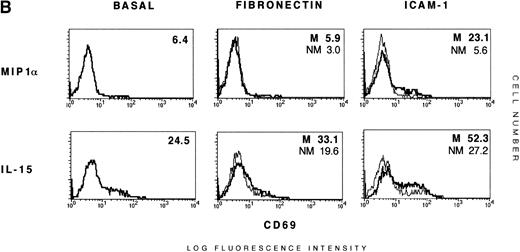
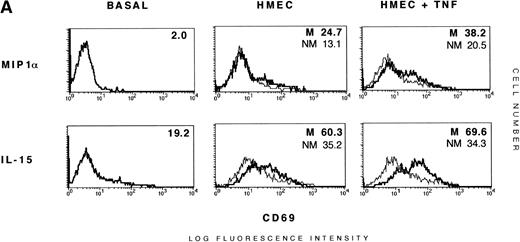
We then studied the effect of T-cell transmigration through HMEC-1 microvascular ECs on the induction of the expression of activation antigens by PBTLs. In static assays, T cells were induced to express CD69 by their interaction with the microvascular ECs: 17.6% ± 4.8% and 27.5% ± 7.3% by nonactivated and TNF-α–activated HMEC-1, respectively. In transmigration assays using IL-15 and MIP-1α as chemotactic agents,10,11 34 the migrated T lymphocytes showed a significantly higher expression of CD69 compared with nonmigrated T cells (Fig 6A). As expected, the transmigration through TNF-α–stimulated HMEC-1 induced the highest expression of CD69. In these assays, the activatory effect of IL-15 on PBTLs was also additive with that of HMEC-1 cells (Fig 6A, and data not shown). In contrast, MIP-1α did not increase the level of CD69 expression by itself and did not show any cooperative effect with HMEC-1 monolayers (Fig 6A, and data not shown).
Induction of T-cell activation during transmigration. (A) Additive effect of transendothelial migration and IL-15 on the expression of CD69 by T cells. PBTLs (>97% CD3+) were added to the upper compartment of Transwell chemotaxis chambers precoated with resting (HMEC-1) or TNF-–activated HMEC-1 cells (TNF–HMEC-1). In the lower chamber MIP1 (20 ng/mL) or IL-15 (15 ng/mL) were added as chemoattractants. As control, T cells were incubated with these cytokines in the absence of ECs. After 16 hours, control, upper chamber, and lower chamber T cells were separately collected and the expression of CD69 in CD3+ cells was measured by two-color flow cytometry. The thin lines and percentages correspond to the upper chamber T cells (NM, nonmigrated) and the thick lines and percentages to T cells migrated to the lower chamber (M, migrated).The proportion of migrated T cells for MIP1 is 25.1% (HMEC-1) and 30.6% (TNF–HMEC-1), and for IL-15 is 33.8% (HMEC-1) and 37.3% (TNF–HMEC-1). A representative experiment out of three is shown. (B) Additive effect of transmigration across ICAM-1–coated membranes and IL-15 on T-cell activation. PBTLs were plated in the upper compartment of FN (20 μg/mL) or rsICAM-1 (20 μg/mL) precoated Transwell chemotaxis chambers and MIP1 (20 ng/mL) or IL-15 (15 ng/mL) were added as chemoattractants in the lower chamber. Control cells were incubated as in (A). After 16 hours, T cells from both chambers were collected separately and the expression of CD69 in CD3+ cells was measured. The thin lines and percentages correspond to nonmigrated (NM) T cells from the upper chamber and the thick lines and percentages are referred to migrated (M) cells from the lower chamber. The proportion of migrated cells for MIP1 is 32.4% (FN) and 37.1% (ICAM-1), and for IL-15 is 42.8% (FN) and 47.6% (ICAM-1). A representative experiment out of three is shown.
Induction of T-cell activation during transmigration. (A) Additive effect of transendothelial migration and IL-15 on the expression of CD69 by T cells. PBTLs (>97% CD3+) were added to the upper compartment of Transwell chemotaxis chambers precoated with resting (HMEC-1) or TNF-–activated HMEC-1 cells (TNF–HMEC-1). In the lower chamber MIP1 (20 ng/mL) or IL-15 (15 ng/mL) were added as chemoattractants. As control, T cells were incubated with these cytokines in the absence of ECs. After 16 hours, control, upper chamber, and lower chamber T cells were separately collected and the expression of CD69 in CD3+ cells was measured by two-color flow cytometry. The thin lines and percentages correspond to the upper chamber T cells (NM, nonmigrated) and the thick lines and percentages to T cells migrated to the lower chamber (M, migrated).The proportion of migrated T cells for MIP1 is 25.1% (HMEC-1) and 30.6% (TNF–HMEC-1), and for IL-15 is 33.8% (HMEC-1) and 37.3% (TNF–HMEC-1). A representative experiment out of three is shown. (B) Additive effect of transmigration across ICAM-1–coated membranes and IL-15 on T-cell activation. PBTLs were plated in the upper compartment of FN (20 μg/mL) or rsICAM-1 (20 μg/mL) precoated Transwell chemotaxis chambers and MIP1 (20 ng/mL) or IL-15 (15 ng/mL) were added as chemoattractants in the lower chamber. Control cells were incubated as in (A). After 16 hours, T cells from both chambers were collected separately and the expression of CD69 in CD3+ cells was measured. The thin lines and percentages correspond to nonmigrated (NM) T cells from the upper chamber and the thick lines and percentages are referred to migrated (M) cells from the lower chamber. The proportion of migrated cells for MIP1 is 32.4% (FN) and 37.1% (ICAM-1), and for IL-15 is 42.8% (FN) and 47.6% (ICAM-1). A representative experiment out of three is shown.
