Abstract
Platelet retraction of a fibrin clot is mediated by the platelet fibrinogen receptor, IIbβ3. In certain forms of the inherited platelet disorder, Glanzmann thrombasthenia (GT), mutant IIbβ3 may interact normally with fibrin yet fail to support fibrinogen-dependent aggregation. We describe a patient (LD) with such a form of GT. Platelets from LD supported normal clot retraction but failed to bind fibrinogen. Platelet analysis using flow cytometry and immunoblotting showed reduced but clearly detectable IIbβ3, findings consistent with type II GT. Genotyping of LD revealed 2 novel β3 mutations: a deletion of nucleotides 867 to 868, resulting in a premature stop codon at amino acid residue 267, and a T883C missense mutation, resulting in a leucine (Leu) 262-to-proline (Pro) substitution. Leu262 is highly conserved among β integrin subunits and lies within an intrachain loop implicated in subunit association. Leu262Proβ3 cotransfected with wild-type IIb into COS-7 cells showed delayed intracellular maturation and reduced surface expression of easily dissociable complexes. In human embryonic kidney 293 cells, Leu262Proβ3 formed a complex with endogenous av and retracted fibrin clots similarly to wild-type β3. The same cells, however, were unable to bind immobilized fibrinogen. The molecular requirements for IIbβ3 to interact with fibrin compared with fibrinogen, therefore, appear to differ. The region surrounding β3 Leu262 may maintain β3 in a fibrinogen-binding, competent form, but it appears not to be required for receptor interactions with fibrin.
The aggregation of platelets and subsequent thrombus formation is mediated by the platelet-specific integrin αIIbβ3 (glycoprotein IIb-IIIa). Platelet αIIbβ3 is a heterodimeric surface receptor consisting of an alpha (αIIb) and a beta (β3) subunit in a noncovalent, cation-dependent complex.1 Platelet aggregation depends on αIIbβ3 binding of fibrinogen,2but the receptor can recognize other ligands, including fibronectin, von Willebrand factor (vWf), and vitronectin.3αIIbβ3 binding of soluble fibrinogen requires activation of the receptor by extracellular or intracellular events, a process that is poorly understood. A valuable tool for studying αIIbβ3 structure and function is the rare, autosomal recessive bleeding disorder Glanzmann thrombasthenia (GT), in which αIIbβ3 is dysfunctional or absent.4
GT mutations characterized at the molecular level are heterogenous and affect the αIIb and β3 genes equally.4,5 In many patients, gene deletions, frameshifts, and premature terminations result in αIIbβ3expression at less than 5% of normal levels (type I GT). Of more interest are cases in which a dysfunctional αIIbβ3 complex is present on the platelet surface at reduced (type II GT) or nearly normal (variant GT) levels. Type II and variant GT are predominantly due to point mutations of the β3 gene in 2 critical areas. First, mutations of the charged residues arginine (Arg) 119, Arg214, and Arg2164 in the β3 extracellular domain lead to the identification of a cation binding motif (DXSXS), which is critical for ligand binding and homologous to the metal ion-dependent adhesion site (MIDAS) of certain integrin α subunits.6,7 Second, mutations in the cytoplasmic domain of β3, such as Arg724Stop,8 result in a receptor that cannot be activated by intracellular signals (inside-out signaling) but still binds ligand in response to extracellular events. Therefore, thrombasthenic mutations can identify critical residues in αIIbβ3 that participate in ligand binding and receptor activation.
The molecular events involved in αIIbβ3ligand binding have been partly described; like many integrins, αIIbβ3 recognizes an Arg-glycine (Gly)-aspartic acid (Asp), or RGD, motif present in some adhesive ligands.3 One of these, fibrinogen, is an oligomeric complex of 3 paired subunits, the Aα, Bβ, and γ chains, and contains 4 RGD motifs, 2 in each Aα chain, at residues 95 to 97 and 572 to 574.9 In addition, a 12-amino acid motif, HHLGGAKQAGDV, comprising residues 400 to 411 of the γ chain, binds αIIbβ3 and competes with RGD for binding.10 Studies with fibrinogen mutants have shown that this C-terminal dodecapeptide is essential for fibrinogen-dependent platelet aggregation, whereas the Aα-chain RGD sequences are not required.11-13 Several research groups have attempted to localize the fibrinogen-binding site at the receptor level. Recombinant truncated extracellular domains of αIIb (residues 1-233) and β3 (residues 111-318) formed an RGD-binding complex.14 Cross-linking and peptide studies identified β3 residues 109 to 171 and 211 to 222 as potential fibrinogen-binding sites.15-17 These 2 regions include residues identified in GT or by mutagenesis6 as part of a MIDAS-like cation binding site in β3. In αIIb, the γ-chain peptide of fibrinogen was cross-linked to residues 294 to 314 of αIIb, suggesting that this is also a ligand-recognition site,18 and mutation of αIIb residues Gly184 to Gly193 was reported to abolish fibrinogen binding.19
The molecular interactions of αIIbβ3 with insoluble fibrin are less well understood. During clot retraction, activated platelets cause a marked reduction in the volume of a fibrin clot.20 Clot retraction can also be induced by nucleated cells21 and is integrin dependent.22 In particular, the β3 subunit is important in binding fibrin, triggering retraction through links between the cytoplasmic domain of β3 and cytoskeletal proteins.23 In cultured mammalian cell lines, β3, as part of the vitronectin receptor, αvβ3, induced spontaneous fibrin-clot retraction, whereas αIIbβ3 required prior activation of the integrin for retraction.24,25 In contrast to the situation with platelet aggregation, the C-terminal of the fibrinogen γ chain does not appear to be required for fibrin-clot retraction mediated by αIIbβ3,12 13 suggesting that fibrinogen and fibrin may bind to different sites on the receptor.
In the current study, we identified a novel β3 mutation, leucine (Leu) 262 to proline (Pro) (Leu262Pro), in a patient with type II GT whose platelets showed normal clot retraction. This mutation is predicted to alter the conformation of a region of β3located between 2 putative ligand-binding sites and involved in subunit interactions. By expressing Leu262Proβ3 in complex with αv in mammalian cells, we demonstrated that the mutant receptor binds fibrin in a similar manner to wild-type β3but does not recognize fibrinogen.
Patients and methods
Patient studies
Patient LD was a 3-year-old girl who presented postnatally with skin petechiae and ecchymoses. She had frequent bruising with minimal trauma and gum bleeding after tooth eruption. The patient's mother had a history of menorrhagia but was found to have von Willebrand disease; her father had no history of abnormal bleeding. Laboratory testing of LD showed that she had a normal platelet count (360 × 109/L) and a prolonged bleeding time. Prothrombin time, partial thromboplastin time, factor VIII, vWF antigen, and ristocetin cofactor levels were also normal.
Clot retraction by platelets
Whole blood from patient LD, her parents, and healthy controls was anticoagulated with acid citrate dextrose A, and prostaglandin E1 (50 ng/mL) was added before centrifugation at 220g to separate platelet-rich plasma (PRP). PRP samples were diluted in homologous platelet-poor plasma to final platelet counts of 2.5, 1.25, and 0.6 × 108 platelets/mL and incubated in glass tubes for 5 minutes at 37°C. Clot formation was induced by calcium chloride (8 mmol/L final concentration), and samples were photographed after 1 hour of incubation at 37°C.
Antibodies
The αIIb-specific monoclonal antibody (mAb) Tab was a gift from Dr Rodger McEver (University of Oklahoma).26 The β3-specific mAb AP3 was described previously.27 The mAb AP1, which recognizes GPIb, and the mAb AP2, which binds to a complex-dependent epitope on αIIbβ3,28 were provided by Dr Robert R. Montgomery (Blood Research Institute, Blood Center of Southeastern Wisconsin, Milwaukee, WI). The mAb LM609, which recognizes the αvβ3 complex,29 was a gift from Dr David A. Cheresh (Scripps Institute, La Jolla, CA). The mAb P4C10 against human β1 integrin was obtained from GIBCO BRL (Gaithersburg, MD). Rabbit polyclonal anti-αIIb and anti-β3 antibodies were prepared at the Blood Research Institute by using standard procedures.
