Abstract
The occurrence of factor VIII (fVIII) inhibitory antibodies is a rare complication of fVIII substitution therapy in mild/moderate hemophilia A patients. fVIII mutations in certain regions such as the C1 domain are, however, more frequently associated with inhibitor, for reasons which remain unclear. To determine whether inhibitors could map to the mutation site, we analyzed at the clonal level the immune response of such a patient with an inhibitor to wild-type but not self-fVIII and an Arg2150His substitution in the C1 domain. Immortalization of the patient B lymphocytes provided a cell line producing an anti-fVIII IgG4κ antibody, LE2E9, that inhibited fVIII cofactor activity, following type 2 kinetics and prevented fVIII binding to von Willebrand factor. Epitope mapping with recombinant fVIII fragments indicated that LE2E9 recognized the fVIII C1 domain, but not the Arg2150His-substituted C1 domain. Accordingly, LE2E9 did not inhibit Arg2150His fVIII activity. These observations identify C1 as a novel target for fVIII inhibitors and demonstrate that Arg2150His substitution alters a B-cell epitope in the C1 domain, which may contribute to the higher inhibitor incidence in patients carrying such substitution. (Blood. 2000; 95:156-163)
Hemophilia A is an X-linked bleeding disorder characterized by the absence or an insufficient amount of functional factor VIII (fVIII). This deficiency affects 1 in 10 000 males and results in bleeding in joints, muscles, and soft tissues. Patients affected by the severe form of the disease (fVIII activity < 0.01 IU/mL) suffer from spontaneous bleedings, whereas in moderate or mild hemophilia A (fVIII activity 0.01 to 0.05 IU/mL and 0.06 to 0.4 IU/mL, respectively), bleeding can occur after minor trauma or surgery. The fVIII molecule is a 330 kD glycoprotein produced by the liver as a single polypeptide chain of 2332 amino acids that subsequently undergoes proteolytic processing.1 The circulating fVIII molecule consists of 2 chains. The heavy chain is constituted of the A1 and A2 domains and variable lengths of the B domain; the light chain contains the A3 domain and the C1 and C2 domains. In plasma, fVIII circulates complexed to von Willebrand factor (vWf) which protects it from rapid degradation.2 On cleavage by thrombin, activated fVIII dissociates from vWf,3 binds to negatively charged phospholipids, and participates as a cofactor to factor IXa in the factor X activating (tenase) complex.
Replacement therapy relies on the use of fVIII concentrates prepared from plasma or of recombinant fVIII (rfVIII). However, such a treatment can elicit the production of specific antibodies neutralising fVIII function, also called inhibitors.4 Several factors contribute to the development of an immune response toward fVIII. Recent evidence has shown that product-related factors can be involved in induction of inhibitors.5,6 Host-related factors play a major role in determining the incidence of inhibitors. Possible association between inhibitor formation and HLA haplotypes has recently been suggested.7,8 In severe hemophilia, there is a close relationship between the fVIII gene defect and the production of inhibitors: patients with severe gene defects such as nonsense mutations, large deletions or gene inversions are more likely to produce inhibitors than those with small deletions or missense mutations.9-11
In agreement with the concept that the presence of self-fVIII, although functionally altered or produced at reduced levels, contributes to render the immune system tolerant to fVIII, the development of inhibitor antibodies in mild hemophilia A is a rare event.12 Usually, the inhibitor is of low titer and transient.13 High-titer inhibitor associated with an anamnestic humoral response after replacement therapy has, however, been observed in some patients. Typically, in such cases, the inhibitor causes a fall of plasma fVIII levels,13 which transforms the bleeding phenotype of the patient into that of a severe hemophiliac. An immune response restricted to wild-type fVIII has recently been reported in mild hemophilia A patients with mutation Arg593-> Cys14 and Arg2150-> His.15Antibodies recognizing wild-type but not self-fVIII represent unique opportunities to study the influence of B-cell epitope alteration on the development of an immune response toward fVIII.
A detailed analysis of the specificity of fVIII inhibitors has proven to be difficult because of the large diversity of the humoral response, including antibodies which do not interfere with fVIII activity.16 Moreover, anti-idiotypic antibodies have been described that can neutralize fVIII inhibitors.17,18 To circumvent difficulties inherent to the use of polyclonal antibodies, we produced human monoclonal antibodies directed toward fVIII and representative of patients' pathogenic antibodies. Preliminary experiments have established that memory B cells from hemophilia A patients with inhibitor can be immortalized with EBV after CD40 cross-linking.19 We have applied the same strategy to characterize at the clonal level the relationship between alteration of fVIII B-cell epitopes and humoral response of a mild hemophilia A patient with inhibitor who maintained significant endogenous fVIII activity despite the presence of a high level of fVIII inhibitor.15
The fVIII gene mutation carried by patient LE was located in the C1 domain, ie, a region in which mutations are associated with a higher incidence of inhibitors in mild/moderate hemophilia A patients.13 However, the reason for such an association is still unclear. The fact that LE polyclonal antibodies recognized normal but not self-fVIII could be accounted for by elimination of a B cell epitope(s) through conformational changes induced at the mutation site in the C1 domain. Alternatively, other regions of the fVIII molecule could be affected by the mutation, as recently demonstrated for the substitution Arg2159Cys in the C1 domain, which altered an epitope located in the C2 domain.20 Mutations in the C1 domain are commonly identified in hemophilia A patients, yet the role of the latter domain in fVIII function or stability is not determined.21 22 Moreover, inhibitor antibodies recognizing the C1 domain have never been demonstrated. Clonal characterization of patient LE antibodies offered, therefore, the potential of determining whether epitopes recognized by inhibitor antibodies were located in the C1 domain, but also provided an opportunity to analyze the structure/function relationship of a fVIII domain whose function is still completely unknown.
Material and methods
Reagents
Human rfVIII (specific activity: 4000 IU/mg) was obtained from Hyland (Glendale, CA) as material for laboratory use only; plasma-derived (pd) fVIII-vWf complex, purified by ion exchange chromatography (specific activity ± 160 IU/mg protein; 15:1 vWf to fVIII w/w ratio), and purified fVIII-depleted vWf (vWf to fVIII w/w ratio 4800:1; lot 951 016) were obtained from the Belgian Red Cross (Brussels, Belgium).
Immortalization of human PBMC
Blood was collected from a mild hemophilia A patient with inhibitor (LE), after informed consent. This 59-year-old patient who had been treated on several occasions with fVIII concentrates had a fVIII activity of 0.23 IU/mL (with 23% of fVIII antigen level), despite a high titer inhibitor (305 Bethesda units, BU).15,32 PBMC were immortalized by infection with the Epstein-Barr virus and cloned according to described procedures.19 23
Sequencing of immunoglobulin genes
V region gene usage was determined by reverse transcriptase polymerase chain reaction (RT-PCR) amplification and sequence analyses using primers specific for the C region gene, and each of the V region gene families.24 The complete sequences of the VH and VL have been submitted to the EMBL Nucleotide Sequence Database under the accession numbers AJ009732 and AJ009733, respectively.