To further examine the role of ICAM-1 in the activation of purified PBTLs, we performed transmigration assays in chemotaxis Transwell chambers coating the polycarbonate membrane (3-μm diameter pore size) with either ICAM-1 or FN. ICAM-1 exerted its proactivatory effect on T cells that migrated in response to IL-15 or MIP-1α (Fig 6B). As in other assays, IL-15 cooperated with the activation induced by the transmigration across ICAM-1 and the migrated subpopulation showed the highest level of CD69 expression (Fig 6B). FN did not show any proactivatory effect (data not shown); however, differences in CD69 expression between the migrated and nonmigrated cells were observed when the chemotaxis was induced by IL-15, likely because of a higher migratory capacity of IL-15–activated T cells (Fig 6B). As it was found in other experiments, the phenotype of the cells activated in the transmigration assays mainly corresponded to CD8+ and CD45RO+ cells (data not shown).
DISCUSSION
The activation of T cells in vivo is usually induced through the TCR/CD3 complex by immunogenic peptides bound to MHC molecules. However, different evidences indicate that most T cells that are recruited and activated at sites of chronic inflammation do not respond to the triggering antigens.2,35 Little is known about the mechanisms involved in the nonspecific recruitment and activation of these cells. Different cytokines are able to activate T cells in vitro in an antigen-independent manner. However, the doses and combinations of cytokines used in such studies do not fully explain the pattern of T-cell activation at sites of chronic inflammation.8,36 In addition, at these sites (eg, RA synovium), there is a relative absence of T-cell–derived cytokines,37 and proactivatory cytokines, such as IL-15, are detected at a lower concentration than that required for the activation of T lymphocytes.8 17Therefore, it is important to explore the possible alternative mechanisms of T-cell activation and recruitment that occur at sites of chronic inflammation.
It has previously been proposed that preactivated cells preferentially migrate toward sites of chronic inflammation. In this regard, it has been described, by using short-time transendothelial migration assays, that the migrated population is slightly enriched in CD69+cells.21,22,38 Herein, we have explored the possible involvement of activated endothelium in the activation and recruitment of resting lymphocytes as an alternative mechanism that accounts for the abundance of activated bystander T cells in chronic inflammatory cell infiltrates. A previous report described that a long-time coculture of peripheral blood mononuclear cells with IL-1β–stimulated ECs resulted in the induction of CD69 in T cells.23 We have observed in a similar model using PBLs cultured in the presence of both resting and TNF-α–stimulated ECs that this proactivatory effect is independent of the presence of monocytes, thus ruling out the possibility of an indirect activation of T cells by monocyte-derived cytokines. In addition, we report the key role of the LFA-1/ICAM-1 adhesion pathway and the additive effect of IL-15 on the activation of PBTLs during this interaction. The interaction with activated ECs through the LFA-1/ICAM-1 pathway is able to induce the production of IFN-γ on CD69+ T cells, which is additive to the response induced by IL-15. In contrast, ECs were unable to stimulate the secretion of IL-4, IL-2, or TNF-α. T cells did not proliferate in response to activated ECs in agreement with the absence of IL-2 and the low expression of CD25. Although we did not perform coculture experiments using autologous T cells and ECs, the possibility of an allogeneic stimulatory effect can be ruled out both by the lack of induction of CD25 expression and by the absence of effect of the blocking anti-MHC MoAb on CD69 upregulation.