Flow-cytometric analysis of platelet membrane glycoproteins
PRP from patient and control samples was centrifuged at 500g, and the platelet pellet was washed and resuspended at 4 × 108 platelets/mL in RCD-EDTA buffer (108 mmol/L sodium chloride [NaCl], 38 mmol/L potassium chloride, 1.7 mmol/L sodium bicarbonate, 21.2 mmol/L sodium citrate, 27.8 mmol/L glucose, 1.1 mmol/L magnesium chloride-6H20 , and 2 mmol/L EDTA [pH 6.5]). For each analysis, 1 × 107platelets in RCD-EDTA buffer plus 0.2% (wt/vol) bovine serum albumin (BSA) were incubated with a mouse mAb at a final concentration of 20 μg/mL for 1 hour at room temperature. Samples were then washed in the same buffer and incubated with a 1:20 dilution of fluorescein isothiocyanate-conjugated–labeled goat-antimouse IgG (Jackson Immunoresearch Laboratories, West Grove, PA) for 30 minutes in the dark. The samples were washed again, diluted in RCD-EDTA buffer and analyzed on a fluorescence-activated cell-sorter scan flow cytometer (Becton Dickinson, Mountain View, CA).
Semiquantitative Western blot analysis of platelet glycoproteins
Platelet lysates were prepared by lysing washed platelets in 50 mmol/L Tris (pH 6.8), 1% (vol/vol) Triton X-100, 10 mmol/LN-ethylmaleimide, 2 mmol/L phenylmethylsulfonyl fluoride (PMSF), and 20 μmol/L leupeptin. After centrifugation at 1500g, the total protein concentration of the supernatants was measured by a bicinchoninic acid assay (Pierce, Rockford, IL). Comparable amounts of thrombasthenic and control total platelet protein were analyzed on an sodium dodecyl sulfate (SDS)–9% polyacrylamide gel under reducing conditions and transferred to a polyvinylidene fluoride (PVDF) membrane (Immobilon; Millipore, Bedford, MA). The membrane was incubated with a mixture of rabbit polyclonal antibodies directed against αIIb and β3 (both at a final concentration of 5 μg/mL), then detected with a 1:2000 dilution of alkaline phosphatase–conjugated goat-antirabbit IgG (Jackson Immunoresearch) and color development with the nitro blue tetrazolium–5-bromo-4-chloro-3-indolyl phosphate substrate pair (Sigma, St Louis, MO).
Polymerase chain reaction amplification of IIb and β3 fragments from genomic DNA
Genomic DNA was prepared from peripheral blood leukocytes and amplified by polymerase chain reaction (PCR) with Taq polymerase by using oligonucleotide primers from intronic flanking sequences of αIIb and β3. All exons of both genes were sequenced at least twice to exclude Taq errors. Exon 5 of β3 was amplified by using the sense primer 5′-CTCTACCAGTGACATGGCTGAA-3′ and the antisense primer 5′-CAAGCTGAAACGAGCCCTGCC-3′. The PCR protocol entailed 5 minutes of denaturation at 100°C and 3 minutes of annealing at 56°C before the addition of Taq polymerase, then 30 cycles each of a 1-minute extension at 72°C, 45 seconds of denaturation at 96°C, and 45 seconds of annealing at 56°C. PCR products were extracted from agarose gels and analyzed by direct cycle sequencing. To detect multiple alleles from the patient LD and her parents, PCR products were subcloned into a TA overhang vector, pCRII (Invitrogen, Carlsbad, CA), and individual clones were sequenced.
PCR-based cartridge mutagenesis of β3complementary DNA
Full-length complementary DNA (cDNA) encoding β3, mutated to delete an internal EcoRI cleavage site (a gift of Dr Gilbert C. White, University of North Carolina School of Medicine), was cloned into plasmid vector pBluescript SK (Stratagene, San Diego, CA). Overlap PCR was used to generate a fragment of β3containing the T883C mutation found in patient LD. Briefly, primers with a single nucleotide mismatch at nucleotide 883 (sense primer, 5′-GGACGGAAGGCCGGCAGGCATTGTC-3′, and antisense primer, 5′-GACAATGCCTGCCGGCCTTCCGTCC-3′) were paired with wild-type β3 cDNA primers (sense primer, nucleotides 332-349: 5′-CCAGGTCACTCAAGTCAG-3′; and antisense primer, nucleotides 1799-1771:5′-GCAGGTGTCAGTAC-GCGTGGTACAGTTGC-3′) to generate a 1467-base-pair (bp) cDNA fragment containing the T883C mutation. The mutated 332-1799 fragment was subcloned into pCRII and digested with the unique restriction enzymes NsiI and MluI, which produced a 966-bp mutated cartridge that was then ligated intoNsiI- and MluI-digested wild-type β3–pBluescript SK. Finally, the reconstituted T883C β3 was excised from pBluescript SK with EcoRI and cloned into the mammalian expression vector pCDNA3(Invitrogen). Sequence analysis of the T883C β3 construct was done to confirm the point mutation and proper insertion of the cartridge into the wild-type β3 cDNA.
Mammalian cell transfection
COS-7 cells were transfected with αIIb- and β3-containing expression vectors in the presence of diethylaminoethyl-dextran as described previously.30 After 48 to 60 hours of culture, transfected COS-7 cells were surface labeled with biotin or metabolically labeled with sulfur 35 (S35)–methionine, as described previously.30The labeled cells were then solubilized in lysis buffer (50 mmol/L Tris-hydrochloric acid [HCl] at pH 7.4, 150 mmol/L NaCl, 1% (vol/vol) Triton X-100, and 2 mmol/L PMSF) and mixed for 30 minutes at 4°C. The lysates were centrifuged at 1600g for 30 minutes at 4°C and the supernatants stored at −80°C. For stable cell transfections, wild-type- and Leu262Proβ3-pcDNA3 plasmids were introduced into human embryonal kidney 293 cells in the presence of cationic lipid (Lipofectamine; GIBCO BRL). Transfected cells were selected in media containing 0.7 mg/mL neomycin.
Pulse-chase metabolic labeling of COS-7 cells
Forty-eight hours after transfection, COS-7 cells were incubated for 30 minutes in Dulbecco modified Eagle medium (DMEM; Sigma) without methionine, then pulsed with 2.22 × 107Bq/10-cm plate of 35S-methionine (DuPont-NEN, Boston, MA) for 30 minutes at 37°C. After the pulse, the cells were washed 3 times with Dulbecco phosphate-buffered saline (D-PBS) containing 1 mg/mL cold methionine (Sigma). The chase was begun by incubating the cells in DMEM containing 1 mg/mL cold methionine for 1, 4, 8, and 22 hours at 37°C. Labeled cells were washed 5 times in D-PBS containing 1 mg/mL cold methionine and then solubilized as described above.
Immunoprecipitation analysis
Lysates were precleared by incubating with 1% (wt/vol) BSA, 10 μg of preimmune mouse IgG (Sigma), and 50 μL of a 50% slurry of protein A-Sepharose CL-4B (Pharmacia, Uppsala, Sweden) for 1 hour at room temperature with constant mixing. The beads were then separated by centrifugation at 1600g for 5 minutes, and the supernatant was incubated with 10 μg of mAb for 18 hours at 4°C, with mixing. Ten micrograms of rabbit antimouse IgG (DAKO, Carpinteria, CA) was added, and mixing was done for 1 hour at room temperature. Protein A-Sepharose (50 μL) was then added, and mixing continued for another hour at room temperature. The samples were then centrifuged at 1600g for 5 minutes and the supernatants discarded. The beads were washed 5 times in immunoprecipitation buffer (50 mmol/L Tris-HCl [pH 7.4], 150 mmol/L NaCl, and 1% (vol/vol) Triton X-100), added to 50 μL of 2 × reducing buffer (4% SDS, 10% β-mercaptoethanol, 100 mmol/L Tris-HCl [pH 6.8], 10% glycerol, and 0.001% bromophenol blue), and boiled for 10 minutes. Samples were centrifuged at 1600g for 5 minutes and the supernatants analyzed by SDS–polyacrylamide gel electrophoresis. Biotin-labeled samples were transferred to PVDF membrane and detected with horseradish peroxidase–streptavidin and chemiluminescence reagents as described previously.30 Gels containing35S-methionine–labeled samples were fixed in 45% methanol and 12% acetic acid for 30 minutes, incubated in Enlightening solution (DuPont-NEN) for 30 minutes, dried, and analyzed by autoradiography.