Purification of human IgG
Human monoclonal antibodies were purified by adsorption on immobilized Protein A (high-TRAP® Protein A; Pharmacia, Uppsala, Sweden). Fab fragments of human monoclonal antibody were prepared by papain digestion. One milligram of LE2E9 was diluted at 500 μg/mL in 100 mmol/L phosphate buffer, pH 7.0, containing 50 mmol/L L-cystein (Sigma Chemicals, St Louis, MO), 1 mmol/L EDTA (Merck, Darmstadt, Germany) and 10 μg papain (Sigma). The mixture was incubated for 3 hours at 37°C with continuous agitation. The reaction was stopped by addition of iodoacetamide to a final concentration of 75 mmol/L and a further incubation of 30 minutes at RT. The digested antibody was dialyzed against phosphate-buffered saline, pH 7.4. Undigested IgG and Fc fragments were then eliminated by passage over immobilized Protein A Sepharose. Fab fragments were further purified by gel filtration chromatography on a Superdex 200 (Pharmacia).
Immunoassays
Previously described methods were used for the detection of anti-fVIII IgG antibodies,19 the determination of IgG subclass,18 and the evaluation of inhibition of fVIII binding to vWf.19 For analysis of the inhibition of rfVIII binding to LE2E9 by Fab or native LE2E9, Maxisorb polystyrene plates (Nunc, Roskilde, Denmark) were incubated for 2 hours with 50 μL of LE2E9 diluted at 5 μg/mL in glycine-buffered saline, 20 mmol/L glycine, 34 mmol/L NaCl, pH 9.2, and washed. Biotin-labeled rfVIII (50 μL) diluted to 1 μg/mL in Tris-casein (10 mmol/L tris(hydroxymethyl)-aminoethane, pH 7.3, containing 150 mmol/L NaCl and 0.5% casein) were mixed for 1 hour at 37°C with 50 μL of human IgG or Fab fragments at various concentrations. A 50-μL aliquot of the mixture was added to the plates for an incubation of 2 hours at RT. After washing, the binding of biotin-labeled rfVIII was detected by sequential addition of avidin-peroxidase and OPD.
fVIII inhibition in functional assays
rfVIII (final concentration 0.2 μg/mL) was incubated with human IgG antibody at different concentrations for 2 hours at 37°C and the residual fVIII activity was assessed by a chromogenic assay (Coatest® Factor VIII, Chromogenix AB, Mölndal, Sweden). Inhibition of plasma fVIII activity was measured by the Bethesda method,25 in which a pool of normal plasma collected in buffered trisodium citrate was used as fVIII source. Residual fVIII activity was assessed by a chromogenic or by a 1-stage clotting assay.
Cloning of normal and mutated fVIII cDNA fragments
All DNA fragments encoding fVIII domains were generated by PCR using primers bound by the restriction sites HindIII (italic) and Not1 (underlined) sites. Sense primers, named according to the first fVIII amino acid residue encoded (codon in bold), were as follows:
1981: 5′-GATGCGAAGCTTGGTGTTTTTGAGACAGTGGAAATG-3′;
1692: 5′-GATGCGAAGCTTCAAAAGAAAACACGACAC-3′;
2146: 5′-GCTCGATACATCCATTTGCACCCAACTC-3′;
2010: 5′-GATGCGAAGCTTATGAGCACACTTTTTCTGGTGTAC-3′;
2125: 5′-GATGCGAAGCTTGTCTTCTTTGGCAATGTGGATTCA-3′;
2170: 5′-GATGCGAAGCTTGATTTAAATAGTTGCAGCATGCCA-3′;
1637: 5′-TCGAAAAAGCTTGGATCCTCTCAAAACCCACCAGTCTTGAAACGC-3′
1692: 5′-TCGAAAAAGCTTGGATCCCAAAAGAAAACACGACACTATTTTATT-3′
2010: 5′-TCGAAAAAGCTTGGATCCATGAGCACACTTTTTCTGGTGTACAGC-3′
The antisense primers, named accorded to the last encoded amino acid residue, were as follows:
2043: 5′-TTCTCGACTTGCGGCCGCATATTGTCCTGAAGCTGTAATCTG-3′;
2222: 5′-TTCTCGACTTGCGGCCGCCTGAGGACGCCAGGCATTACTCCTC-3′;
2332: 5′-TTCTCGACTTGCGGCCGCGTAGAGGTCCTGTGCCTCGCAGCC-3′;
2155: 5′-GAGTTGGGTGCAAATGGATGTATCGAGC-3′;
2173: 5′-TTCTCGACTTGCGGCCGCACTATTTAAATCACAGCCCATCAAC-3′.
Primers 2146 and 2155 carry the substitutions G— > A and C— > T (bold and underlined), respectively, responsible for the Arg— > His substitution in fVIII. All PCR products were subcloned in frame into Signal pIgplus (R&D Systems Europe Ltd, Abingdon, UK) and controlled by sequencing in both directions on a ABI Genetic Analyser 3.10 (Perkin Elmer). The complete cDNA of human rfVIII cloned in pSP64 (American Tissue Collection Inc, Rockville, MD) was used as template in the construction of plasmids encoding wild-type fVIII fragments.
A cDNA fragment encoding the fVIII light chain carrying the mutation Arg2150His was produced by Splicing by Overlap Extension-PCR.26 Briefly, 2 PCR fragments were generated using complete cDNA of human rfVIII cloned in pSP64 (American Tissue Collection Inc) as template and a couple of primers (sense: GATGCGAAGCTTCAAAAGAAAACACGACAC and antisense: 2155 and sense, 2146: GCTCGATACATCCATTGCACCCAACTC, and antisense, 2332, respectively). After primerless PCR assembly and reamplification with primers 1692 and 2332, the DNA fragments were digested with HindIII and Not1 and ligated in frame into Signal pIgplus (R&D Systems). This construct was used as template for the production of plasmid encoding all fVIII framents containing the Arg2150His mutation.
Expression of fVIII recombinant fragments in reticulocyte transcription/translation system
DNA 500 ng to 1 μg, linearized by Not1 digestion, was used as a template in a T7 RNA polymerase transcription system in micrococcal nuclease-treated reticulocyte lysates (Promega, Southampton, UK) according to the manufacturer's instructions in the presence of L-[35S]methionine (Amersham, Bucks, UK). The [35S]-methionine labeled fVIII fragments migrated on SDS-PAGE as bands matching the expected mass of corresponding fVIII polypeptides.
Immunoprecipitation of L-[35S]methionine-labeled fVIII fragments
Standard in vitro translation product 1 to 3 μL was added to 500 μL human antibody at 2 μg/mL in NET-gel buffer 50 mmol/L Tris-HCl, pH 7.5; 150 mmol/L NaCl; 0.1% Nonided NP-40;1 mmol/L EDTA (pH 8; 0.25% gelatin and 5% BSA). Tubes were gently rocked for 1 hour at 4°C. Twenty microliters of a 50% solution of Protein A Sepharose was then added to the antigen/antibody mixture, and incubated for 1 hour at 4°C on a rocking platform. The Sepharose beads were centrifuged and washed twice with Tris-NP40 10 mmol/L Tris-HCl (pH 7.5; 0.1% NP40). Bound antigen/antibody complexes were eluted from the beads by boiling for 4 minutes in 30 μL of SDS gel loading buffer. An aliquot of 15 μL was analyzed by 10% (w/v) polyacrylamide gel electrophoresis and visualized by autoradiography. The intensity of the bands was scored as plus (+) or minus (−) by 2 independent investigators. Control experiments were performed with the human monoclonal antibody BO2C11, directed toward the fVIII C2 domain,19 a rabbit polyclonal IgG antibody (aA3) directed toward amino acid residues 1797-1815 of the fVIII A3 domain and purified by immunoadsorption on the corresponding insolubilized synthetic peptide (kind gift of M. Di Giambattista and R. Laub, Belgian Red Cross), and normal donor's polyclonal IgG antibodies (Wi) purified on Protein A Sepharose.
