Abstract
Vascular endothelium is continuously exposed to complement-mediated challenge, and this is enhanced during inflammation. Although the complement-regulatory proteins decay-accelerating factor (DAF), CD59, and membrane cofactor protein (MCP) protect endothelial cells (ECs) against complement-mediated injury, the control of their expression and relative contributions to vascular protection is unclear. We explored the hypothesis that mechanisms exist which induce upregulation of complement-regulatory proteins on ECs to maintain vascular function in inflammation. Tumor necrosis factor alpha (TNF) and interferon gamma (IFNγ) each increased DAF expression but not CD59 or MCP expression, and a combination of these cytokines was more potent than either alone. Cytokine-induced expression depended on increased DAF mRNA and de novo protein synthesis and was maximal by 72 hours. In addition, assembly of the membrane-attack complex (MAC) on ECs induced a 3-fold increase in DAF expression, and this was enhanced by cytokines. DAF upregulation was not inhibited by protein kinase C (PKC) antagonists. The increase in DAF was functionally relevant since it reduced complement 3 (C3) deposition by 40%, and this was inhibited by an anti-DAF monoclonal antibody. These observations indicate that upregulation of DAF expression by cytokines or MAC may represent an important feedback mechanism to maintain the integrity of the microvasculature during subacute and chronic inflammatory processes involving complement activation.
COMPLEMENT is a powerful cytotoxic defense system which, by the nature of its effects, represents a potential danger to host cells.1 As a consequence of this, a complex array of protective mechanisms have evolved, including the cell-surface proteins decay-accelerating factor ([DAF] CD55), protectin (CD59), and membrane cofactor protein ([MCP] CD46). The genes encoding DAF and MCP are closely related and clustered on the long arm of chromosome 1, band 1q32, while the gene for CD59 is located on chromosome 11.2 The mechanisms by which these factors regulate complement are distinct. DAF, which prevents the formation and accelerates the decay of complement 3 (C3) convertases,3and MCP, which binds C3b and C4b and facilitates their degradation by factor I,4 operate at the proximal end of the cascade, while CD59 serves to inhibit the membrane-attack complex ([MAC] C5b-9).5
Vascular endothelium, by virtue of its anatomic location at the blood/tissue interface, may be directly exposed to autologous complement activation, particularly during inflammation.1In certain instances such as severe vasculitis and, most notably, antibody-mediated hyperacute allograft rejection, this is overwhelming and results in endothelial cell (EC) death.6 However, in a variety of chronic inflammatory diseases such as atherosclerosis and rheumatoid arthritis and systemic inflammatory states such as systemic lupus erythematosus, endothelium is continuously exposed to low levels of complement activation with deposition of the C5b-9 MAC but without significant EC lysis.7-9 Although DAF, CD59, and MCP are all expressed on ECs and contribute to the control of complement activation on the cell surface,10-12 the specific contributions of these different molecules to the protection of the endothelium during inflammation remain to be determined.2
Exposure of ECs to proinflammatory cytokines results in marked phenotypic changes including upregulation of adhesion molecules, secretion of soluble mediators, and changes in vascular tone and permeability.13,14 In addition, it is well established that complement-activation products generated during an inflammatory response may act directly on ECs and influence their function.15 Thus, C1q may upregulate the expression of E-selectin and intercellular adhesion molecule-1 (ICAM-1),16 while C5a has been shown to induce P-selectin expression by ECs.17 Furthermore, it has been reported that sublytic concentrations of C5b-9 can bind to ECs, stimulating the expression of adhesion molecules and the release of biologically active mediators. Thus, assembly of the MAC on the EC surface may upregulate the expression of tissue factor,18,19 as well as P- and E-selectin, vascular cell adhesion molecule-1 (VCAM-1), and ICAM-1.19-21 In addition, the secretion by ECs of an array of soluble mediators in response to C5b-9, including the chemokines interleukin-8 (IL-8) and monocyte-chemoattractant protein-1,22 prostacyclin,23 von Willebrand factor,20 and the growth factors basic fibroblast growth factor and platelet-derived growth factor,24 has been reported.
We aimed to investigate the hypothesis that the maintenance of vascular integrity in the face of persistent complement activation during chronic inflammation is dependent on the induction of one or more of the complement-regulatory proteins DAF, CD59, and MCP by proinflammatory mediators. Thus, soluble and cell-associated mediators of the inflammatory response might act to upregulate the innate protective mechanisms of endothelium against the potentially deleterious effects of complement activation, in parallel with their ability to facilitate leukocyte adhesion and transmigration. Although there is some evidence that DAF, MCP, and CD59 can be upregulated on the EC surface in vitro, the mechanisms of control remain poorly understood. The expression of DAF on human umbilical vein ECs (HUVECs) may be upregulated by phorbol esters,25 wheat germ agglutinin,26 and histamine.27 Despite this, there are few data on the regulation of complement-regulatory proteins by cytokines on ECs, with the exception of one report showing a modest increase in DAF expression by HUVECs in response to stimulation with IL-4 or IL-1.28 To our knowledge, there is no published information on the regulation of the expression of complement-regulatory proteins by microvascular ECs, which may be particularly vulnerable to complement activation during inflammatory responses that develop in the tissues in vivo. In this study, we characterized the expression and regulation of DAF, MCP, and CD59 on cultured human large- and small-vessel ECs. We provide evidence that DAF is inducible on the EC surface, by both protein kinase C (PKC)-dependent and -independent pathways, in response to soluble and cell-associated proinflammatory mediators, and demonstrate a functional role for this response in the protection of EC viability.
MATERIALS AND METHODS
Monoclonal antibodies and other reagents.
The monoclonal antibodies (MoAbs) included the following. A35 (IgG1) against CD59 and anti-DAF MoAbs 5B2 and 1C6 (both IgG1); the latter were kind gifts from Dr T. Fujita (University of Tsukuba, Tsukuba, Japan). Anti-DAF MoAb 1H4 (IgG1) and TRA-2-10 (IgG1) against MCP were kind gifts from Dr D.M. Lublin and Professor J.P. Atkinson, respectively (Washington University School of Medicine, St Louis, MO). The anti-endoglin (CD105) mAb RMAC8 (IgG2a) and the anti–class I MoAb W6/32 (IgG2a) were kind gifts from Dr A. d’Apice (St Vincent’s Hospital, Victoria, Australia) and Dr N. Davey (Imperial College School of Medicine, London, UK), respectively. IgG1 and IgG2a control MoAbs were obtained from the adhesion panel of the Fifth CD Workshop, and the EC-specific mAb EN4 (IgG1) was from Sanbio (Uden, Holland). Recombinant human tumor necrosis factor-α (TNF-α) and the mAb MOPC-21, which was used as an isotype-matched negative control, were kind gifts from Dr Martyn Robinson (Celltech, Slough, UK). We are grateful for the gift of the following cytokines: recombinant human interferon gamma ([IFN-γ] Glaxo, Geneva, Switzerland), IL-4 (Immunex Corp, Seattle, WA), and IL-1β (Glaxo, Geneva, Switzerland). The specific PKC antagonist RO31-822029 was a kind gift from Dr Trevor Hallam (Roche, Welwyn Garden City, UK). The PKC agonist phorbol 12, 13-dibutyrate (PBu), bovine serum albumin (BSA), nonenzymatic cell-dissociation solution, and cycloheximide were purchased from Sigma Chemical Co (Poole, UK). Normal human serum (NHS) was obtained from blood samples from healthy individuals, collected under sterile conditions into glass tubes and allowed to clot at 37°C prior to further incubation at 4°C for 2 hours to induce clot retraction. Following centrifugation at 1,800g, the NHS was collected, pooled, and stored at −70°C.