Clot retraction by 293 cells expressing avβ3
Chromatographically purified fibrinogen I (γAγA) was a gift of Dr Michael W. Mosesson (Sinai-Samaritan Medical Center, Milwaukee, WI). Plasma from healthy subjects was depleted of fibronectin by passage through a gelatin-Sepharose column (Sigma) as described previously.24 Preliminary experiments (data not shown) demonstrated that untransfected 293 cells showed moderate retraction of clotted plasma but were unable to retract clots formed from fibronectin-depleted plasma. Therefore, fibronectin-depleted plasma was used in retraction assays to minimize the contribution of endogenous αvβ1 and other fibronectin receptors. Cultured untransfected and transfected 293 cells were washed twice in D-PBS (Sigma), lifted with 0.01% (wt/vol) trypsin and 3.5 mmol/L EDTA, and washed twice again in D-PBS. The cells (10 × 106/mL) were then resuspended in modified Eagle medium containing Earle salts (MEM-ES; Sigma) and 0.1 mmol/LL-glutamine. For clot-retraction assays, 300 μL of the cell solution was added to 100 μL of medium containing 5 μg aprotinin (Sigma) and either 100 μL of fibronectin-depleted plasma or 100 μL of medium containing 100 μg of purified fibrinogen, in a 10- × 75-mm borosilicate glass tube (Fisher Scientific, Pittsburgh, PA). To initiate clot formation, 1 U of human α thrombin was added and the tubes were incubated at 37°C. The external dimensions of each clot were measured at 30-minute intervals, and a cylindrical model (volume = πradius2 × height) was used to calculate the approximate clot volume.
In some experiments, plasma or 293 cells were preincubated with peptides or mAbs for 15 minutes at 22°C. The peptides RGDW and RGEW and the fibrinogen peptide HHLGGAKQAGDV (H12), corresponding to γ-chain residues 400 to 411, were synthesized on a Pepsynthesizer (Model 9050; Millipore) with 9-fluoronylmethoxycarbonyl chemistry using standard manufacturers' procedures.
Cell adhesion to immobilized substrates
Adhesion of fluorescently labeled cells was preformed as described previously.8 Protein substrates or antibodies (2-10 μg/mL in D-PBS) were added to an Immulon 2 96-well plate (Dynatech, Chantilly, VA) and incubated overnight at 4°C. Before use, the coated plates were washed with D-PBS and blocked with 1% (wt/vol) BSA in D-PBS for 1 hour at 22°C. Transfected or control 293 cells were washed and trypsinized as described above, resuspended at 2 × 106 cells/mL in MEM-ES medium, and incubated with 2 μg/mL calcein AM (Molecular Probes, Eugene, OR) for 30 minutes at 37°C. After labeling, the cells were washed twice in D-PBS and resuspended in MEM-ES at 3 × 106/mL. One hundred microliters of labeled cell suspension was added to each well and allowed to adhere for 1 hour at 37°C. The total fluorescence per well was measured in a multiwell plate reader (Cytofluor; Perseptive Biosystems, Framingham, MA) immediately after incubation and 2 washes with MEM-ES to remove nonadherent cells.
Results
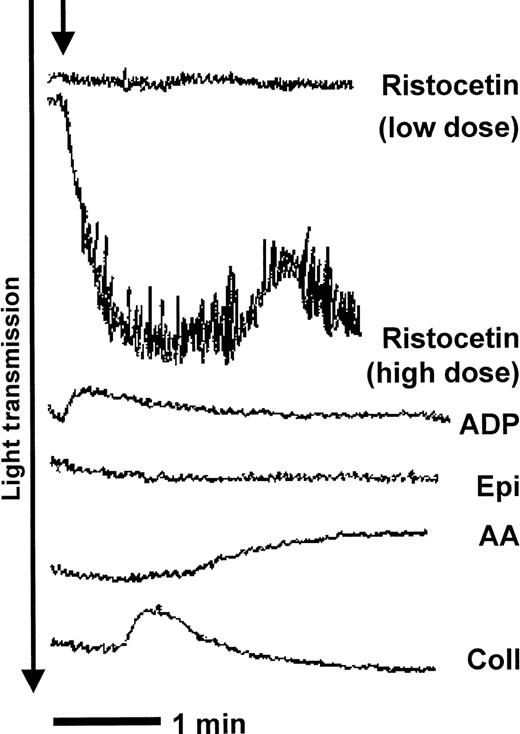
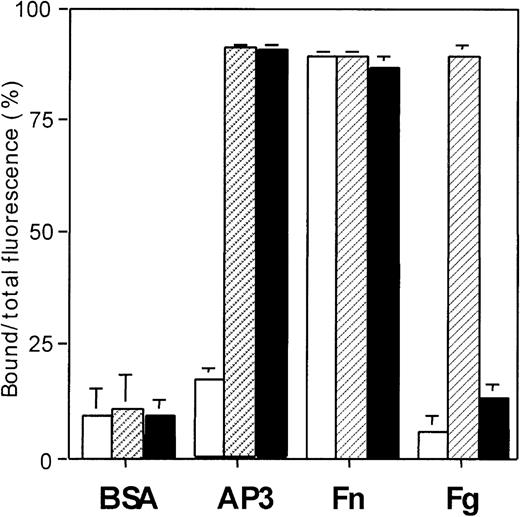
The clinical history of patient LD indicated a marked hemostatic defect. Platelets from the patient did not aggregate in response to adenosine diphosphate, epinephrine, or arachidonic acid and showed only shape change in response to collagen, but they agglutinated with ristocetin (Figure 1). The failure of the platelets to support fibrinogen-dependent aggregation suggests a defect in platelet αIIbβ3.
Platelets from the proband (LD) do not support fibrinogen-dependent platelet aggregation.
Platelet-rich plasma (PRP) from patient LD was stirred in an aggregometer at 37°C before the addition of agonists (time point indicated by arrow). Platelets from LD showed no aggregation in response to adenosine diphosphate (ADP), epinephrine (Epi), or arachidonic acid (AA) and showed shape change only in response to collagen (Coll). Platelets from LD agglutinated reversibly with high-dose ristocetin.
Platelets from the proband (LD) do not support fibrinogen-dependent platelet aggregation.
Platelet-rich plasma (PRP) from patient LD was stirred in an aggregometer at 37°C before the addition of agonists (time point indicated by arrow). Platelets from LD showed no aggregation in response to adenosine diphosphate (ADP), epinephrine (Epi), or arachidonic acid (AA) and showed shape change only in response to collagen (Coll). Platelets from LD agglutinated reversibly with high-dose ristocetin.
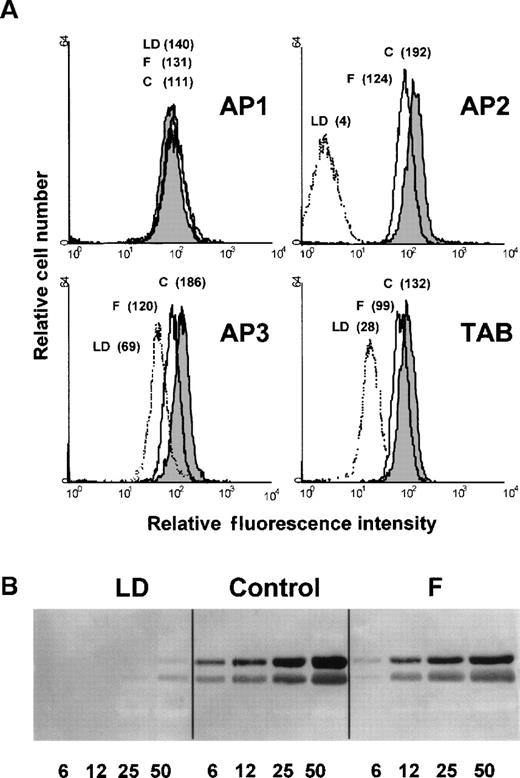
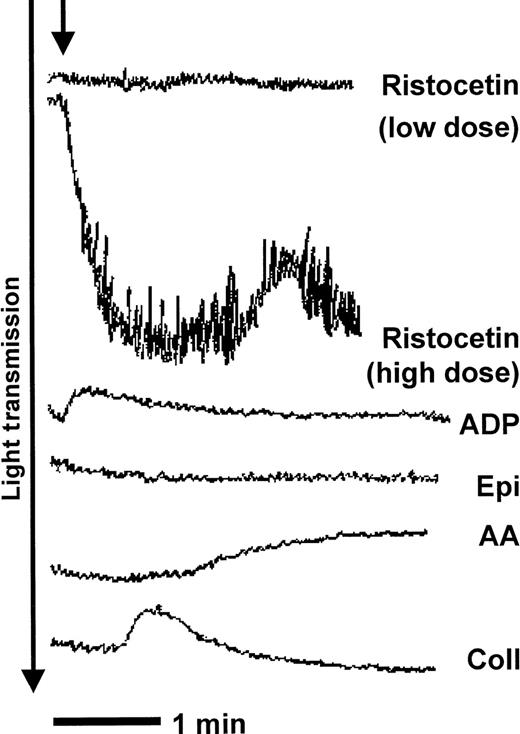
On flow cytometry (Figure 2A), platelets from LD showed reduced (30% of normal) binding of subunit-specific mAbs against αIIb or β3 but no binding of a complex-specific antibody (AP2). Total platelet levels of αIIbβ3 were assessed by semiquantitative immunoblotting of platelet lysates (Figure 2B). In lysates from LD, faint but detectable bands of the expected apparent molecular weight were seen, corresponding to approximately 10% of control levels. These findings are consistent with a diagnosis of Type II GT. In both assays, platelets from the proband's father showed reduced (50% of normal) levels of platelet αIIbβ3, findings consistent with a heterozygous defect that affects αIIbβ3 expression. No platelet samples from the patient's mother were available. The failure of platelets from LD to aggregate implies a defect in binding of soluble fibrinogen.