Results
Production and characterization of the human monoclonal antibody LE2E9
The PBMC of a hemophilia A patient with inhibitor, LE, were immortalized by EBV infection concomitantly to activation by CD40 cross-linking. Four hundred and eighty cell lines were screened by ELISA for production of antibodies toward fVIII. One cell line, LE2E9, was successfully cloned by limiting dilution. Clonality was verified by RT-PCR amplification of mRNA coding for the V regions of the antibody heavy and light chains: a single sequence was obtained from 10 clones of PCR products. The V region of LE2E9 heavy chain gene was most homologous to DP-64, a member of the VH-4 gene family and the J region was most homologous to JH4b. Sequencing of the cloned light chain gene identified the V region gene as a Vκ3 and the J region gene as a Jκ4. Purified antibodies were obtained by passage of LE2E9 cell culture supernatant on Protein-A Sepharose. An ELISA performed with IgG subclass- and light chain-specific antibodies identified LE2E9 as an IgG4κ.
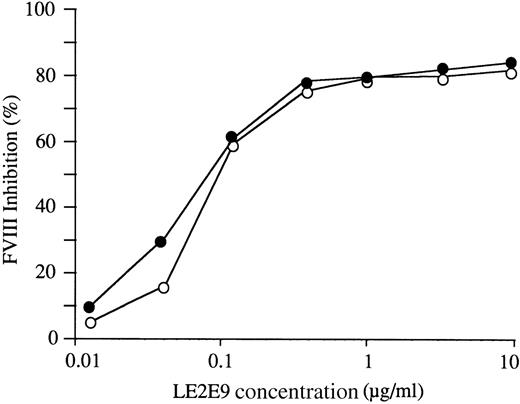
LE2E9 inhibits wild-type allogeneic but not syngeneic fVIII
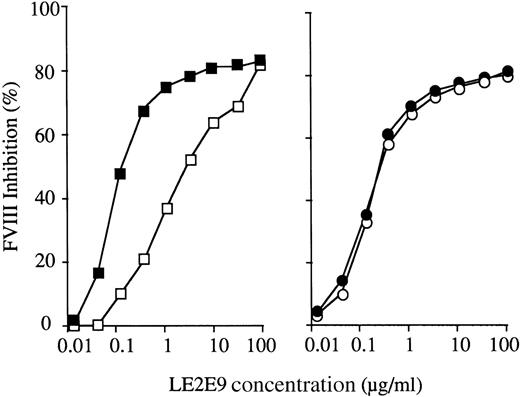
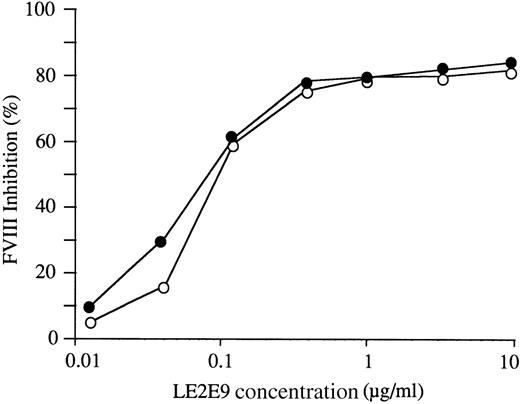
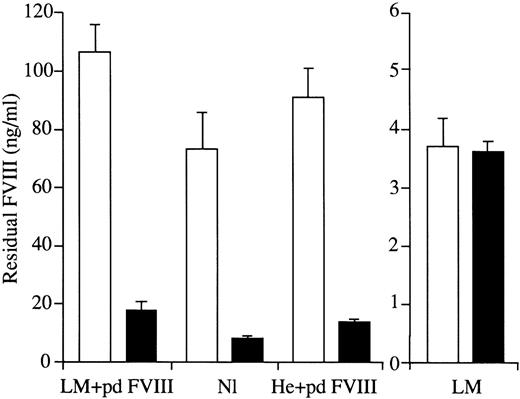
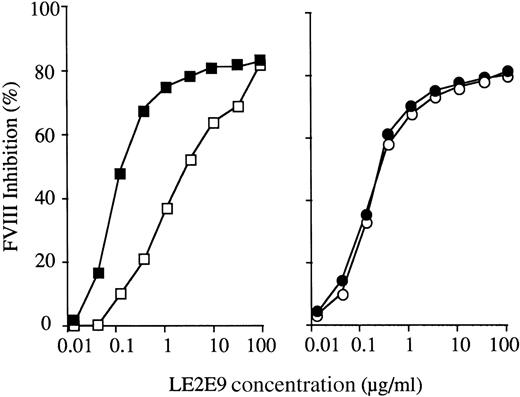
LE2E9 inhibited fVIII with high specific activity: when 1 volume of LE2E9 was mixed with 1 volume of rfVIII at 0.2 μg/mL for an incubation of 2 hours at 37°C, the final LE2E9 concentration required to inhibit 50% of fVIII activity was 0.1 μg/mL (Figure1). However, even in the presence of a large excess of LE2E9 (10 μg/mL), the inhibition remained incomplete (85%). In control experiments, fVIII activity was reduced by more than 95% after incubation with the human monoclonal antibody, BO2C11, at 1 μg/mL.19 Similar results were obtained when a pool of normal plasma was used as a source of fVIII (Figure 1) and when residual fVIII activity was evaluated either by chromogenic or 1-stage coagulation assays. By contrast, LE2E9 did not reduce the fVIII activity present in the plasma of patient LE's brother (LM), a mild hemophilia A patient with a fVIII level of 0.09 IU/mL (Figure2). Likewise, no inhibition of fVIII activity was observed when LE2E9 was incubated with plasma of the patient from whom the LE2E9 cell line had been derived.
Inhibition of fVIII functional activity.
Equal volumes of LE2E9 and of rfVIII (■) or of normal plasma (○) were incubated for 2 hours at 37°C. LE2E9 concentrations before mixing with plasma were as indicated. The residual fVIII activity was measured in a chromogenic assay.
Inhibition of fVIII functional activity.
Equal volumes of LE2E9 and of rfVIII (■) or of normal plasma (○) were incubated for 2 hours at 37°C. LE2E9 concentrations before mixing with plasma were as indicated. The residual fVIII activity was measured in a chromogenic assay.
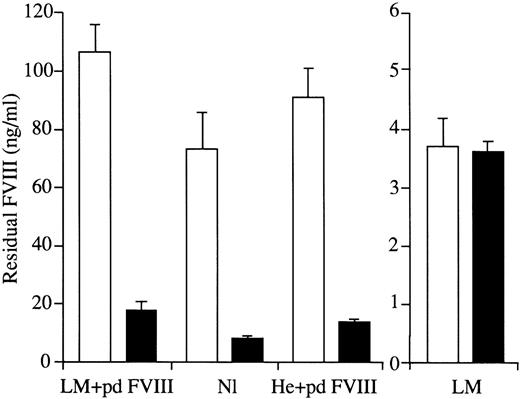
Inhibition of Arg2150His fVIII activity by LE2E9.