Cell isolation and culture.
HUVECs were isolated from umbilical cords by digestion with collagenase type II (Boehringer Mannheim, Lewes, UK) as described previously,30 and cultured in 1% gelatin–coated tissue culture flasks (Costar, Cambridge, MA) in medium 199 ([M199] ICN Biomedicals Inc, Costa Mesa, CA) supplemented with 20% fetal bovine serum ([FBS] Hyclone Laboratories Inc, Logan, UT), 100 IU/mL penicillin, 0.1 mg/mL streptomycin, 2 mmol/L l-glutamine (all from GIBCO-BRL Life Technologies, Paisley, UK), 10 U/mL heparin (Leo Laboratories, Prince Risborough, UK), and 30 μg/mL EC growth supplement (Sigma). Dermal microvascular ECs (DMECs) were isolated from human foreskins and cultured in fibronectin-coated flasks as previously described in detail.31 Each experiment was performed with ECs at passage 3 to 6. The human dermal microvascular cell line HMEC-1,32 a kind gift from Dr E. Ades (Centers for Disease Control, Atlanta, GA), was cultured in 1% gelatin–coated tissue culture flasks in MCDB-131 growth medium (GIBCO-BRL) supplemented with 10% FBS, 100 IU/mL penicillin, 0.1 mg/mL streptomycin, 2 mol/Ll-glutamine, and 10 ng/mL epidermal growth factor (Becton Dickinson, Bedford, MA).
Treatment of cells with phosphatidylinositol-specific phospholipase C.
Phosphatidylinositol-specific phospholipase C (PIPLC) was prepared fromBacillus cereus by Dr Peter Robinson (Imperial College School of Medicine, London, UK). To cleave the glycosyl-phosphatidylinositol (GPI)-anchored proteins DAF and CD59 from the cell surface, monolayers of ECs in 35-mm petri dishes (6 × 105 cells per dish) were washed three times with Hanks’ balanced salt solution (HBSS) before addition of PIPLC diluted 1:100 in M199. After incubation at 37°C for 30 minutes, ECs were washed with HBSS, harvested with trypsin/EDTA (ICN Biomedicals), and analyzed by flow cytometry for surface antigen expression.
Flow cytometry.
Following stimulation with test factors, monolayers of ECs were harvested by exposure to trypsin/EDTA for 1 minute at 37°C. After repeated pipetting to ensure single-cell suspensions, the cells were stained with the appropriate primary MoAb for 30 minutes at 4°C. After washing twice in phosphate-buffered saline/2.5% FBS, ECs were resuspended in fluorescein isothiocyanate (FITC)-labeled rabbit anti–mouse Ig (DAKO, Glostrup, Denmark) for 30 minutes at 4°C, followed by washing as before and fixation in 1% paraformaldehyde. Samples were analyzed on an Epics XL-MCL flow cytometer (Coulter, Hialeah, FL) by counting 10,000 cells per sample. In some experiments, results are expressed as the relative fluorescence intensity (RFI), which represents the mean fluorescence intensity (MFI) with test MoAb divided by the MFI using an isotype-matched irrelevant MoAb. In the inhibition experiments, RO31-8220 and cycloheximide led to a small reduction in the constitutive expression of DAF by resting ECs. To control for this effect, the results of these experiments are expressed as the RFI ratio, calculated as follows: RFI ratio = DAF RFI on EC Treated With Proinflammatory Stimulus/DAF RFI on Unstimulated EC Control.
Northern blotting analysis.
Confluent ECs in 75-cm2 tissue culture flasks were incubated with TNF-α (10 ng/mL) and IFN-γ (500 U/mL) or plain medium alone for a maximal 24 hours at 37°C. At the end of the stimulation, cells were lysed in guanidinium isothiocyanate (Sigma) and RNA was extracted as described by Chomczynski and Sacchi.33Purified RNA was resuspended in 20 μL RNase-free water and stored at −70°C before use. The probe for DAF was obtained from a plasmid vector34 and the DAF insert released by incubation for 2 hours at 37°C with the SalI and XbaI restriction enzymes. Northern blotting was performed as described by Sambrook et al.35 Purified RNA was run on 1% formaldehyde agarose gels, blotted onto GeneScreen membrane (DuPont, Letchworth, UK), and fixed in a UV Crosslinker (Stratagene, Cambridge, UK). Membranes were prehybridized for 4 hours in 1 mol/L NaCl with 50% (vol/vol) formamide, 4 mg DNA (salmon tests), 0.1% (wt/vol) sodium dodecyl sulfate (SDS), and 10% (wt/vol) dextran sulfate (all from Sigma). Approximately 200 ng purified probes were boiled for 3 minutes and used for radiolabeling with 32P-dCTP using the Klenow fragment of Escherichia coli DNA polymerase (Northumbria Biologicals, Cramlington, UK). Membranes were hybridized to appropriate32P-dCTP–labeled cDNA probes overnight at 42°C, and were then washed in solutions of 0.1% SDS (wt/vol) containing successively lower concentrations of SSC buffer (1× SSC is 0.15 mol/L NaCl plus 0.015 mol/L sodium citrate, pH 7). Specific hybridization was detected by autoradiography following exposure to Kodak XOMat film (Eastman Kodak, Rochester, NY). For quantification, Northern blots were scanned using the Appligene Image Analysis System (Appligene, Durham, UK), and densitometry was performed using National Institutes of Health Image 1.52 software (Bethesda, MD). Values were corrected for ethidium bromide–stained rRNA-loading patterns, and an arbitrary value of 1 was assigned to unstimulated ECs.
Generation of the MAC.
ECs were plated at confluence (2 × 105 cells per well) in 24-well plates (Costar) and cultured overnight at 37°C. They were then opsonized with MoAb RMAC8 (IgG2a), negative control MoAb, or plain medium alone for 1 hour prior to addition of 2.5% NHS, heat-inactivated human serum ([HIHS] 30 minutes at 56°C), or C7- or C8-deficient serum (Sigma) followed by incubation at 37°C for up to 48 hours. At the end of the assay, the EC monolayers were washed and the cells were harvested by trypsin/EDTA. After repeated pipetting to ensure single-cell suspensions, the cells were stained with an FITC-labeled anti-DAF MoAb (Serotec, Kidlington, Oxford, UK) for 30 minutes at 4°C, and DAF expression was then analyzed by flow cytometry as described before. The serum concentrations in the assay were defined as sublytic using a standard51Cr-release assay12 (data not shown). In addition, in all experiments, cell viability was assessed by examination of cell monolayers using phase-contrast microscopy, cell-counting, and estimation of trypan blue exclusion in the EC populations before staining.