Platelets from LD express IIb and β3 subunits but little IIbβ3complex.
(A) Flow-cytometric analysis of surface αIIbβ3. Monoclonal antibodies directed against a control glycoprotein, GPIb (AP1), the αIIbβ3 complex (AP2), the β3subunit (AP3), or the αIIb subunit (TAB) were incubated with washed platelets from a healthy donor (control), the patient (LD), or the patient's father (F), and binding was assessed. Control platelet binding of nonimmune mouse IgG yielded a relative mean fluorescence of 2. (B) Western blot analysis of total platelet αIIbβ3. The indicated amounts of Triton X-100–treated platelet lysates from a healthy control, the patient (LD), and the patient's father (F) were separated by sodium dodecyl sulfate (SDS)–7% polyacrylamide gel electrophoresis, transferred to a polyvinylidene fluoride membrane, and detected with rabbit polyclonal antibodies against αIIb and β3. The positions of αIIb (upper arrow) and β3(lower arrow) are indicated.
Platelets from LD express IIb and β3 subunits but little IIbβ3complex.
(A) Flow-cytometric analysis of surface αIIbβ3. Monoclonal antibodies directed against a control glycoprotein, GPIb (AP1), the αIIbβ3 complex (AP2), the β3subunit (AP3), or the αIIb subunit (TAB) were incubated with washed platelets from a healthy donor (control), the patient (LD), or the patient's father (F), and binding was assessed. Control platelet binding of nonimmune mouse IgG yielded a relative mean fluorescence of 2. (B) Western blot analysis of total platelet αIIbβ3. The indicated amounts of Triton X-100–treated platelet lysates from a healthy control, the patient (LD), and the patient's father (F) were separated by sodium dodecyl sulfate (SDS)–7% polyacrylamide gel electrophoresis, transferred to a polyvinylidene fluoride membrane, and detected with rabbit polyclonal antibodies against αIIb and β3. The positions of αIIb (upper arrow) and β3(lower arrow) are indicated.
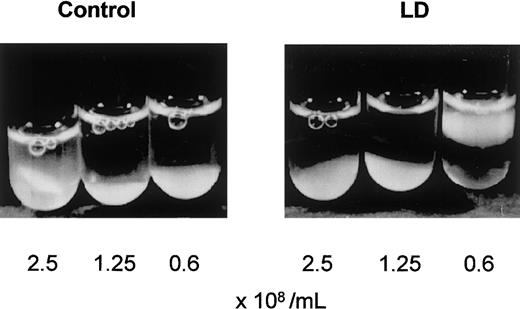
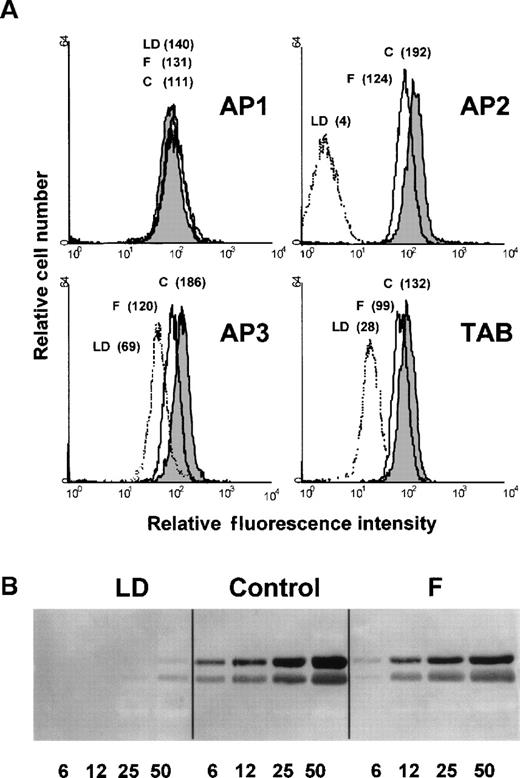
The ability of platelets from LD to interact with fibrin was assessed in a clot-retraction assay. Clotted PRP from LD (Figure3) and both parents (data not shown) retracted as strongly as control plasma, indicating that the defective platelet αIIbβ3 complex was still capable of interacting with fibrin.
Platelets from LD retract a fibrin clot.
PRP from a healthy control or patient LD was diluted with autologous plasma to the indicated platelet concentration and clotted by adding 8 mmol/L calcium chloride. After 1 hour of incubation at 37°C, clot retraction of platelets from LD was equivalent to that of control platelets.
Platelets from LD retract a fibrin clot.
PRP from a healthy control or patient LD was diluted with autologous plasma to the indicated platelet concentration and clotted by adding 8 mmol/L calcium chloride. After 1 hour of incubation at 37°C, clot retraction of platelets from LD was equivalent to that of control platelets.