Equal volumes of buffer (open bars) or LE2E9 (10 μg/mL, solid bars) and of plasma were mixed and incubated for 1 hour at 37°C. The residual fVIII activity was measured in a fVIII chromogenic assay. Plasma samples were: pool of normal plasma (Nl), LM plasma (LM), LM plasma supplemented with pdfVIII (LM + pdfVIII), and plasma of a severe hemophilia A patient supplemented with pdfVIII (He + pdfVIII). The mean residual fVIII activities with standard deviations of 3 independent experiments are shown.
Inhibition of Arg2150His fVIII activity by LE2E9.
Equal volumes of buffer (open bars) or LE2E9 (10 μg/mL, solid bars) and of plasma were mixed and incubated for 1 hour at 37°C. The residual fVIII activity was measured in a fVIII chromogenic assay. Plasma samples were: pool of normal plasma (Nl), LM plasma (LM), LM plasma supplemented with pdfVIII (LM + pdfVIII), and plasma of a severe hemophilia A patient supplemented with pdfVIII (He + pdfVIII). The mean residual fVIII activities with standard deviations of 3 independent experiments are shown.
To rule out the possibility that the lack of inhibition of LM fVIII was due to quantitative or qualitative alteration of vWf or to the presence of anti-idiotypic antibodies, patient LM's plasma was supplemented with pdfVIII and incubated with LE2E9. As shown in Figure 2, wild-type pdfVIII mixed in LM plasma was inactivated by LE2E9 as well as fVIII in normal plasma or pdfVIII mixed in plasma of a patient with severe hemophilia A. Capture experiments were carried out to exclude that LE2E9 bound to mutated Arg2150His fVIII without reducing its activity. LE2E9 was insolubilized onto Protein A Sepharose and incubated with normal or patient LE's plasma. No reduction of fVIII activity was observed in patient LE's plasma whereas normal plasma activity was reduced by more than 80%.
LE2E9 does not recognize a recombinant fVIII light chain carrying the mutation Arg2150His
The absence of recognition of Arg2150His fVIII suggested that the epitope recognized by LE2E9 was located on the fVIII light chain. In addition, LE2E9 bound to purified isolated fVIII light chain but not to the fVIII heavy chain in ELISA (data not shown). To demonstrate that in the absence of plasma, LE2E9 did not recognize the mutated fVIII light chain, DNA fragments encoding wild-type and mutated fVIII light chains were synthesized. The corresponding proteins were expressed in reticulocyte lysates. The correct folding of native and mutated light chains was determined by immunoprecipitation with the human monoclonal antibody BO2C11, which recognizes a conformational epitope within the carboxy-terminal part of the fVIII light chain.19Immunoprecipitation experiments indicated that BO2C11 bound wild-type and Arg2150His light chains, whereas LE2E9 captured exclusively the wild-type light chain (Figure 3). Prolonged exposure of SDS-PAGE gels to the autoradiography film failed to detect any significant binding of LE2E9 to the mutated light chain. Control experiments showed no binding to assay reagents other than fVIII or fVIII fragments, and preincubation with soluble rfVIII prevented the binding to methionine-labeled fVIII fragments, confirming the binding specificity.
Immunoprecipitation of wild-type and mutated rfVIII light chain.
Recombinant fVIII fragments labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 (LE) bound to Protein A Sepharose. After washing, bound material was eluted by SDS-buffer and analyzed by SDS-PAGE, followed by autoradiography. Controls included a human monoclonal antibody, BO2C11 (BO), directed toward the fVIII C2 domain,19 a rabbit polyclonal IgG antibody (aA3), directed toward amino acid residues 1797-1815 of the fVIII A3 domain and normal donor polyclonal IgG antibodies (Wi). The experiments were repeated 3 times with similar results.
Immunoprecipitation of wild-type and mutated rfVIII light chain.
Recombinant fVIII fragments labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 (LE) bound to Protein A Sepharose. After washing, bound material was eluted by SDS-buffer and analyzed by SDS-PAGE, followed by autoradiography. Controls included a human monoclonal antibody, BO2C11 (BO), directed toward the fVIII C2 domain,19 a rabbit polyclonal IgG antibody (aA3), directed toward amino acid residues 1797-1815 of the fVIII A3 domain and normal donor polyclonal IgG antibodies (Wi). The experiments were repeated 3 times with similar results.
LE2E9 binds to the C1 domain
LE2E9 did not recognize fVIII in Western blotting (unpublished data, 1996), indicating that the epitope recognized was conformational. Further epitope mapping was therefore performed with fVIII fragments produced in reticulocyte lysates. Preliminary experiments had indicated that such an approach was efficient for the synthesis of fVIII domains. The immunoprecipitation procedure using labeled fVIII domains produced in reticulocyte lysate was validated by mapping the epitope recognized by the human monoclonal antibody BO2C11. A complete agreement was observed between the binding to fVIII C2 deletion fragments produced in reticulocyte lysates and the binding to recombinant fragments produced in Escherichia coli or COS cells (unpublished data, 1997, and Figure 4). LE2E9 bound to full-length light chain, to fragments corresponding to A3C1, C1C2, and the isolated C1 domain (Figure 4). By contrast, as shown in Figure5, LE2E9 did not bind to the C1 or C1C2 domains with the substitution Arg2150His, although in a control experiment, the Arg2150His C1C2 domain was bound by BO2C11 like its normal counterpart.
Epitope mapping of LE2E9.
(A) Structure of circulating fVIII. Each domain of fVIII is identified by a letter in upper case followed by a numeral. The small acidic regions are indicated by a1, a2, and a3, respectively. The copper ion involved in the non-covalent association of the A1 and A3 domains is indicated. (B) Recombinant fVIII fragments labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 bound to Protein A Sepharose. After washing, bound material was eluted and analyzed by SDS-PAGE, followed by autoradiography. Recombinant fVIII fragments are indicated by open bars. The amino- and carboxy-terminal extremities of fragments are as indicated. Control experiments were carried out with a human monoclonal antibody, BO2C11, directed toward the fVIII C2 domain19 and a rabbit polyclonal IgG antibody, aA3, directed toward amino acid residues 1797-1815 of the fVIII A3 domain The experiments were repeated at least 3 times with comparable results.
Epitope mapping of LE2E9.
(A) Structure of circulating fVIII. Each domain of fVIII is identified by a letter in upper case followed by a numeral. The small acidic regions are indicated by a1, a2, and a3, respectively. The copper ion involved in the non-covalent association of the A1 and A3 domains is indicated. (B) Recombinant fVIII fragments labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 bound to Protein A Sepharose. After washing, bound material was eluted and analyzed by SDS-PAGE, followed by autoradiography. Recombinant fVIII fragments are indicated by open bars. The amino- and carboxy-terminal extremities of fragments are as indicated. Control experiments were carried out with a human monoclonal antibody, BO2C11, directed toward the fVIII C2 domain19 and a rabbit polyclonal IgG antibody, aA3, directed toward amino acid residues 1797-1815 of the fVIII A3 domain The experiments were repeated at least 3 times with comparable results.