C3-binding assay.
ECs were plated in 35-mm petri dishes (6 × 105 cells per dish) and cultured overnight at 37°C before addition of TNFα (10 ng/mL) and IFNγ (500 U/mL), or in plain medium alone for 48 hours. Following harvesting with trypsin/EDTA, ECs were pelleted in 96-well v-bottom plates (Costar) and incubated with RMAC8 MoAb for 30 minutes at 4°C. After washing with HBSS/1% BSA, ECs were incubated with 100 μL 20% NHS in M199 for 2 hours at 37°C prior to washing with HBSS/1% BSA and addition of FITC-conjugated rabbit anti–human C3c (DAKO) at 1:40 dilution for 30 minutes at 4°C. After washing twice with HBSS/1% BSA, the presence of C3c was estimated using flow-cytometric analysis as already described. Control samples included the omission of NHS and the addition of 10 mmol/L EDTA to the NHS to inhibit the classic pathway of complement activation. In the inhibition studies, the blocking MoAbs were added to the assay with the RMAC8 MoAb to achieve a final concentration of 50 μg/mL.
Statistics.
Differences between the results of experimental treatments were evaluated by the Mann-Whitney U test. Differences were considered significant at a P value of <.05.
RESULTS
Expression of DAF, MCP, and CD59 on ECs.
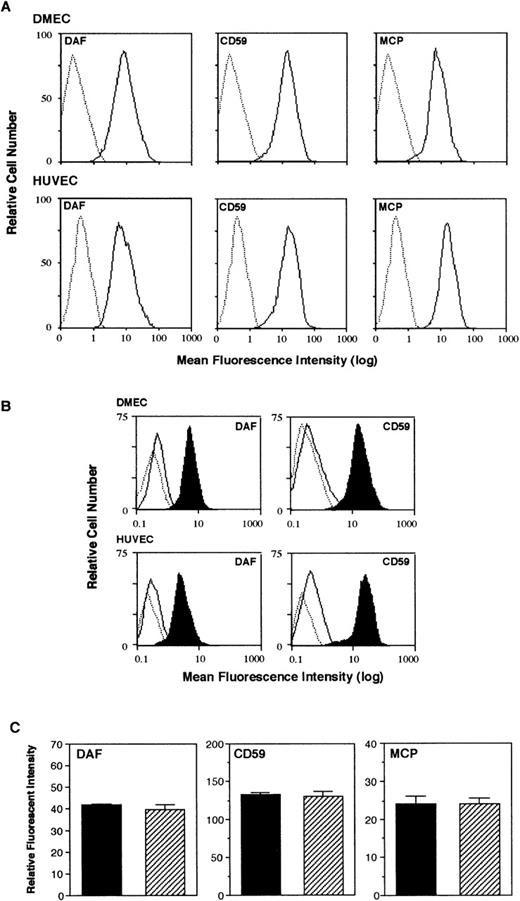
Flow-cytometric analysis of resting ECs demonstrated that DAF, MCP, and CD59 are constitutively expressed on the cell surface of both HUVECs and DMECs. All 3 molecules were found on greater than 95% of resting ECs with unimodal expression (Fig 1A). On large-vessel ECs, CD59 and DAF are known to be attached to the cell surface via a GPI anchor,2 which may influence the function of these molecules.3 To investigate the membrane-anchoring of DAF and CD59 on microvascular ECs, the expression of both molecules was compared before and after treatment of ECs with PIPLC. Incubation of ECs with PIPLC for 30 minutes at 37°C removed greater than 90% of DAF and CD59 from the surface of HUVECs and DMECs, demonstrating that these molecules are predominantly GPI-anchored on both cell types (Fig1B). In contrast, MCP, although constitutively expressed on both HUVECs and DMECs, was not released by PIPLC, consistent with attachment to the cell surface via a transmembrane anchor (data not shown).4The specificity of PIPLC for GPI-anchored proteins alone was further confirmed by its failure to alter the surface expression of CD31 and ICAM-1 (data not shown). To exclude a deleterious effect of trypsin on the levels of DAF, CD59, and MCP measured, HUVECs were harvested with either trypsin/EDTA or a nonenzymatic cell-dissociation solution (Sigma) and analyzed by flow cytometry. No difference in the expression of DAF, CD59, or MCP was observed following the different treatments (Fig 1C).
Expression of DAF, CD59, and MCP on HUVECs and DMECs. (A) Expression of DAF, CD59, and MCP on resting ECs was assessed by flow cytometry using mAbs 5B2, A35, and TRA-2-10, respectively. The figure shows expression on DMECs and HUVECs with background fluorescence (FITC-labeled rabbit anti–mouse Ab alone, …) and specific antigen expression (—). (B) EC monolayers were incubated for 30 minutes in the absence or presence of PIPLC before harvesting and analysis by flow cytometry. DAF and CD59 were detected with MoAb 5B2 and A35, respectively. The figure shows background fluorescence (…), untreated ECs demonstrating constitutive expression (shaded histogram), and PIPLC-treated ECs (—). (C) HUVECs were harvested with either trypsin/EDTA (▪) or a nonenzymatic cell-dissociation solution (▨) before analysis by flow cytometry. DAF, CD59, and MCP were detected with MoAbs 5B2, A35, and TRA-2-10, respectively. The figure is representative of 3 similar experiments.
Expression of DAF, CD59, and MCP on HUVECs and DMECs. (A) Expression of DAF, CD59, and MCP on resting ECs was assessed by flow cytometry using mAbs 5B2, A35, and TRA-2-10, respectively. The figure shows expression on DMECs and HUVECs with background fluorescence (FITC-labeled rabbit anti–mouse Ab alone, …) and specific antigen expression (—). (B) EC monolayers were incubated for 30 minutes in the absence or presence of PIPLC before harvesting and analysis by flow cytometry. DAF and CD59 were detected with MoAb 5B2 and A35, respectively. The figure shows background fluorescence (…), untreated ECs demonstrating constitutive expression (shaded histogram), and PIPLC-treated ECs (—). (C) HUVECs were harvested with either trypsin/EDTA (▪) or a nonenzymatic cell-dissociation solution (▨) before analysis by flow cytometry. DAF, CD59, and MCP were detected with MoAbs 5B2, A35, and TRA-2-10, respectively. The figure is representative of 3 similar experiments.
DAF is cytokine-inducible on ECs.