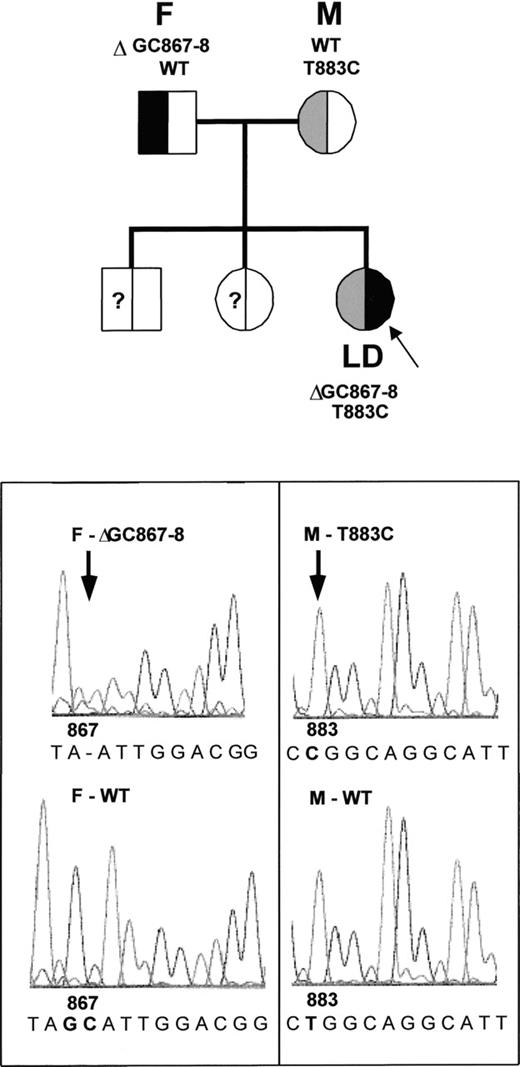
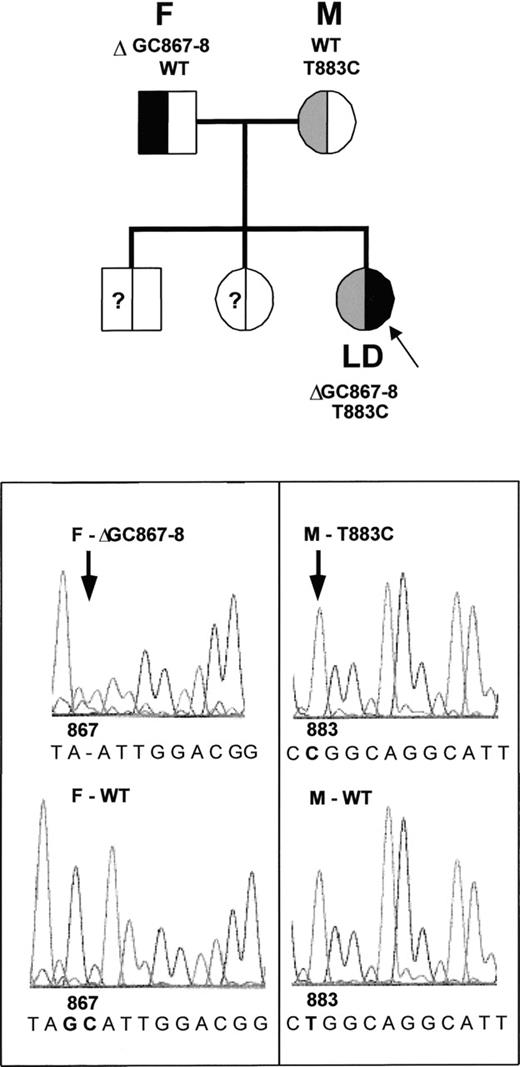
Genetic analysis of LD and her family (Figure4) demonstrated that LD was a compound heterozygote for 2 novel mutations of the β3 gene in exon 5. First, in both LD and her father, a dinucleotide deletion of bases GC867 to GC868 was found. This deletion is predicted to result in a frameshift and substitution of a premature stop codon for amino acid 267. Second, LD and her mother had a point mutation of T883C, which is predicted to cause the substitution of a Pro for Leu at position 262. Sequencing of both alleles by subcloning of PCR-amplified genomic DNA confirmed that each of LD's parents carried 1 wild-type and 1 mutant β3 allele, whereas LD had inherited both exon 5 mutations. No mutations were found in the αIIb gene of LD. The half-normal levels of αIIbβ3observed on platelets from LD's father (Figure 2) are consistent with failure to express the truncated D867-868 form of β3. This suggests that all the β3 present on platelets from LD carries the Leu262Pro mutation.
LD is a compound heterozygote for 2 mutations of the β3 gene.
Analysis of genomic DNA amplified by polymerase chain reaction identified a deletion of GC867-868 in LD's father (F) and a T883C substitution in her mother (M). Both mutant alleles were found in LD. The patient's siblings were not analyzed but are asymptomatic.
LD is a compound heterozygote for 2 mutations of the β3 gene.
Analysis of genomic DNA amplified by polymerase chain reaction identified a deletion of GC867-868 in LD's father (F) and a T883C substitution in her mother (M). Both mutant alleles were found in LD. The patient's siblings were not analyzed but are asymptomatic.
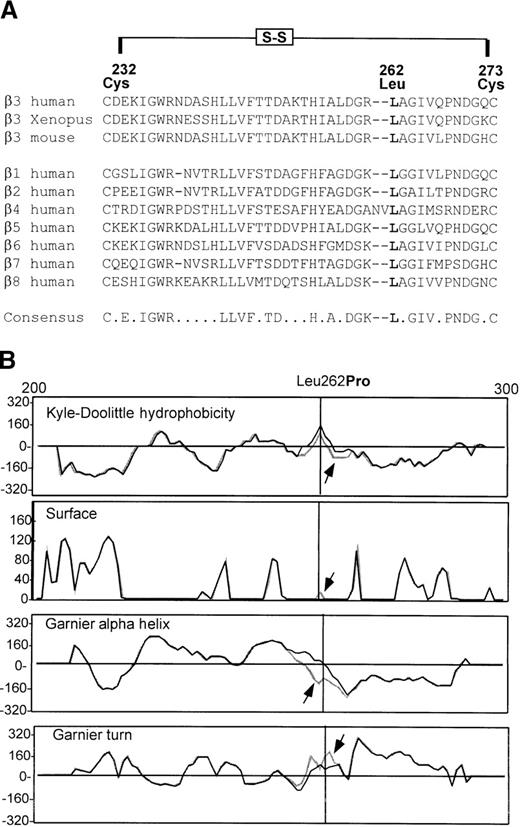
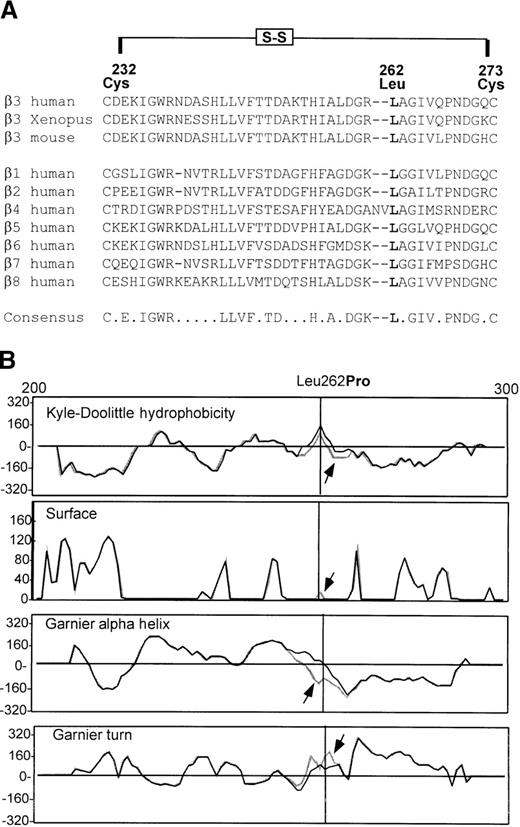
Comparison of the human β3 amino acid sequence with β3 subunits from other species and other human β integrin subunits showed that the position corresponding to β3 262 was always occupied by a Leu residue (Figure5A). The effect of a Leu262-to-Pro substitution on the predicted structure of β3 residues 200 to 300 was modeled by using a selection of protein structure algorithms (GeneWorks; Intelligenetics, Mountain View, CA). Compared with the wild type, the presence of a Pro at position 262 led to a reduction in hydrophobicity (by the Kyle-Doolittle hydrophobicity-scoring system), a reduced probability of an α helix but an increased probability of a β turn (by Garnier protein-structure analysis), and an increased probability of surface exposure (Figure 5B). Therefore, it is likely that the Pro262β3 mutant adopts a local conformation different from that of Leu262β3.
Structural analysis of the Leu262Proβ3mutation.
(A) Leucine (Leu) 262 is completely conserved among β subunits. The amino acid sequence of human β3 residues cystine (Cys) 232 to Cys273 is shown aligned with frog (Xenopus) and mouse β3 and with the sequences of 7 other human β subunits. Notably, the Leu residue at position 262 (in boldface) is invariant. The proposed intramolecular disulfide loop Cys232-27330is shown. (B) Predicted hydrophobicity and secondary structure are shown for β3 amino acids 200 to 300 containing either wild-type Leu262 (black line) or mutant Pro262 (stippled line with arrow). The position of amino acid 262 is indicated by the vertical line.
Structural analysis of the Leu262Proβ3mutation.
(A) Leucine (Leu) 262 is completely conserved among β subunits. The amino acid sequence of human β3 residues cystine (Cys) 232 to Cys273 is shown aligned with frog (Xenopus) and mouse β3 and with the sequences of 7 other human β subunits. Notably, the Leu residue at position 262 (in boldface) is invariant. The proposed intramolecular disulfide loop Cys232-27330is shown. (B) Predicted hydrophobicity and secondary structure are shown for β3 amino acids 200 to 300 containing either wild-type Leu262 (black line) or mutant Pro262 (stippled line with arrow). The position of amino acid 262 is indicated by the vertical line.