Binding of LE2E9 to native or Arg2150His C1 and C1C2 domains.
Native and Arg2150His recombinant fVIII C1 domain (A) or C1C2 domains (B) labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 (LE) bound to Protein A Sepharose. After washing, bound material was eluted by SDS-buffer and analyzed by SDS-PAGE, followed by autoradiography. Controls included the human monoclonal antibody, BO2C11 (BO), and normal donor polyclonal IgG antibodies (Wi). The experiments were repeated 3 times with similar results.
Binding of LE2E9 to native or Arg2150His C1 and C1C2 domains.
Native and Arg2150His recombinant fVIII C1 domain (A) or C1C2 domains (B) labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 (LE) bound to Protein A Sepharose. After washing, bound material was eluted by SDS-buffer and analyzed by SDS-PAGE, followed by autoradiography. Controls included the human monoclonal antibody, BO2C11 (BO), and normal donor polyclonal IgG antibodies (Wi). The experiments were repeated 3 times with similar results.
A fVIII carrying a Pro2153Gln substitution is partially resistant to LE2E9
The observation that mutation Arg2150His in C1 completely prevented the binding of LE2E9 to fVIII prompted us to search for other mutations in the light chain that could alter the binding of LE2E9. As shown in the Table, LE2E9 inhibited the activity of all mutated fVIII molecules tested so far, except those carrying the mutation Arg2150His. Partial resistance to inactivation by LE2E9 was conferred by the Pro2153Gln substitution but not by the Arg2159Leu substitution in the C1 domain. As indicated in Figure6, LE2E9 at a concentration of 3 μg/mL inhibited 50% of Pro2153Gln fVIII activity, whereas 15-fold less LE2E9 was required to inhibit 50% activity of normal rfVIII added in Pro2153Gln fVIII plasma. The prevention of the inhibition was not due to the interaction of vWf or anti-idiotypic antibodies, as rfVIII added to the patient's plasma containing Pro2153Gln fVIII was inactivated like fVIII in control plasma.
Inhibition of Pro2153Gln fVIII functional activity by LE2E9.
Equal volumes of LE2E9 and of plasma, supplemented or not with rfVIII at 0.5 IU/mL, were incubated for 2 hours at 37°C (□, Pro2153Gln plasma; ▪, Pro2153Gln plasma supplemented with rfVIII; ○, Arg2159cys plasma; ■, Arg2159Cys plasma supplemented with rfVIII). LE2E9 concentrations before mixing with plasma were as indicated. The residual fVIII activity was measured in a chromogenic assay.
Inhibition of Pro2153Gln fVIII functional activity by LE2E9.
Equal volumes of LE2E9 and of plasma, supplemented or not with rfVIII at 0.5 IU/mL, were incubated for 2 hours at 37°C (□, Pro2153Gln plasma; ▪, Pro2153Gln plasma supplemented with rfVIII; ○, Arg2159cys plasma; ■, Arg2159Cys plasma supplemented with rfVIII). LE2E9 concentrations before mixing with plasma were as indicated. The residual fVIII activity was measured in a chromogenic assay.
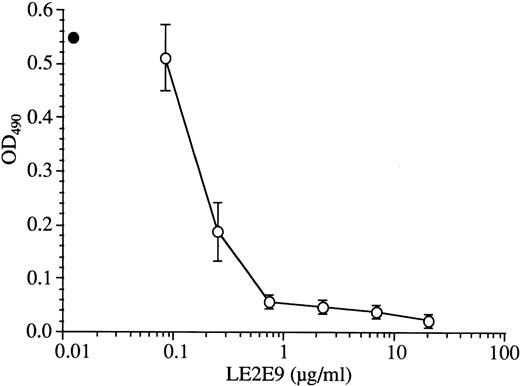
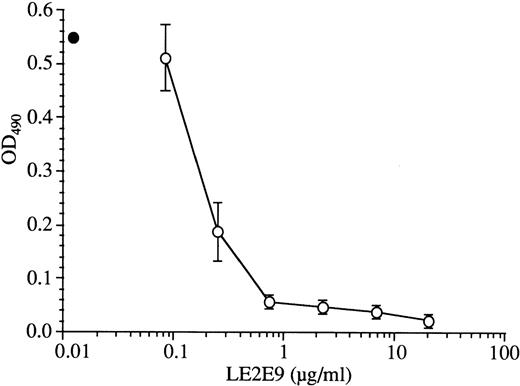
LE2E9 inhibits fVIII binding to vWf
The capacity of LE2E9 to inhibit the binding of fVIII to vWf was assessed in ELISA. Figure 7 shows that LE2E9 inhibited the binding of fVIII to vWf in a dose-dependent manner. The concentration of LE2E9 required to achieve 50% inhibition (IC50) of fVIII binding was 0.25 μg/mL and more than 95% inhibition was obtained with 20 μg/mL of LE2E9.
Inhibition of fVIII binding to vWf.
rfVIII at 0.2 μg/mL final concentration was mixed for 30 minutes at 37°C with different concentrations of LE2E9 before addition to vWf-coated plates. The plates were then incubated for 2 hours at RT, and the binding of fVIII was detected by addition of the HRP-labeled anti-fVIII A2 domain mAbF15B12. The mean of fVIII binding in the absence (■) or presence of antibody (○) with the standard deviation of triplicates are indicated. Controls in the absence of fVIII gave OD490 lower than 0.05. The experiments were repeated 3 times with similar results.
Inhibition of fVIII binding to vWf.
rfVIII at 0.2 μg/mL final concentration was mixed for 30 minutes at 37°C with different concentrations of LE2E9 before addition to vWf-coated plates. The plates were then incubated for 2 hours at RT, and the binding of fVIII was detected by addition of the HRP-labeled anti-fVIII A2 domain mAbF15B12. The mean of fVIII binding in the absence (■) or presence of antibody (○) with the standard deviation of triplicates are indicated. Controls in the absence of fVIII gave OD490 lower than 0.05. The experiments were repeated 3 times with similar results.
Fab fragments of LE2E9 also inhibited fVIII binding to vWf. However, on a molar basis, 15 times more Fab than native LE2E9 was required to inhibit 50% of fVIII binding to vWf (data not shown). Additional experiments were carried out to exclude that the LE2E9 Fab fragments still contained intact or partially digested antibody. SDS-PAGE analysis of the Fab fragments purified by Protein-A adsorption and gel filtration chromatography showed a single band. The presence of trace amounts of Fcγ fragments in the Fab fragment preparation was further excluded by ELISA. Thus, fVIII-coated plates were incubated with native or Fab LE2E9. Binding of both Fab and native LE2E9 was detected by addition of peroxidase-labeled anti-κ light chain IgG. By contrast, addition of peroxidase-labeled anti-Fcγ IgG did not detect any binding of the Fab fragment preparation even at a Fab concentration as high as 100 μg/mL. By comparison, addition of 0.1 μg/mL of native LE2E9 was sufficient to result in significant binding. In ELISA, a 15-fold higher concentration of Fab than of native antibody was required to inhibit 50% of the binding of biotin-labeled LE2E9 onto insolubilized fVIII (data not shown), indicating that Fab LE2E9 fragment had a lower affinity for fVIII than native antibody. Accordingly, the higher concentrations of LE2E9 Fab than of native antibody required to inhibit fVIII binding to vWf can be attributed to a reduced affinity of LE2E9 Fab fragments for fVIII.