To investigate the regulation of complement-regulatory proteins on the EC surface during inflammation, monolayers of ECs were stimulated with the proinflammatory cytokines TNF-α, IL-1β, IFN-γ, or a combination of TNF-α and IFN-γ and subsequently analyzed by flow cytometry. The concentrations of cytokines were based on those previously demonstrated to induce EC activation and upregulation of surface molecules including E-selectin, VCAM-1, ICAM-1, and Thy-1,30,31 36 and dose-response curves for each cytokine tested were generated (data not shown). No significant increase in the expression of either CD59 (Fig 2C and D) or MCP (Fig 2E and F) was found following a 48-hour stimulation with these cytokines. Furthermore, an extended time course up to 72 hours showed similar results. However, a significant increase in DAF was found following stimulation for 48 hours with TNF-α (DMECs and HUVECs) and IFN-γ (DMECs) (P < .05; Fig 2A and B). Moreover, the combination of TNF-α and IFN-γ was more effective than either cytokine alone, inducing an increase in DAF expression of up to 4-fold (P < .02; Fig 2A and B). While we were able to consistently demonstrate a small increase in DAF expression on HUVECs after 72 hours of stimulation with IL-4, this did not reach significance. Furthermore, IL-4 had no effect on the expression of DAF on DMECs in 4 separate experiments on different EC preparations (data not shown). In addition, we were unable to demonstrate an effect of IL-4 on the TNF-induced expression of DAF or an effect of IL-4 on MCP or CD59.
Analysis of DAF, CD59, and MCP expression on DMECs and HUVECs following stimulation with cytokines. Monolayers of ECs were incubated for 48 hours in the presence or absence of IL-1β (10 ng/mL), IFNγ (500 U/mL), TNF- (10 ng/mL), or TNF- and IFN-γ before harvesting and analysis by flow cytometry. DAF, CD59, and MCP were detected using MoAbs 5B2, A35, and TRA-2-10, respectively. The results (mean ± SD) are expressed as the RFI (MFI of test sample divided by MFI of irrelevant isotype-matched negative control) for (A, B) DAF, (C, D) CD59, and (E, F) MCP. The results are representative of 4 experiments performed on different EC lines. *P < .05, **P < .02. The efficacy of cytokines used in each experiment was confirmed by their ability to induce VCAM-1 or ICAM-1 as appropriate (data not shown). US, unstimulated.
Analysis of DAF, CD59, and MCP expression on DMECs and HUVECs following stimulation with cytokines. Monolayers of ECs were incubated for 48 hours in the presence or absence of IL-1β (10 ng/mL), IFNγ (500 U/mL), TNF- (10 ng/mL), or TNF- and IFN-γ before harvesting and analysis by flow cytometry. DAF, CD59, and MCP were detected using MoAbs 5B2, A35, and TRA-2-10, respectively. The results (mean ± SD) are expressed as the RFI (MFI of test sample divided by MFI of irrelevant isotype-matched negative control) for (A, B) DAF, (C, D) CD59, and (E, F) MCP. The results are representative of 4 experiments performed on different EC lines. *P < .05, **P < .02. The efficacy of cytokines used in each experiment was confirmed by their ability to induce VCAM-1 or ICAM-1 as appropriate (data not shown). US, unstimulated.
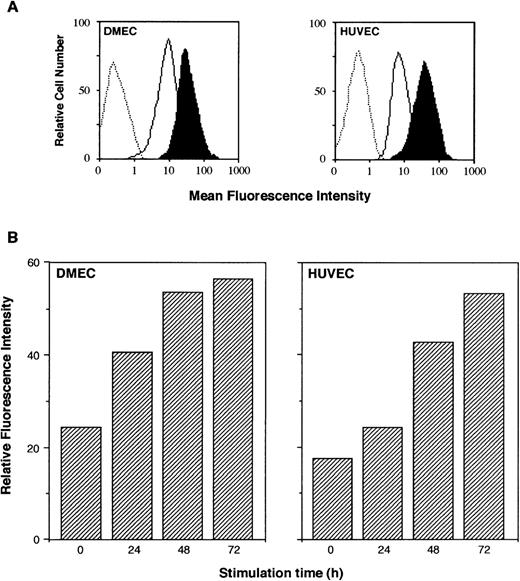
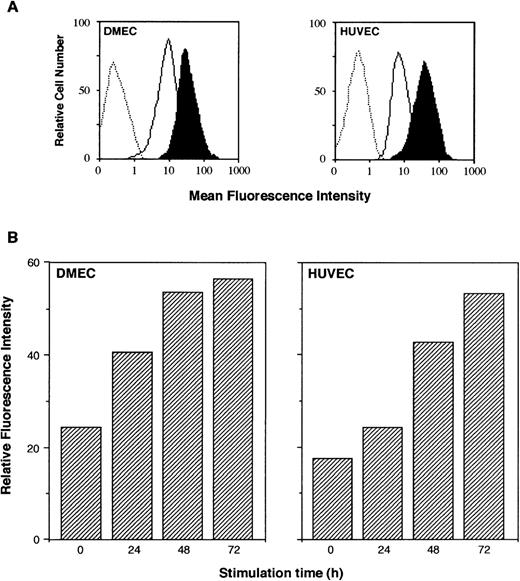
The flow-cytometric histograms of DAF expression 48 hours poststimulation with a combination of TNF-α and IFN-γ, show an increase in the MFI of up to 4-fold for both HUVECs and DMECs (Fig3A). To investigate the kinetics of this response, flow cytometry was performed on EC monolayers stimulated for 24, 48, and 72 hours with TNF-α and IFN-γ. An increase in DAF was first detectable after 24 hours of stimulation (Fig 3B), and was maximal by 72 hours and persisted to 96 hours (data not shown).
Time course of DAF upregulation on HUVECs and DMECs by cytokines. EC monolayers were stimulated for up to 72 hours with plain medium or a combination of TNF- (10 ng/mL) and IFN-γ (500 U/mL). After harvesting, single-cell suspensions were analyzed by flow cytometry for DAF expression using MoAb 5B2. (A) Upregulation of DAF on DMECs and HUVECs after 48 hours of stimulation with a combination of TNF- and IFN-γ: negative control (…), constitutive expression of DAF (—), and TNF- and INF-γ–induced DAF (filled histograms). (B) Kinetics for DAF expression on DMECs and HUVECs following stimulation with TNF- and IFN-γ. The figure is representative of 3 similar experiments on each cell type.
Time course of DAF upregulation on HUVECs and DMECs by cytokines. EC monolayers were stimulated for up to 72 hours with plain medium or a combination of TNF- (10 ng/mL) and IFN-γ (500 U/mL). After harvesting, single-cell suspensions were analyzed by flow cytometry for DAF expression using MoAb 5B2. (A) Upregulation of DAF on DMECs and HUVECs after 48 hours of stimulation with a combination of TNF- and IFN-γ: negative control (…), constitutive expression of DAF (—), and TNF- and INF-γ–induced DAF (filled histograms). (B) Kinetics for DAF expression on DMECs and HUVECs following stimulation with TNF- and IFN-γ. The figure is representative of 3 similar experiments on each cell type.