Mammalian cell-expression systems were used to confirm that the Leu262Pro form of αIIbβ3 showed altered function. Leu262Proβ3 cDNA was constructed and cotransfected with wild-type αIIb into COS-7 cells. Biotin surface labeling of these transiently transfected cells showed that the mutant complex was poorly expressed and less stable than the wild type: from a detergent lysate, the complex-specific antibody AP2 immunoprecipitated only trace amounts of αIIbLeu262Proβ3 (data not shown). The β3 subunit-specific antibody, AP3, precipitated both subunits from lysates of wild-type αIIbβ3transfected cells but only the β3 subunit from cells transfected with αIIbLeu262Proβ3 (data not shown), resultsconsistent with the idea that the αIIbLeu262Proβ3 complex is easily dissociable. The addition of 2 mmol/L calcium to αIIbLeu262Proβ3 lysates did not preserve subunit association. Similarly, the αIIb-specific antibody, Tab, captured only the αIIb subunit from lysates of cells transfected with the mutant receptor (data not shown). Thus, the surface expression of αIIbLeu262Proβ3 in COS-7 cells recapitulated the platelet phenotype, with both subunits detectable but little or no binding of a complex-specific antibody.
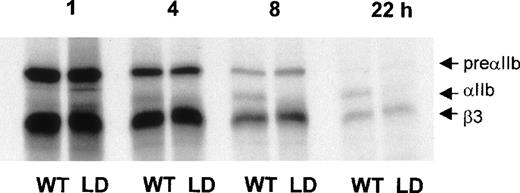
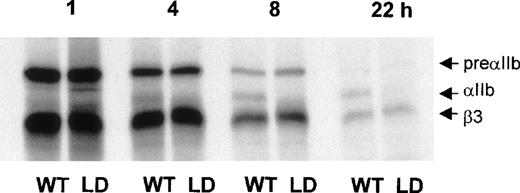
Metabolic labeling of transfected COS-7 cells with35S-methionine was used to assess the biosynthesis of αIIbLeu262Proβ3. Normal synthesis and expression of αIIbβ3 follows an ordered series of events31 32 in which cleavage of preαIIb to mature αIIb indicates that the nascent integrin complex has reached the Golgi and undergone posttranslational processing. Pulse-chase experiments were used to follow the intracellular maturation of αIIb and either wild-type β3 or Leu262Proβ3. As shown in Figure 6, immunoprecipitation of Leu262Proβ3 by an anti-β3 antibody captured preαIIb, indicating that the mutant subunit had formed a heterodimer in the endoplasmic reticulum (ER). There was no apparent defect in the extent or rate of Leu262Proβ3synthesis. However, the maturation of the mutant complex was markedly delayed. In cells expressing αIIbβ3, mature αIIb was observed within 4 hours of the methionine pulse and cleavage was virtually complete by 22 hours. In contrast, preαIIb associated with Leu262Proβ3 was not cleaved before 22 hours, a finding consistent with a defect in heterodimer export from the ER. These results provide a likely molecular explanation for the reduced expression of αIIbLeu262Proβ3 observed in platelets from LD.
Maturation of IIbLeu262Proβ3is delayed in COS-7 cells.
COS-7 cells transfected with wild-type (WT) αIIb and either WT β3 or Leu262Proβ3 (LD) were pulsed with sulfur 35–methionine for 30 minutes and chased for up to 22 hours with medium containing 1 mg/mL cold methionine. Cell lysates prepared at the indicated times were immunoprecipitated with an anti-β3 antibody (AP3) and analyzed by autoradiography of an SDS–7% polyacrylamide gel run under reducing conditions. Although preαIIb and Leu262Proβ3 synthesis and association are normal in lysates from LD, the appearance of a mature αIIbLeu262Proβ3 complex is markedly delayed.
Maturation of IIbLeu262Proβ3is delayed in COS-7 cells.
COS-7 cells transfected with wild-type (WT) αIIb and either WT β3 or Leu262Proβ3 (LD) were pulsed with sulfur 35–methionine for 30 minutes and chased for up to 22 hours with medium containing 1 mg/mL cold methionine. Cell lysates prepared at the indicated times were immunoprecipitated with an anti-β3 antibody (AP3) and analyzed by autoradiography of an SDS–7% polyacrylamide gel run under reducing conditions. Although preαIIb and Leu262Proβ3 synthesis and association are normal in lysates from LD, the appearance of a mature αIIbLeu262Proβ3 complex is markedly delayed.
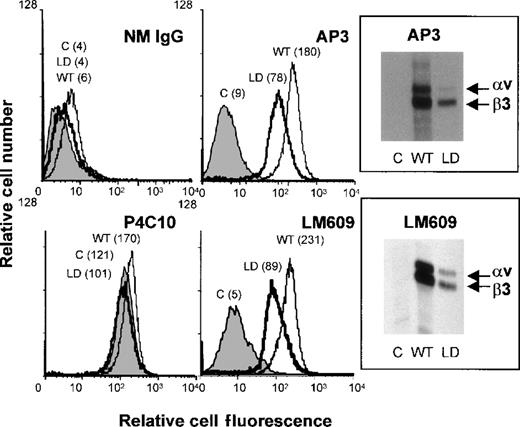
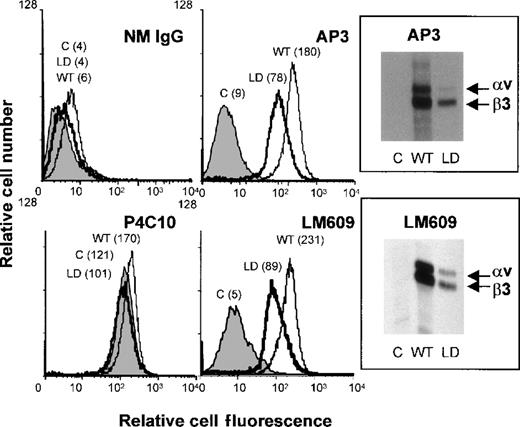
To study the effect of the Leu262Proβ3 on ligand binding and specificity, the mutant β3 subunit alone was stably expressed in human embryonal kidney 293 cells. Previous studies using this cell line23 showed that transfected β3is expressed on the cell surface in a complex with endogenous αv and can mediate fibrin-clot retraction. A further advantage of this system is that αvβ3, unlike transfected αIIbβ3, does not require activation to bind ligand.24 The expression of αv-Leu262Proβ3 in 293 cells was assessed by flow cytometry and biotin surface labeling. As shown in Figure7, the mutant complex was expressed less effectively than wild-type αvβ3 (40%-50% levels), as expected, but intact heterodimer was detected on the cell surface by both AP3 and the complex-specific antibody, LM609.
Leu262Proβ3 is expressed in a complex with αv in 293 cells.
Untransfected (C) 293 cells or cells stably transfected with WT β3 or Leu262Proβ3 (LD) were analyzed by flow cytometry. The mean fluorescence for each cell line is shown. The 2 left-hand panels show binding of a negative-control antibody (nonimmune mouse IgG) and a positive-control antibody (polyclonal anti-β1). The 2 right-hand panels show the results of flow cytometry and immunoprecipitation of biotin surface-labeled cells with antibodies against β3 (AP3) or the αvβ3complex (LM609). The positions of αv and β3are indicated.
Leu262Proβ3 is expressed in a complex with αv in 293 cells.
Untransfected (C) 293 cells or cells stably transfected with WT β3 or Leu262Proβ3 (LD) were analyzed by flow cytometry. The mean fluorescence for each cell line is shown. The 2 left-hand panels show binding of a negative-control antibody (nonimmune mouse IgG) and a positive-control antibody (polyclonal anti-β1). The 2 right-hand panels show the results of flow cytometry and immunoprecipitation of biotin surface-labeled cells with antibodies against β3 (AP3) or the αvβ3complex (LM609). The positions of αv and β3are indicated.