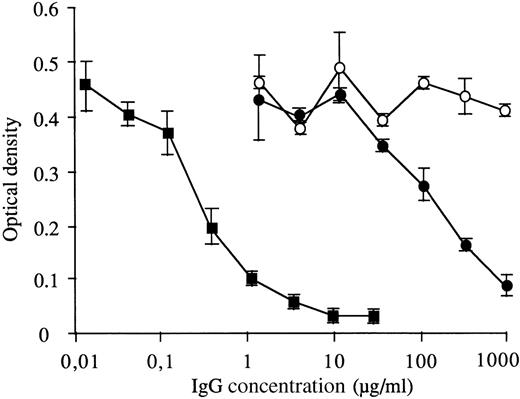
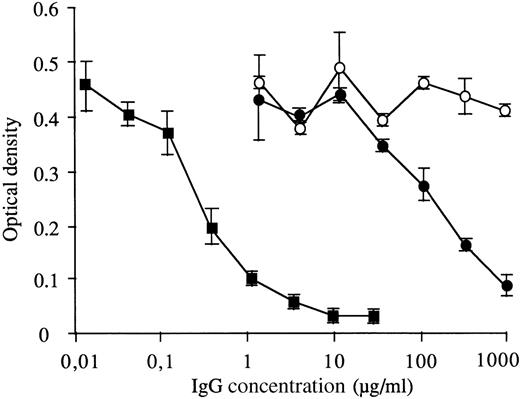
LE2E9 binding to fVIII is inhibited by LE IgG
To determine whether LE2E9 was representative of LE antibodies, a competitive assay was used. The binding of biotin-labeled LE2E9 to insolubilized fVIII was measured in the presence of increasing concentrations of either LE2E9, polyclonal LE IgG, or control polyclonal IgG. Polyclonal LE IgG dose-dependently inhibited LE2E9 binding to fVIII. The concentrations of LE2E9 or LE IgG inhibiting 50% of the binding of biotin-labeled LE2E9 to fVIII were 0.3 μg/mL and 170 μg/mL, respectively, whereas no inhibition was observed with control IgG (Figure 8).
Inhibition of LE2E9 binding to fVIII by LE IgG.
Biotin-labeled LE2E9 at 0.5 μg/ml was mixed with different concentrations of LE2E9 (▪), LE IgG (■), or control polyclonal IgG (○) before addition to fVIII-coated plates. The plates were then incubated for 2 hours at RT and the binding of biotin-labeled LE2E9 was detected by addition of HRP-labeled avidine. The mean and standard deviation of duplicates are indicated. Controls in the absence of fVIII gave OD490 lower than 0.05. The experiments were repeated 3 times with similar results.
Inhibition of LE2E9 binding to fVIII by LE IgG.
Biotin-labeled LE2E9 at 0.5 μg/ml was mixed with different concentrations of LE2E9 (▪), LE IgG (■), or control polyclonal IgG (○) before addition to fVIII-coated plates. The plates were then incubated for 2 hours at RT and the binding of biotin-labeled LE2E9 was detected by addition of HRP-labeled avidine. The mean and standard deviation of duplicates are indicated. Controls in the absence of fVIII gave OD490 lower than 0.05. The experiments were repeated 3 times with similar results.
Discussion
The development of a fVIII inhibitor in mild hemophilia A patients is a rare but severe complication of fVIII substitution therapy, which is typically associated with the shift of the patient's bleeding phenotype to that of severe hemophilia.13 Given the complexity inherent to the study of polyclonal anti-fVIII antibodies, we have analyzed at the clonal level the immune response of a mild hemophilia A patient (Arg2150His) who presented with a high titer inhibitor toward allogeneic but not self-fVIII.15 A human IgG4κ monoclonal antibody, LE2E9, was produced and characterized. The major features of LE2E9 were (i) partial (type 2) inhibition of wild-type fVIII activity in functional assays; (ii) complete inhibition of fVIII binding to vWf; (iii) absence of inhibition of fVIII of mild hemophilia A patients with mutation Arg2150His in the C1 domain; and (iv) binding to wild-type fVIII C1 domain.
Although a mutation in the fVIII gene is likely to alter the antigenicity of the molecule, so far there have been few reports establishing a relationship between the mutation and the specificity of patients' antibodies. One study failed to establish such a relationship for the Arg593Cys substitution in the fVIII gene.27 A recent report described another mild hemophilia A patient with an identical substitution and producing inhibitor antibodies that recognized specifically allogeneic fVIII but not self-fVIII; in this patient the inhibitor titer was, however, lower than 2 BU/mL and the restricted antibody specificity was observed only after a period of several years with no fVIII administration.14 Two patients with substitution Arg2150His also developed high titer immune response toward fVIII while conserving a residual fVIII activity, indicating that the inhibitory antibodies had a specificity restricted to normal fVIII.28
The mild hemophilia A patient from whom LE2E9 was derived carries the mutation Arg2150-> His and developed a high titer inhibitor (305 BU) after fVIII administration, while maintaining unchanged fVIII levels. The inhibitor antibodies of this patient did not alter fVIII activity of patient LE's brother, suggesting that antibody specificity was restricted to wild-type fVIII.15 Like patient LE's antibodies, LE2E9 did not inhibit fVIII Arg2150His. Capture experiments were performed to exclude that LE2E9 bound to Arg2150His fVIII without inhibiting its activity. Further, the absence of inhibition was not due to the presence of anti-idiotypic antibodies17,18,29 or to interaction with plasma protein, such as vWf,30 31 because pdfVIII added to the patient's plasma was inhibited by LE2E9, as well as pdfVIII in a control plasma.
Patient LE's polyclonal antibodies inhibited fVIII activity 10-fold better in the presence of vWf than in its absence.15 This observation could be accounted for by an increase of the inhibitory activity of the antibodies in the presence of vWf, or alternatively by the presence of different types of inhibitor antibodies, one relying on vWf to inhibit fVIII activity, the other not. Two types of antibodies could be identified among the patient polyclonal antibody population. One type of LE antibodies recognized fVIII complexed to vWf, whereas the other recognized isolated fVIII.32 The observation that LE2E9 inhibited rfVIII in the absence, as well as in the presence of vWf, confirms that the patient's antibodies comprised at least 2 types of inhibitory antibodies, one of which being able to inhibit fVIII in the absence of vWf. Further evidence that antibodies similar to LE2E9 were present in LE plasma was provided by the observation that LE IgG inhibited LE2E9 binding to fVIII. However, it is not known to what extend the patient's inhibitor titer is due to antibodies with LE2E9 specificity.