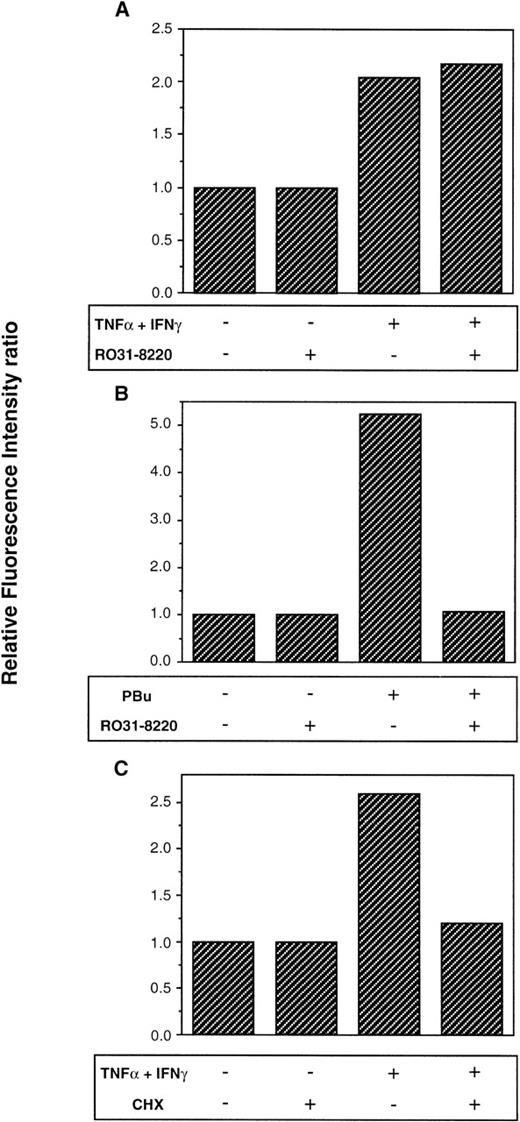
It is known that the activation of PKC in HUVECs by phorbol esters results in the upregulation of DAF on the cell surface.25To investigate whether PKC activation is required for the induction of DAF on cytokine-stimulated ECs, we used the specific PKC antagonist RO31-8220,29 which we have previously demonstrated to be an effective and nontoxic inhibitor of EC PKC.31 36 In these experiments, the HMEC-1 cell line was used and the cells were pretreated for 30 minutes with RO31-8220 before stimulation with TNF-α and IFN-γ or PBu. The induction of DAF following 48 hours of stimulation with TNFα and IFN-γ was not inhibited by RO31-8220, suggesting cytokine signaling via a PKC-independent pathway (Fig 4A). In contrast, the induction of DAF by PBu was completely inhibited by the presence of RO31-8220 (Fig 4B). In some experiments, treatment with RO31-8220 led to a small reduction in the constitutive expression of DAF, and the results are thus expressed as the RFI ratio to control for this effect as detailed earlier. RO31-8220 did not alter the constitutive expression of MCP, CD59, or EN4.
Effect of cycloheximide and the PKC antagonist RO31-8220 on DAF expression by ECs. HMECs plated at confluence in 35-mm petri dishes (6 × 105 cells/dish) and cultured overnight at 37°C were treated with (A, B) RO31-8220 (1 μmol/L) and (C) cycloheximide (CHX, 1 μg/mL) for 30 minutes before addition of activating factors. The cells were subsequently stimulated with (A, C) TNF- (10 ng/mL) and IFN-γ (500 U/mL), (B) PBu (50 ng/mL), or plain medium for 48 hours. After harvesting, DAF expression was measured by flow cytometry using MoAb 5B2, with MOPC-21 as an isotype-matched negative control. The figure shows the effect of (A, B) specific PKC antagonist RO31-8220 on TNF- and IFN-γ– and PBu-induced DAF expression, respectively, and (C) CHX on TNF- and IFN-γ–induced DAF. CHX also completely inhibited PBu-induced DAF (data not shown). To exclude the effects of nonspecific cytotoxicity, cell viability was assessed by monolayer morphology, cell-counting, and trypan blue exclusion on EC populations before staining (data not shown). To control for any effect of the antagonists on the constitutive expression of DAF, results are expressed as the RFI ratio. The figure is representative of 4 similar experiments.
Effect of cycloheximide and the PKC antagonist RO31-8220 on DAF expression by ECs. HMECs plated at confluence in 35-mm petri dishes (6 × 105 cells/dish) and cultured overnight at 37°C were treated with (A, B) RO31-8220 (1 μmol/L) and (C) cycloheximide (CHX, 1 μg/mL) for 30 minutes before addition of activating factors. The cells were subsequently stimulated with (A, C) TNF- (10 ng/mL) and IFN-γ (500 U/mL), (B) PBu (50 ng/mL), or plain medium for 48 hours. After harvesting, DAF expression was measured by flow cytometry using MoAb 5B2, with MOPC-21 as an isotype-matched negative control. The figure shows the effect of (A, B) specific PKC antagonist RO31-8220 on TNF- and IFN-γ– and PBu-induced DAF expression, respectively, and (C) CHX on TNF- and IFN-γ–induced DAF. CHX also completely inhibited PBu-induced DAF (data not shown). To exclude the effects of nonspecific cytotoxicity, cell viability was assessed by monolayer morphology, cell-counting, and trypan blue exclusion on EC populations before staining (data not shown). To control for any effect of the antagonists on the constitutive expression of DAF, results are expressed as the RFI ratio. The figure is representative of 4 similar experiments.
Cytokine-induced DAF on ECs requires protein synthesis.
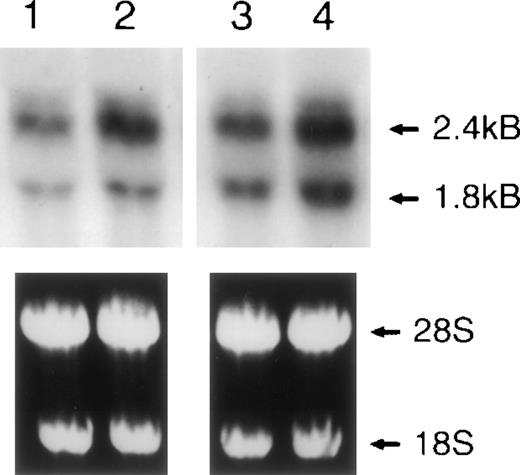
In experiments similar to those already described, HMECs were pretreated for 30 minutes with cycloheximide before stimulation with TNF-α and IFN-γ or PBu. The presence of cycloheximide completely inhibited the cytokine-induced (Fig 4C) and PBu-induced (data not shown) expression of DAF, suggesting that the induction of DAF is dependent on de novo protein synthesis. Northern blot analysis was performed using mRNA extracted from unstimulated ECs and cells stimulated with TNF-α and IFN-γ for up to 24 hours. DAF mRNA was detectable at a low level in unstimulated ECs and was clearly upregulated following a 6-hour stimulation with cytokines in both DMECs and HUVECs (Fig 5). Two DAF mRNA transcripts were detected at 2.4 and 1.8 kb, as previously reported.34 37 Quantification of mRNA levels in resting and cytokine-stimulated ECs using densitometric scanning demonstrated a 7-fold increase in DMECs and a 4-fold increase in HUVECs following 6 hours of stimulation with TNF-α and IFN-γ. After cytokine stimulation, the observed increase in DAF mRNA was first detectable at 3 hours and maximal at 6 to 8 hours, and declined to basal levels by 24 hours poststimulation (data not shown). Thus, the upregulation of cell-surface expression following stimulation of ECs with cytokines is associated with a transient increase in DAF steady-state mRNA.