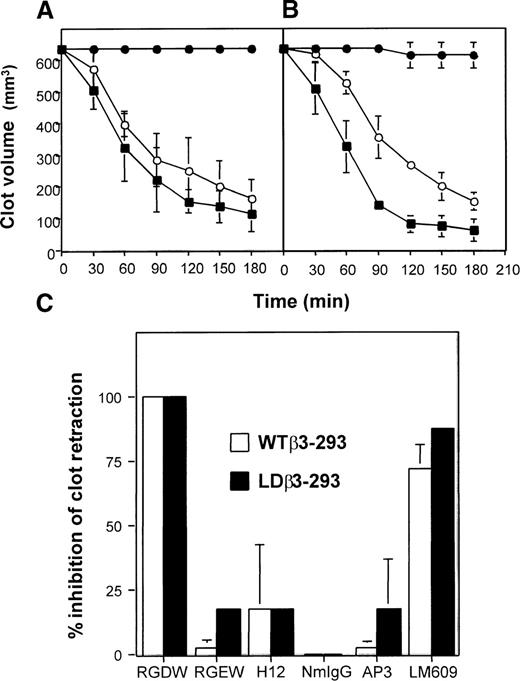
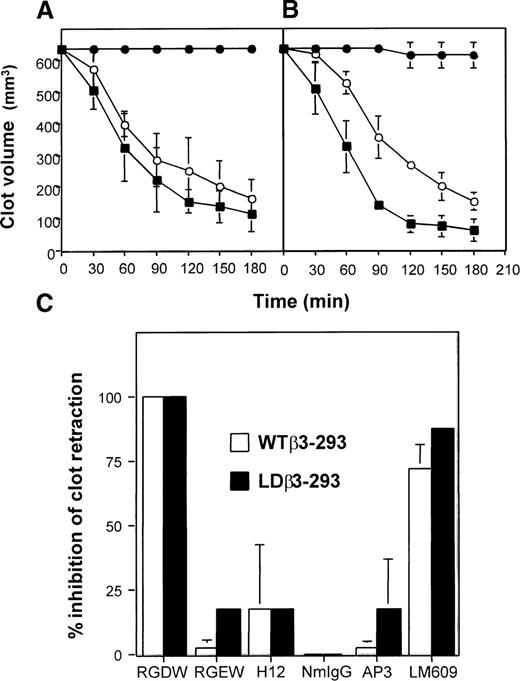
The ability of αvLeu262Proβ3 cells to retract a fibrin clot was compared with that of untransfected and αvβ3 cells (Figure8). Wild-type αvβ3 cells mediated rapid retraction of fibrin clots from both fibronectin-depleted plasma (Figure 8A) and purified fibrinogen (Figure 8B). Despite the reduced receptor density on their surface, αvLeu262Proβ3 cells showed nearly normal retraction of fibrin clots (Figure 8). In both αvβ3 and αvLeu262Proβ3 cells, retraction could be enhanced by 0.5-mmol/L Mn2+ and inhibited by EDTA or ethylene glycol tetraacetic acid (data not shown), inhibited by RGDW but not by RGEW or fibrinogen γ-chain peptides, and inhibited by the complex-specific antibody, LM609 (Figure 8C). This suggests that a similar, cation-dependent mechanism underlies the interaction of both the wild-type and mutant integrin complex with an RGD-like site on fibrin.
vLeu262Proβ3 on 293 cells retracts a fibrin clot.
Untransfected 293 cells (solid circles) and cells expressing WT αvβ3 (solid squares) or αvLeu262Proβ3 (open circles) were assessed for their ability to retract clotted fibronectin-depleted plasma (A) or purified fibrinogen (B). The estimated clot volume is expressed as a function of time (minutes). The data shown are representative results from 3 separate experiments. αvLeu262Proβ3-mediated clot retraction was comparable to that of WT αvβ3. (C) WT αvβ3 cells (open columns) or αvLeu262Proβ3 cells (solid columns) were incubated for 15 minutes at 22°C with peptides RGDW, RGEW, or H12 (all at a final concentration of 2 mmol/L) or with the indicated antibodies (final concentration, 10 μg/mL). Only RGDW and the αvβ3-specific antibody LM609 fully inhibited clot retraction.
vLeu262Proβ3 on 293 cells retracts a fibrin clot.
Untransfected 293 cells (solid circles) and cells expressing WT αvβ3 (solid squares) or αvLeu262Proβ3 (open circles) were assessed for their ability to retract clotted fibronectin-depleted plasma (A) or purified fibrinogen (B). The estimated clot volume is expressed as a function of time (minutes). The data shown are representative results from 3 separate experiments. αvLeu262Proβ3-mediated clot retraction was comparable to that of WT αvβ3. (C) WT αvβ3 cells (open columns) or αvLeu262Proβ3 cells (solid columns) were incubated for 15 minutes at 22°C with peptides RGDW, RGEW, or H12 (all at a final concentration of 2 mmol/L) or with the indicated antibodies (final concentration, 10 μg/mL). Only RGDW and the αvβ3-specific antibody LM609 fully inhibited clot retraction.
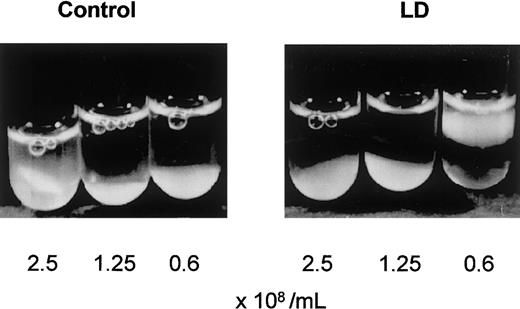
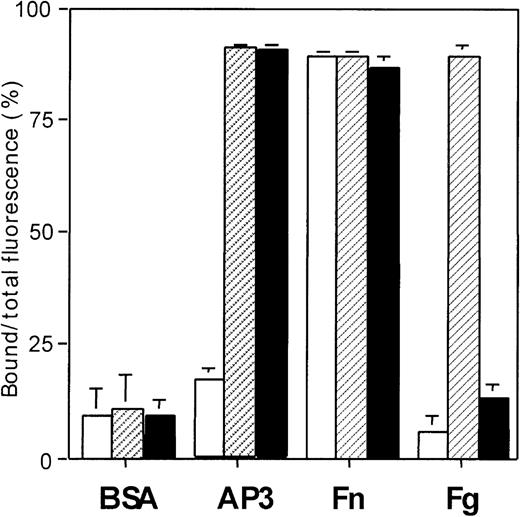
Finally, transfected 293 cells were assessed for their ability to bind purified fibrinogen and other ligands immobilized in a 96-well microtiter plate (Figure 9). Untransfected cells and β3-transfected lines bound equally to the control ligand fibronectin, suggesting a primary role for αvβ1 and other endogenous integrins. The degree of cell spreading on fibronectin after adhesion was similar for all cell lines. Similarly, all 293 cell lines adhered to immobilized vitronectin (data not shown). As expected, both β3-transfected cell lines, but not untransfected cells, bound to a β3-specific antibody, AP3. However, whereas wild-type αvβ3 cells showed significant adhesion and spreading on immobilized fibrinogen, the αvLeu262Proβ3 complex was unable to interact with immobilized fibrinogen. Therefore, the expression of a αvLeu262Proβ3 mutation in a cultured cell line recapitulated the ligand-binding specificity of αIIbLeu262Proβ3 on platelets in that it was unable to bind fibrinogen but showed nearly normal binding and retraction of a fibrin gel.
vLeu262Proβ3 does not support cell adhesion to immobilized fibrinogen.
Untransfected 293 cells (open columns) and cells expressing WT αvβ3 (hatched columns) or αvLeu262Proβ3 (solid columns) were labeled with calcein am and allowed to adhere to immobilized substrates (bovine serum albumin, AP3, fibronectin, or fibrinogen) for 1 hour at 37°C. Adhesion is shown as the ratio of fluorescence per well before and after washing. Each column represents the mean (± SD) value from triplicate samples, and the results are representative of 4 separate experiments.
vLeu262Proβ3 does not support cell adhesion to immobilized fibrinogen.
Untransfected 293 cells (open columns) and cells expressing WT αvβ3 (hatched columns) or αvLeu262Proβ3 (solid columns) were labeled with calcein am and allowed to adhere to immobilized substrates (bovine serum albumin, AP3, fibronectin, or fibrinogen) for 1 hour at 37°C. Adhesion is shown as the ratio of fluorescence per well before and after washing. Each column represents the mean (± SD) value from triplicate samples, and the results are representative of 4 separate experiments.