LE polyclonal antibodies bound a recombinant fVIII fragment corresponding to the A3C1 domain, although it was not directly demonstrated that such antibodies were inhibitory.15Whether inhibitor antibodies recognized the isolated C1 domain remained unsolved too, as our attempts to produce recombinant fragments corresponding to the C1 domain were unsuccessful in eukaryotic cells because synthesized fragments were not secreted (unpublished data, 1997). Epitope mapping was therefore performed with recombinant fragments produced in reticulocyte lysate, a procedure previously shown to be successful to evaluate antibodies directed toward the A3 domain.33 The epitope recognized by LE2E9 is conformational as no binding to fVIII was observed in Western blotting. We therefore used an immunoprecipitation assay in which LE2E9 recognized the C1 domain of the fVIII molecule.
LE2E9 behaves as a type 2 inhibitor, characterized by incomplete fVIII inactivation, even in large excess of antibody. So far, partial inactivation of fVIII by type 2 inhibitor antibodies has been attributed to the interaction of fVIII with vWf. Gawryl and Hoyer30 demonstrated that some type 2 inhibitors competed with vWf for binding to fVIII. Conversely, vWf is required to allow certain type 2 inhibitor antibodies to exert their activity, by reducing the rate of dissociation of activated fVIII from vWf.15 In contrast, LE2E9 inhibited fVIII effectively in the absence of vWf. Similar levels of inhibition of fVIII activity by LE2E9 were reached for rfVIII or pdfVIII, indicating that vWf did not protect fVIII from inactivation. LE2E9 represents therefore a novel form of type 2 inhibitor. The mechanism of fVIII inactivation by LE2E9 is currently being investigated. Preliminary experiments indicated that LE2E9 reduced the binding of activated fVIII to phosphatidylserine. The latter inhibition remained incomplete, even in the presence of a large excess of LE2E9 (unpublished data, 1997), in agreement with the type 2 inhibitor pattern of LE2E9.
In contrast to the partial inhibition of fVIII activity in functional assay, the inhibition of fVIII binding to vWf is complete at concentrations of LE2E9 in slight excess to those of fVIII. LE2E9 Fab fragments also inhibited fVIII binding to vWf, although, in agreement with the lower affinity of Fab fragments for fVIII, 15-fold higher concentrations of Fab fragments than of native antibody were required to achieve the same percentage of inhibition. Binding of fVIII to vWf is attributed to 2 fVIII regions: the carboxy-terminal part of the C2 domain and the acidic part of the A3 domain.3,34-36 It was therefore unexpected that LE2E9, which recognizes an epitope in the C1 domain, could interfere with fVIII binding to vWf. However, it is still unknown whether the epitope recognized by LE2E9 is directly involved in fVIII binding to vWf or whether LE2E9 reduces the interactions of fVIII with vWf by steric hindrance. Alternatively, the binding of LE2E9 to fVIII may alter the configuration of other fVIII light chain region(s) involved in fVIII binding to vWf, resulting in a reduced ability to bind to vWf. The latter hypothesis is, however, less likely because LE2E9 did not inhibit the binding of the human monoclonal antibody, BO2C11, which also inhibits fVIII binding to vWf but recognizes a conformational determinant, requiring the association of the amino- and carboxy-terminal part of the C2 domain (19 and unpublished data, 1998). The inhibition of fVIII binding to vWf by LE2E9 is in agreement with recent observations suggesting that residue Arg2150 in the C1 domain could directly or indirectly contribute to fVIII binding to vWf. Indeed, when plasma vWf/fVIII complexes were captured on a Sepharose column coated with an anti-vWf monoclonal antibody, the fraction of fVIII remaining bound to the column was significantly lower with Arg2150His fVIII than with normal fVIII (77% and > 90%, respectively).32 This reduced binding to vWf is due, at least in part, to a higher dissociation rate of the fVIII/vWf complex for Arg2150His fVIII than for normal fVIII.32
Alteration of fVIII metabolism and/or function due to the substitution Arg2150His is associated with alteration of the C1 domain antigenicity as indicated by the absence of inhibition of fVIII Arg2150His by the human monoclonal antibody LE2E9, specific for the fVIII C1 domain. These observations identify the fVIII C1 domain as a novel target for fVIII inhibitors and suggest that alteration of B-cell epitope(s) may contribute to the higher incidence of inhibitors found in mild/moderate hemophilia A patients with mutations in the carboxy-terminal end of the fVIII C1 domain.13
Acknowledgments
We thank J. Arnout and M. Vanrusselt for performing the coagulation assays, J. M. Lavergne for identification of mutations in the fVIII gene, and J.-J. Pin, S. Lebecque, and J. Banchereau for their invaluable help in the production of the human monoclonal antibodies.
Supported in part by research grant G .0292.98 of the Flemish Research Foundation, by grant BR1/4-255/138 of the Institut pour l'Encouragement de la Recherche Scientifique dans l'Industrie et l'Agriculture, and by grant Schw 752/1-1 from the Deutsche Forschungsgemeinschaft. J. Vermylen is holder of the Dr Jean Choay Chair for Hemostasis Research.
Reprints:Marc Jacquemin, Center for Molecular and Vascular Biology, Katholieke Universiteit Leuven, Campus Gasthuisberg, O&N, Herestraat 49, B-3000 Leuven, Belgium.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