Northern blot analysis of cytokine-induced DAF on HUVECs and DMECs. ECs were cultured for 6 hours in plain medium alone or supplemented with a combination of TNF- (10 ng/mL) and IFN-γ (500 U/mL). Total RNA was isolated and Northern blots were prepared. Lane 1, unstimulated DMECs; lane 2, TNF- and IFN-γ–stimulated DMECs; lane 3, unstimulated HUVECs; lane 4, TNF- and INF-γ–stimulated HUVECs. The ethidium bromide–stained gel confirmed equal loading of RNA in each lane. These findings were confirmed in 3 separate experiments.
Northern blot analysis of cytokine-induced DAF on HUVECs and DMECs. ECs were cultured for 6 hours in plain medium alone or supplemented with a combination of TNF- (10 ng/mL) and IFN-γ (500 U/mL). Total RNA was isolated and Northern blots were prepared. Lane 1, unstimulated DMECs; lane 2, TNF- and IFN-γ–stimulated DMECs; lane 3, unstimulated HUVECs; lane 4, TNF- and INF-γ–stimulated HUVECs. The ethidium bromide–stained gel confirmed equal loading of RNA in each lane. These findings were confirmed in 3 separate experiments.
Assembly of the MAC on ECs induces DAF expression.
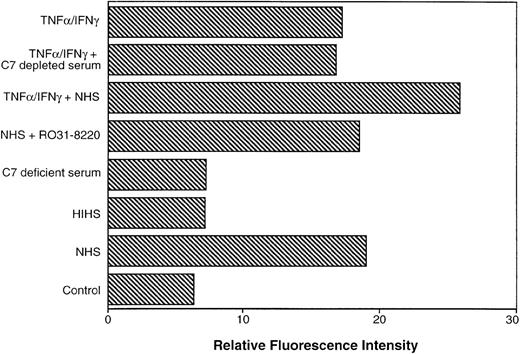
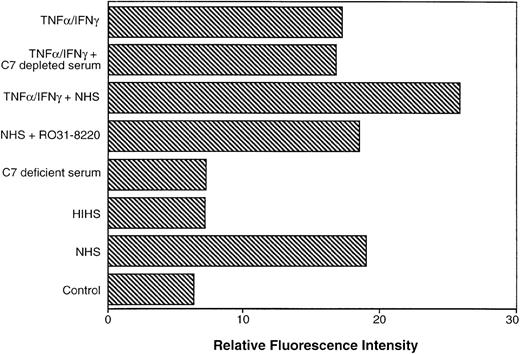
Endothelial cells at sites of inflammation may be activated by the MAC of complement and by proinflammatory cytokines. The effect of the MAC on EC DAF expression was studied by generating the C5b-9 complex at levels that were shown in our preliminary experiments to be sublytic to ECs. The EC monolayers were opsonized with an IgG2a anti-endoglin (CD105) MoAb RMAC8.38 IgG2a is the optimal murine isotype for C fixation, and endoglin was chosen as the target antigen because it is highly expressed on the EC surface and its expression is not upregulated by cytokines.39 Following opsonization, ECs were incubated with 2.5% NHS at 37°C to induce generation of the MAC. Exposure of HMECs to the MAC increased DAF expression on the cell surface up to 3-fold (Fig 6). Kinetic analysis demonstrated that this response was maximal at 24 hours and was maintained at 48 hours. Similar responses were observed at the same time points with HUVECs (data not shown). The dependence on C activation and the generation of the C5b-9 complex was demonstrated by the lack of response when either HIHS or C7-deficient serum were used instead of NHS (Fig 6). Furthermore, no response was found with C8-deficient serum, suggesting that generation of the C5b-7 complex is insufficient to induce DAF (data not shown). As with cytokine-stimulated DAF expression, inclusion of the PKC antagonist RO31-8220 did not inhibit MAC-induced DAF. It should be noted that the RFIs in these experiments were lower than those described earlier, since a directly FITC-labeled anti-DAF MoAb was used for the detection of DAF.
Upregulation of DAF on ECs following assembly of the MAC of complement. HMECs were plated at confluence in 24-well plates (2 × 105 cells/dish) and cultured overnight at 37°C. They were then opsonized with MoAb RMAC8 or negative control MoAb for 1 hour, followed by addition of 2.5% NHS to induce formation of the MAC. In parallel wells, ECs were pretreated with a combination of TNF- and IFN-γ for 16 hours before assembly of the MAC. Additional controls included the addition of HIHS or C7-deficient serum in place of NHS. To inhibit PKC, RO31-8220 was added for 30 minutes before assembly of the MAC and remained in the cultures throughout the assay. After a total incubation of 24 hours at 37°C, ECs were harvested and DAF expression was quantified by flow cytometry using an FITC-labeled anti-DAF MoAb.
Upregulation of DAF on ECs following assembly of the MAC of complement. HMECs were plated at confluence in 24-well plates (2 × 105 cells/dish) and cultured overnight at 37°C. They were then opsonized with MoAb RMAC8 or negative control MoAb for 1 hour, followed by addition of 2.5% NHS to induce formation of the MAC. In parallel wells, ECs were pretreated with a combination of TNF- and IFN-γ for 16 hours before assembly of the MAC. Additional controls included the addition of HIHS or C7-deficient serum in place of NHS. To inhibit PKC, RO31-8220 was added for 30 minutes before assembly of the MAC and remained in the cultures throughout the assay. After a total incubation of 24 hours at 37°C, ECs were harvested and DAF expression was quantified by flow cytometry using an FITC-labeled anti-DAF MoAb.
To investigate the combined effects of the MAC and proinflammatory cytokines on EC DAF expression, EC monolayers were treated with TNF-α and IFN-γ overnight prior to washing and opsonization as before. Pretreatment of ECs with cytokines followed by MAC generation induced an increase of DAF in excess of 3-fold, greater than the increase found with either the MAC or cytokines alone (Fig 6). This effect was dose-dependent (data not shown) and was maximal following treatment of ECs with 10 ng/mL TNF-α and 250 U/mL IFN-γ. Inclusion of C7-depleted serum instead of NHS did not enhance the response, and the increase in DAF levels was the same as observed following treatment with the cytokines alone. As predicted by the results described, inhibition of PKC by RO31-8220 did not abrogate this response (data not shown).