The involvement of cell adhesion molecules in the activation of PBTLs induced by their interaction with ECs was initially suggested by (1) the failure of EC culture supernatants to activate T cells; (2) the ability of fixed ECs to reproduce the activation effect on PBTLs observed with alive cells; and (3) resting ECs, which express low levels of ICAM-1, only slightly induced CD69 expression on T cells, whereas activated ECs, which strongly upregulate ICAM-1 and VCAM-1, induced a much higher expression of CD69. Our data showing both the inhibition of CD69 expression with anti–LFA-1/ICAM-1 MoAb as well as the induction of CD69 on interaction of PBTLs with immobilized ICAM-1 underscore the importance of the LFA-1/ICAM-1 adhesion pathway in T-cell activation by ECs. The activation of PBTLs by ECs was preferentially exerted on the CD45RO+ T-cell subset. This is in accordance with the fact that these memory T cells express a higher density of LFA-1 than naive T cells, preferentially bind to endothelium, and show an intrinsic migratory capacity, thus leading to their accumulation in chronic inflammatory infiltrates.38-40 The persistence of CD69 T-cell expression observed on the interaction of PBTLs with ICAM-1 is clearly distinct to that described after stimulation with anti-CD3 MoAbs or phorbol esters, which induce a transient increment in CD69 and CD25 expression and a return to basal levels after 48 hours.24
The relevant role played by the cytokine IL-15 in chronic inflammatory lesions has been reported.9,16 The IL-15 produced in the rheumatoid synovium can recruit and activate T cells, which in turn amplify and perpetuate the inflammatory phenomenon through the induction of monocyte-derived TNF-α via a cell-to-cell contact-dependent mechanism. Both CD69 and LFA-1 have been postulated as the cell surface molecules that mediate the interaction of T cells with monocytes, leading to the secretion of TNF-α and the subsequent induction of a cascade of proinflammatory cytokines that are responsible for joint destruction.17 Nevertheless, at least in the case of RA, the induction of CD69 expression is not completely explained by the action of IL-15 alone, because the levels of IL-15 detected in RA synovial fluid are lower than those required to trigger a high expression of CD69.8,17 Our data show that IL-15 is able to induce in vitro the expression of CD69 and CD25 on T cells. Therefore, the phenotype induced by IL-15 does not completely correspond with that observed in chronic inflammatory infiltrates, where T cells display a high expression of CD69 with only intermediate levels of CD25.1,18,19,41 However, this phenotype corresponds to that induced by the coordinate effect of activated endothelium plus IL-15, with a high expression of CD69 and a mild induction of CD25. The recently reported activation of the binding capacity of LFA-1 to ICAM-1 by IL-15 could explain this cooperative effect of IL-15 in EC-induced T-cell activation.11
In the transendothelial migration process, T cells interact with EC mainly via the LFA-1/ICAM-1 adhesion pathway.3 Our studies on the phenotypic characterization of T cells that transmigrate across confluent monolayers of the human microvascular EC line HMEC-1 showed the highest expression of CD69 in T cells that were able to transmigrate. This induction of CD69 expression was much higher when T cells transmigrated across TNF-α–activated HMEC-1 than through nonactivated HMEC-1. Furthermore, by using an ICAM-1–coated Transwell migration system, we could reproduce the high induction of CD69 in the migratory subpopulation and this proactivatory effect was additive with IL-15. All these results suggest that the induction of CD69, but not CD25, during transmigration is mediated by the LFA-1/ICAM-1 interaction, as occurs during interaction with EC monolayers. On the other hand, the higher CD69 expression found in the migratory subpopulation of T cells in the FN-coated Transwell chambers when IL-15 is used as chemoattractant is likely because of the higher migratory capacity of the IL-15–activated T cells.
In summary, our data suggest that the activated endothelium at sites of chronic inflammation, along with IL-15, is able to induce, via the LFA-1/ICAM-1 adhesion pathway, the activation and recruitment of PBTLs, preferentially the CD8+ CD45RO+ cell subset. This phenomenon could be responsible for the phenotype (CD69high, CD25dull) and the pattern of cytokines (Th1 response, absence of IL-2, and proliferation) observed in chronic inflammatory T-cell infiltrates. The relevance of LFA-1 in these conditions could be further emphasized by the existence of an LFA-1–activating environment that has been found in the rheumatoid synovial fluid.42 Therefore, the maintenance of T-cell activation in chronic inflammatory sites could result from the interaction of these LFA-1 high-avidity state T cells with resident cells expressing ICAM-1.43 44 In addition, cytokines might potentiate this T-cell activation. This model provides a mechanism for the recruitment and activation of CD45RO+ T cells at sites of chronic inflammation, where there is a relative absence of T-cell–derived cytokines, such as IL-2.
ACKNOWLEDGMENT
We are especially grateful to Drs R. González-Amaro, M. Nieto, and M.A. del Pozo for critical reading of the manuscript; to E. Moreno for excellent editorial assistance; and to M.Vitón for technical support.
Supported by grant SAF96/0039 from Plan Nacional de Investigación y Desarrollo and by Grant No. 08.3/0011/1997 from Comunidad Autónoma de Madrid.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Francisco Sánchez-Madrid, Servicio de Inmunologı́a, Hospital de la Princesa, Universidad Autónoma de Madrid, Diego de León, 62, 28006-Madrid, Spain; e-mail: fsmadrid/princesa@hup.es).