![Fig. 3. Immunoprecipitation of wild-type and mutated rfVIII light chain. / Recombinant fVIII fragments labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 (LE) bound to Protein A Sepharose. After washing, bound material was eluted by SDS-buffer and analyzed by SDS-PAGE, followed by autoradiography. Controls included a human monoclonal antibody, BO2C11 (BO), directed toward the fVIII C2 domain,19 a rabbit polyclonal IgG antibody (aA3), directed toward amino acid residues 1797-1815 of the fVIII A3 domain and normal donor polyclonal IgG antibodies (Wi). The experiments were repeated 3 times with similar results.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/1/10.1182_blood.v95.1.156/5/m_bloo00150003w.jpeg?Expires=1768082495&Signature=ZRDxDGrwzo4AHHj6miRB2FR7ePhRwtFWYfomdnbrc2f4~fKww4NvLNZgostAdfEYhP7f8yNCekDqYkSEO5sgqcED8ioAn~AvXqFGbZTvAmA6-vNGkiJ1LtnVXSIbxq~tRhwAsDoW15XM8V17A-s7acjY364TZhAuypU0kfpu19DVK8uTwOfqmriz4cYOFiKXNNJnlfIKRUvSQR9PZy7m5tVIGakkPwsTCv-5YjR~-EsEyiGCfcHbzi~ELe9Vp~5tqPBlNw3ag52F7~NDH07juLwC5lrdMb0dr94eTFUFhcowmmZHWIa3DF1IthibMzE9fntK5OEkhuccok5LgLK9dw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 4. Epitope mapping of LE2E9. / (A) Structure of circulating fVIII. Each domain of fVIII is identified by a letter in upper case followed by a numeral. The small acidic regions are indicated by a1, a2, and a3, respectively. The copper ion involved in the non-covalent association of the A1 and A3 domains is indicated. (B) Recombinant fVIII fragments labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 bound to Protein A Sepharose. After washing, bound material was eluted and analyzed by SDS-PAGE, followed by autoradiography. Recombinant fVIII fragments are indicated by open bars. The amino- and carboxy-terminal extremities of fragments are as indicated. Control experiments were carried out with a human monoclonal antibody, BO2C11, directed toward the fVIII C2 domain19 and a rabbit polyclonal IgG antibody, aA3, directed toward amino acid residues 1797-1815 of the fVIII A3 domain The experiments were repeated at least 3 times with comparable results.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/1/10.1182_blood.v95.1.156/5/m_bloo00150004x.jpeg?Expires=1768082495&Signature=BgIUeWN1tdE46Me7pmae9JwJosvkiyw0N4N7~XkpdVumJ2xK8QXyUJnNGMJSLtlWCv06PtZDzxP6pOCMKoUTAlqQVUi3kgKF-VK-OcYYa0Desh7QTusoNMngOaMkNSrdK3ML65I99Pgddn17tAgybMVNHsI6KiWS7LE2GOUDa3Dn10CONGXF1hzUUb1UYHKtd7p38l-chtduQLurwQTd3TQMHwzRW-6m6Bt-fPGxkdynzwZo36N46hZ0JEkikIysC12lSBr8sW7IfWETvDAs5TkBoXlgT4fZ6nQO4NRGJakAfmH80O~JGWIXYbHZp0k9KsLGK21B2YuM~uZWrjnGGw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 5. Binding of LE2E9 to native or Arg2150His C1 and C1C2 domains. / Native and Arg2150His recombinant fVIII C1 domain (A) or C1C2 domains (B) labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 (LE) bound to Protein A Sepharose. After washing, bound material was eluted by SDS-buffer and analyzed by SDS-PAGE, followed by autoradiography. Controls included the human monoclonal antibody, BO2C11 (BO), and normal donor polyclonal IgG antibodies (Wi). The experiments were repeated 3 times with similar results.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/1/10.1182_blood.v95.1.156/5/m_bloo00150005w.jpeg?Expires=1768082495&Signature=gj2y7KJd34MNqjNXK8QtGR7-8vfT2xUZcuPT7aidtrmBFuUURQBMPzRdfrvqR9TS8VMEyeBS2Xk54WigbhARRfx06x6f2q~a5ZQz08o33LUrh0Ouzt9AaUcBYSFCdVurowtY39EpVgvb4XYm5hkZCgIOQdRo7sbNWnFZsIJPqkVcIs86As3W9aX--L8k8QtaLSpq45AIn3i0B-T3Q~hFzJ6z-2bzvxdz2bTgZYJm-wB7O8iD5MJ8ud-jdxdCQ8jgkSf6INI~PyzlF9AFhnNy4aqRo43N0Fi6-cFf7wl2~1du4uRlLVx9yAHiVQgB7IGJ1GgJ3Wvtr5pFx0C4Hlojng__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Fig. 3. Immunoprecipitation of wild-type and mutated rfVIII light chain. / Recombinant fVIII fragments labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 (LE) bound to Protein A Sepharose. After washing, bound material was eluted by SDS-buffer and analyzed by SDS-PAGE, followed by autoradiography. Controls included a human monoclonal antibody, BO2C11 (BO), directed toward the fVIII C2 domain,19 a rabbit polyclonal IgG antibody (aA3), directed toward amino acid residues 1797-1815 of the fVIII A3 domain and normal donor polyclonal IgG antibodies (Wi). The experiments were repeated 3 times with similar results.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/1/10.1182_blood.v95.1.156/5/m_bloo00150003w.jpeg?Expires=1768120090&Signature=bVH19Aj6oXyHyPR6W3JAEeF6YMnnxnjFSz2w8s1iMhrHpyKSqRCr52DT83Bj-nBj8d7fQy7EIbxTKE~4v0HFFVYTX3wOlEsvb7TtdG9PzTujT6TRnzKdZkvd0Y~PBUKOrojPUJkhrNJbxHw4oXpW7dB0oD6Hat3JU5wqkp7MTZ~lPquxugCdwIULml8zvNXB9KH8NkOakt2wvwCEEhm6EjeQxsEpfOXFYVg7EgKiVcTa49u3xzuVlYtp-1a0VJHE2bP8EnrSUhKtb65TUIASluBfQRiaBzlzU9HS9kC17r8b46OLIWsOnHCz6WeOv7IU8tj1LbyJm4q26FMjGCsDRw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 4. Epitope mapping of LE2E9. / (A) Structure of circulating fVIII. Each domain of fVIII is identified by a letter in upper case followed by a numeral. The small acidic regions are indicated by a1, a2, and a3, respectively. The copper ion involved in the non-covalent association of the A1 and A3 domains is indicated. (B) Recombinant fVIII fragments labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 bound to Protein A Sepharose. After washing, bound material was eluted and analyzed by SDS-PAGE, followed by autoradiography. Recombinant fVIII fragments are indicated by open bars. The amino- and carboxy-terminal extremities of fragments are as indicated. Control experiments were carried out with a human monoclonal antibody, BO2C11, directed toward the fVIII C2 domain19 and a rabbit polyclonal IgG antibody, aA3, directed toward amino acid residues 1797-1815 of the fVIII A3 domain The experiments were repeated at least 3 times with comparable results.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/1/10.1182_blood.v95.1.156/5/m_bloo00150004x.jpeg?Expires=1768120090&Signature=cqlo1G2Mmnq7GOIefv51vb8eIyh5~xtAARxTw92AioBRfWyF829tUra~GoOsEkYxp-osdBWdLzm-kVjX~5474lVGYucsm6wqBFAhd5mrA8~LxQbRY9djSPfqOMmaoeRsPUzfFytia1FBhb5narEqMJhLWVWQ4xvEQ6f~p8Fnagu1qbuExso3MYGavQru-HlitYtJ308kXOHDKjqiFBiyIeKn8C4q6dh2OwyvWMtINhU4Z3JL2FkgewaWWAocDCR2r51SKoU9w-r86c6gqsQzkDj459agiYTSo49fPIlg~aboCdU2ZPz2TPM~K5FKQS9bB0OI8Ut1VtG3likHCs17Yg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 5. Binding of LE2E9 to native or Arg2150His C1 and C1C2 domains. / Native and Arg2150His recombinant fVIII C1 domain (A) or C1C2 domains (B) labeled with [35S]methionine and expressed in reticulocyte lysates were incubated for 2 hours at 4°C with LE2E9 (LE) bound to Protein A Sepharose. After washing, bound material was eluted by SDS-buffer and analyzed by SDS-PAGE, followed by autoradiography. Controls included the human monoclonal antibody, BO2C11 (BO), and normal donor polyclonal IgG antibodies (Wi). The experiments were repeated 3 times with similar results.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/1/10.1182_blood.v95.1.156/5/m_bloo00150005w.jpeg?Expires=1768120090&Signature=ctyJ5Mz8GZUw9p0ul9NuI--9drUJwNY4ES2qfO~yHchP2nUXt4jiDlsNUFfLQ1x4E6OQ0c26Izq6w3sZCxc19cK~Drw1ayDKA3ijnKf8QHY6RlM0RzkHGauNmVX2McqpoYgK8asJKRDnWECbS4PkbbdKdYnDGpONvmUCSiWd0OYuNtFkF4m1DF4pCmZKlrSruTrhyszSdimADpiXoLn3hErromU0vBSb3XCFrQwjVrK8-oyaCyLlYQDRUJO738wDev7O2snZMx56LvEl5D9Ay81xylzpsGEvyrohMPZf61HXrIQ96DABYEj-OljmEMqLe1P9b57JnpkXp~DLy9s4yQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)