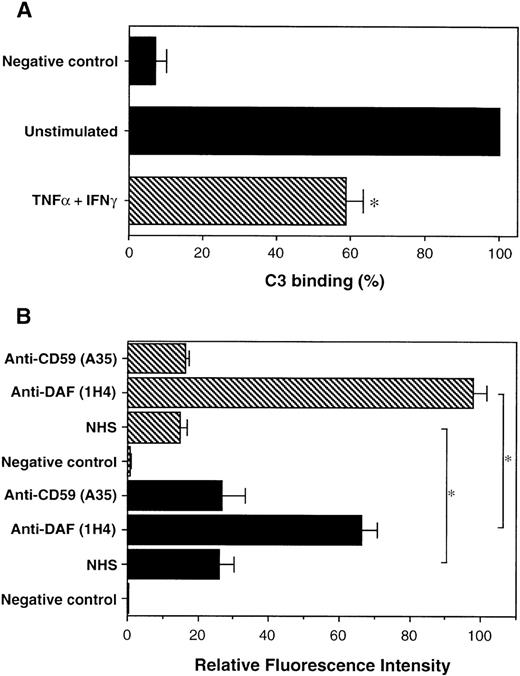
Cytokine-induced DAF reduces complement binding to ECs.
The binding of complement factor C3 to the EC surface was used to investigate whether the observed induction of DAF could afford increased protection to ECs against complement-mediated injury. HMEC monolayers were opsonized with RMAC8 followed by incubation with 20% NHS for 2 hours, after which C3 binding to the cell surface was quantified by flow cytometry using a FITC-labeled antibody against C3c. The addition of 10 mmol/L EDTA to the NHS completely inhibited C3 binding, confirming that the response was dependent on the classic pathway of complement activation (data not shown). Moreover, stimulation of ECs for 48 hours with TNF-α and IFN-γ before analysis reduced the deposition of C3 on the cell surface by 42% compared with unstimulated cells (P = .014; Fig 7A). Parallel flow-cytometric analysis confirmed that EC expression of endoglin was not altered by cytokine stimulation (data not shown). To confirm the role of DAF in the reduction of C3 binding following cytokine stimulation, the inhibitory anti-DAF MoAb 1H4, which does not fix complement (J.C.M. and D.O.H., unpublished observation, December 1998), was included in the assay. In addition, we also studied the effects of the non–complement-fixing, inhibitory anti-CD59 MoAb A35,40 which would not be expected to inhibit C3 binding. The addition of MoAb 1H4 markedly increased the binding of C3 to unstimulated opsonized ECs exposed to 20% NHS (Fig 7B). Furthermore, the reduction of C3 binding after 48 hours of prestimulation with TNF-α and IFN-γ was reversed by the presence of 1H4, with the resultant detected level of C3 significantly greater than that found on unstimulated ECs (P < .05). No significant increase in the binding of C3 was detected in the presence of either anti-CD59 or irrelevant control MoAbs. The inclusion of blocking MoAbs with DAF or CD59 did not significantly increase cell lysis at this concentration of NHS (data not shown). Therefore, these observations suggest that the increased levels of cell-surface DAF observed following stimulation with cytokines or the MAC may provide additional protection to ECs against complement-mediated injury during inflammation.
Functional analysis of cytokine-induced DAF on ECs. HMECs were plated at confluence in 35-mm petri dishes (6 × 105 cells/dish) and cultured overnight at 37°C. They were then stimulated with a combination of TNF- (10 ng/mL) and IFN-γ (500 U/mL) for 48 hours. After harvesting, ECs were incubated with the anti-endoglin MoAb RMAC8 or plain medium alone for 30 minutes at 4°C. In the blocking experiments, the anti-DAF MoAb 1H4, anti-CD59 MoAb A35, or isotype-matched negative control MoAb (final concentration, 50 μg/mL) were added to the assay with RMAC8. The ECs were then washed in HBSS/1% BSA before addition of 20% NHS for 2 hours at 37°C. Binding of C3 was detected by flow cytometry using FITC-conjugated rabbit anti–human C3. (A) Percent C3 binding (mean ± SD) to unstimulated (▪) and TNF- and IFN-γ–stimulated (▧), HMECs, with binding to unstimulated ECs shown as 100%: (B) changes in C3 binding (RFI mean ± SD) on unstimulated (▪) and TNF- and IFN-γ–stimulated (▧) HMECs in the presence of non–complement-fixing inhibitory MoAbs 1H4 (anti-DAF) and A35 (anti-CD59). *P < .05.
Functional analysis of cytokine-induced DAF on ECs. HMECs were plated at confluence in 35-mm petri dishes (6 × 105 cells/dish) and cultured overnight at 37°C. They were then stimulated with a combination of TNF- (10 ng/mL) and IFN-γ (500 U/mL) for 48 hours. After harvesting, ECs were incubated with the anti-endoglin MoAb RMAC8 or plain medium alone for 30 minutes at 4°C. In the blocking experiments, the anti-DAF MoAb 1H4, anti-CD59 MoAb A35, or isotype-matched negative control MoAb (final concentration, 50 μg/mL) were added to the assay with RMAC8. The ECs were then washed in HBSS/1% BSA before addition of 20% NHS for 2 hours at 37°C. Binding of C3 was detected by flow cytometry using FITC-conjugated rabbit anti–human C3. (A) Percent C3 binding (mean ± SD) to unstimulated (▪) and TNF- and IFN-γ–stimulated (▧), HMECs, with binding to unstimulated ECs shown as 100%: (B) changes in C3 binding (RFI mean ± SD) on unstimulated (▪) and TNF- and IFN-γ–stimulated (▧) HMECs in the presence of non–complement-fixing inhibitory MoAbs 1H4 (anti-DAF) and A35 (anti-CD59). *P < .05.
DISCUSSION
DAF is widely expressed on the surface of both hematopoietic and nonhematopoietic cells, suggesting that it plays an important role in protection against the toxic effects of complement activation.3,41 The evidence to date suggests that the surface expression of DAF may vary between tissues and may be regulated by both physiologic and pathophysiologic mechanisms.2,8,42,43 However, the understanding of the regulation of DAF and its functional significance remains incomplete.2 Our study demonstrates that exposure of ECs to soluble cytokines and cell-associated MAC, which may coexist at sites of inflammation, increases cell-surface expression of DAF. The data suggest that these factors, which promote leukocyte adhesion to and transmigration across the endothelium during inflammation, may also protect ECs against complement-mediated injury in chronic inflammatory disease.
In the present study, initial experiments confirmed the presence of DAF, MCP, and CD59 on HUVECs under basal culture conditions.10,12 In addition, we found that all three molecules are expressed at equivalent antigen densities on DMECs. The constitutive expression of complement-regulatory proteins is thought to protect the endothelium against the constant low-level activity of the alternative pathway.3,12 However, there is a greatly increased potential for local endothelial injury following activation of the classic or alternative pathways of complement. Under these circumstances, induction of complement-regulatory protein gene expression might be expected to maintain or enhance the protection of host tissues against complement-mediated injury. This hypothesis is supported by our current observations that TNF-α and IFN-γ induced DAF expression on ECs. This upregulation was dependent on increased steady-state mRNA and protein synthesis and was maximal at cytokine concentrations previously shown to optimally induce ICAM-1 and VCAM-1 on ECs.30 The relatively delayed time course of DAF protein upregulation on ECs is not unique and is comparable to that previously reported for the Thy-1 and major histocompatibility complex class I and II molecules on ECs.13,31 In contrast, we detected no change in the basal level of either MCP or CD59 following EC treatment with a variety of cytokines. Previous studies have demonstrated upregulation of DAF expression on HUVECs in response to stimulation with phorbol esters, wheat germ agglutinin, and histamine.25-27 Moreover, Moutabarrik et al28found a slight increase in DAF following stimulation of HUVECs with IL-1, lipopolysaccharide, and IL-4, but not with TNF, and a small increase in CD59 on TNF-stimulated cells. Although we also found a small increase in DAF on HUVECs in response to treatment with IL-4, this did not reach statistical significance and IL-4 had no effect on DAF expression by DMECs in our studies.
In addition to cytokines, there is compelling evidence that complement-activation products mediate changes in EC surface-antigen expression.15-17 Thus, the MAC is known to increase TNF-induced expression of E-selectin and ICAM-1 on ECs and thereby to increase neutrophil adhesion.19,22 This raised the question of whether the MAC itself is capable of influencing the expression of DAF on ECs. Using an in vitro model in which an anti-endoglin MoAb and NHS were used to localize complement activation to the EC surface, we observed a 3-fold increase in DAF, which was maximal 24 hours postactivation. The dependence of this response on generation of the C5b-9 complex was demonstrated by the failure of HIHS and C7- and C8-deficient serum to induce DAF. The lack of response with C8-deficient serum suggested that the complete C5b-9 complex is required and that the previously described signaling capacity of the C5b-7 complex44 is insufficient to induce DAF expression. While the response was consistently enhanced by prestimulation of ECs for 16 hours with TNF-α and IFN-γ, the effect of prestimulation with cytokines and the MAC together was typically additive rather than synergistic, as previously described for ICAM-1 and E-selectin.22
Our data therefore suggest that following activation of complement, generation of C5b-9 can induce a feedback loop of vascular protection via upregulation of DAF on the EC surface, a mechanism that is enhanced by the presence of proinflammatory cytokines. This may be important in human inflammatory diseases such as atherosclerosis, systemic lupus erythematosus, rheumatoid arthritis, and glomerulonephritis, in which complement-activation products may be deposited on the cell surface.7-9,45,46 Furthermore, the capacity of the MAC to stimulate DAF expression during EC exposure to sublytic concentrations of antibody and complement may contribute significantly to the phenomenon of accommodation, in which the endothelium becomes resistant to complement-fixing alloreactive or xenoreactive antibodies in the transplantation setting.47
The role of PKC in the regulation of DAF was studied using the PKC-specific inhibitor RO31-8220,29 which completely abrogated the PBu-induced upregulation of EC DAF.25However, the presence of RO31-8220 had no effect on the induction of DAF by TNF-α and IFN-γ. Furthermore, although PKC has been implicated as one of a number of potential signaling pathways activated by C5b-9,44,48,49 RO31-8220 had no effect on DAF induction by the MAC. These and other data36 suggest the presence in ECs of agonist-specific pathways for the regulation of surface proteins, which in turn may have important functional implications. It is therefore of particular interest that a recent study has shown that activation of PKC in HUVECs not only upregulates cell-surface DAF but also results in deposition of the molecule in the extracellular matrix.50 We have made similar observations with DAF and Thy-1 both in vitro (J.C.M. and D.O.H., unpublished observation, January 1995) and in situ in human skin, where both molecules were found in close association with the dermal vascular basement membrane.31,51 However, treatment of HUVECs with cytokines did not induce deposition of DAF in the extracellular matrix.50 Together, these observations indicate the presence of separate pathways for DAF induction in ECs, each of which may be capable of mediating a specific distribution of the molecule within the tissues.
The functional role of DAF on ECs was assessed by measurement of surface-bound C3. Stimulation with TNF-α and IFN-γ reduced C3 binding to the EC surface following activation of complement. Moreover, inclusion of an inhibitory anti-DAF MoAb (1H4) in the assay showed that this effect was mediated, at least in part, by increased cell-surface expression of DAF. This suggests that the upregulation of DAF to the levels observed after EC exposure to proinflammatory cytokines and/or the MAC provides enhanced endothelial protection. DAF-mediated cytoprotection may combine with other inducible protective mechanisms likely to be active during inflammation, including an increase in the synthesis of factors H and I, which specifically regulate alternative pathway activation.52,53 These mechanisms may be of particular importance in the light of recent data demonstrating that treatment of ECs with cytokines may result in complement activation and C3 deposition on the exposed subendothelial basement membrane.54
The evidence to date suggests that the relative hierarchy in terms of the physiologic importance of the complement-regulatory proteins is CD59 > DAF > MCP.2 However, our observations suggest that DAF is particularly important in providing additional EC protection during subacute and chronic inflammation, and this may reflect the inefficiency of terminal complement-component activation and its absolute dependence on excess C3 activation.55 In addition, the demonstration of distinct pathways for regulation raises the possibility that DAF may have functions in EC biology above and beyond decay-accelerating activity. DAF expression on the apical surface of ECs in response to cytokines would place DAF in a position to interact with leukocytes during their adhesion and transmigration to inflammatory sites. Indeed, a recent study has demonstrated an adhesive reaction between erythrocyte DAF and its ligand CD97, a molecule expressed on activated T lymphocytes and monocytes.56Finally, in light of the role of PKC in EC proliferation,57it is possible that the PKC-dependent pathway of DAF expression may be implicated in EC proliferation and angiogenesis.
In summary, we have demonstrated that DAF is expressed by cultured large- and small-vessel ECs and is inducible on these cells by PKC-dependent and -independent pathways. The increased level of DAF observed after exposure of ECs to cytokines and the MAC increases the level of protection against complement-mediated damage via a feedback loop, suggesting that this pathway may play an important role in maintaining vascular integrity during subacute and chronic inflammatory responses.
ACKNOWLEDGMENT
We are grateful to P. Kiely, P. Singh, L. Lovat, and M. McNamara for collection of the foreskins and to the staff of the maternity unit of Hammersmith Hospital for provision of the umbilical cords. We would like to thank Mark Walport, Bernie Morley, Marina Botto, Tony d’Apice, Teizo Fujita, Doug Lublin, and John Atkinson for their help in this study.
Supported by the Arthritis Research Campaign, The Medical Research Council (UK), and in part by a discretionary professorial award from the BHF.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Justin C. Mason, PhD, The BHF Cardiovascular Medicine Unit, National Heart and Lung Institute, Imperial College School of Technology and Medicine, Hammersmith Hospital, Du Cane Road, London W12 ONN, UK; e-mail: jmason@rpms.ac.uk.