Discussion
In this study, we characterized the molecular defects responsible for a novel case of GT. The patient's history and the absence of platelet aggregation in response to multiple agonists allowed the clinical diagnosis of GT. On the basis of our detection by flow cytometry and immunoblotting of platelet αIIbβ3levels that were 5% to 30% of normal values, we found this patient to have type II thrombasthenia. Although flow data with subunit-specific mAbs showed surface expression to be 30% of normal levels, there was no binding of the complex-specific mAb, AP2 (Figure 2A). This indicates that either the conformation of the mutant complex is abnormal or that the complex itself is unstable after surface expression. Such an unstable complex was described previously in another β3 point mutation (serine 162 to Leu), in which dissociation of the mutant αIIbβ3complex was demonstrated by abnormal migration through a sucrose gradient.33
Genotypic analysis of the patient's family identified 2 novel mutations of β3 only 16 bases apart in exon 5. The first was a dinucleotide deletion of bases 867 to 868 that resulted in a frameshift and substitution of a termination codon for amino acid residue 267. The 867-868 deletion was found in both the patient and her father and is predicted to result in the synthesis of a severely truncated form of β3 encoding only residues 1 to 267. The father's phenotype, with levels of platelet αIIbβ3 that were 50% of normal values, suggests that this truncation mutant interferes significantly with receptor expression. Several truncation mutants affecting the β3 subunits were previously described in patients with GT.34-36 In all these cases, the truncated subunit failed to be expressed, thereby conferring a type I GT phenotype. In vitro studies with truncated recombinant αIIb and β3 molecules showed that β3 fragments corresponding to residues 111 to 31814 alone are sufficient for heterodimer formation with wild-type or truncated forms of αIIb. However, it appears that heterodimer formation is not sufficient for surface expression of the receptor; transfection studies with αIIb-truncation mutants37 38 found that mutant heterodimers were retained in the ER and degraded. By analogy with these mutants, it is likely that the truncated 1-267 form of β3 is also subject to intracellular trapping and is not expressed on the cell surface.
The second mutation found in this family resulted in the substitution of a Pro for Leu at residue 262. Because the 867-868–deletion mutant allele is unlikely to be expressed, all the β3 detectable on platelets from LD can be expected to contain the Leu262Pro mutation. In COS cells, cotransfection of wild-type αIIb and Leu262Proβ3 reproduced the platelet phenotype, with reduced levels of subunit expression on the cell surface and a heterodimer complex that was unstable in detergent lysates and not recognized by the complex-specific antibody, AP2. Analysis of the intracellular processing of αIIbLeu262Proβ3(Figure 6) showed that maturation of the mutant complex was markedly delayed. Delayed intracellular trafficking was observed in other cases of type II thrombasthenia due to point mutations of αIIb31,37 and β3,33suggesting that an altered heterodimer conformation interferes with receptor processing. The presence of detectable surface expression of Leu262Proβ3 in both platelets from LD (Figure 2) and COS cells shows that some mutant αIIbLeu262Proβ3 receptor can still undergo posttranslational processing and be exported from the Golgi complex. Therefore, the reduced levels of receptor on platelets from LD may reflect both delayed intracellular trafficking and reduced stability of the heterodimer in the plasma membrane.
The αIIbLeu262Proβ3 complex on platelets from LD was unable to support fibrinogen-dependent platelet aggregation (Figure 1) but could bind fibrin (Figure 3) in a clot-retraction assay. We studied the ligand-binding specificity of Leu262Proβ3 by expressing it in a complex with endogenous αv subunit in human embryonal kidney 293 cells. Because 293 cells express the vitronectin receptor αvβ1 but have no endogenous β3,39 transfection of β3 into these cells enables them to mediate fibrin-clot retraction.24 The αvLeu262Proβ3complex expressed in stably transfected 293 cells had the same ligand specificity as αIIbLeu262Proβ3: it bound and retracted fibrin (Figure 8) but did not adhere to immobilized fibrinogen (Figure 9). The small reduction in clot retraction observed in cells expressing αvLeu262Proβ3 was likely due to quantitative differences in surface-expression levels or qualitative differences in the receptor-ligand interaction. Clot retraction mediated by αvβ3 and αvLeu262Proβ3 appeared to proceed by means of the same mechanism; both were cation dependent, enhanced in the presence of Mn2+, and inhibited by EDTA.
Consistent with results in earlier studies in platelets20,40 and nucleated cells,24 an RGD-containing peptide inhibited fibrin-clot retraction by both cell types. Despite this, fibrin RGD sequences may not be required for integrin binding; earlier studies indicated that the RGD at Aα95-97 was not involved in αIIbβ3 binding to fibrinogen,41 and fibrinogen lacking the RGD motif at Aα572-574 still supported αvβ3-dependent clot retraction.42 We did not observe any inhibition by a fibrinogen γA 400-412 peptide, in keeping with reports that the γA region is also not required for αIIbβ3-mediated fibrin binding.13,41 These studies of mutant ligand have raised the possibility that fibrinogen and fibrin bind to different or overlapping sites on αIIbβ3.12 13 Our description of a mutant receptor that differentiates between binding fibrin and fibrinogen is further evidence for ligand-specific molecular interactions. The preservation of fibrin binding in the Leu262Pro mutant suggests that receptor conformation or stability (or both) is less critical for binding to multimeric fibrin than to fibrinogen.
The Leu at position 262 in β3 was highly conserved among β integrins (Figure 5), suggesting that it may play a role in maintaining receptor structure. Leu262 lies within a proposed intramolecular disulfide loop, between Cys232 and Cys273.30Limited tryptic proteolysis of αIIbβ3 and N-terminal sequencing of the resulting fragments found β3residues 217 to 298 associated with αIIbH residues 91-139 and αIIbL residues 1 to 26,43 suggesting that this region of β3 is involved in intersubunit contacts. Therefore, the Leu262Pro substitution may affect complex conformation and stability by disrupting a β3 contact site for αIIb. A mAb that recognizes β3 residues 262 to 302, P40, was also characterized.44 P40was reported to bind platelet αIIbβ3only after treatment with EDTA, whereas it could bind endothelial cell αvβ3 without receptor dissociation.44 This implies, first, that in αIIbβ3, the β3 262-302 epitope is not surface exposed, consistent with the hypothesis that it forms part of an interface with αIIb, and second, that the conformation of β3 in αIIbβ3 differs from that of β3 complexed to αv. A comparison of the poor expression levels of αIIbLeu262Proβ3in both platelets and COS cells with the high expression of αvLeu262Proβ3 in 293 cells indeed indicates that the conformation of the 232-273 loop is more critical for association with αIIb than with αv.
Sequences immediately adjacent to the 232-273 loop of β3have been implicated in ligand binding. Several research groups have observed that β3 peptides corresponding to residues 211 to 231 can inhibit fibrinogen binding to αIIbβ3,17,45,46 but they disagreed about whether the peptide bound fibrinogen17,45or interacted with αIIbβ3itself.46 One study reconciled these viewpoints by reporting that the β3 peptide 214-218 binds αIIbβ3, whereas a 217-231 peptide binds fibrinogen.47 In addition, structural modeling and mutagenesis of β3 identified both Asp217 and glutamic acid 220 as potential cation-coordinating residues in the MIDAS-like domain of β3.7,48 On the C-terminal side, a recombinant fragment comprising β3 residues 274 to 368 was found to bind to the γ chain of fibrinogen and a mAb against residues 274 to 403 inhibited fibrinogen binding to platelets, suggesting that this region of β3 includes a fibrinogen-binding site.49 Therefore, the intrachain disulfide loop containing Leu262 may not only contribute to heterodimer formation but may also be essential for the orientation of flanking binding sites.
Most studies of αIIbβ3-ligand interactions focused on the cation-dependent binding of soluble fibrinogen and the undefined process of receptor activation that must precede binding. Platelet adhesion to immobilized fibrinogen can proceed without αIIbβ3 activation, possibly because of the exposure of binding sites on fibrinogen after surface adhesion.50 However, a fibrin clot presents a third set of conditions to αIIbβ3 in that (1) activation of the complex is required for efficient binding,20,25 (2) the molecular structure of cross-linked fibrin differs from that of monomeric fibrinogen,51 and (3) the receptor recognizes motifs other than the γ-chain C-terminal.12 13 The in vitro phenomenon of clot retraction and the ability of certain thrombasthenic αIIbβ3 mutants to retain fibrin binding provide a powerful approach for exploring the αIIbβ3-fibrin interaction. Additional selective mutagenesis studies of β3 residues 232 to 273 based on the above findings may clarify the regulatory role of this intrachain loop in receptor activation.
Acknowledgments
We thank Sabine Weyerbusch-Bottum for technical assistance, Dr Ronggang Wang and Dr Michael Mosesson for valuable discussions, Trudy Holyst for custom peptide synthesis, and the molecular biology core facility of the Blood Research Institute for automated DNA sequencing.
Supported by grant P01-HL-44612 from the National Institutes of Health and performed during the tenure of an Established Investigator Award from the American Heart Association (P.J.N.). C.M.W. was the recipient of a Winthrop Traveling Fellowship from the Royal Australasian College of Physicians and was a postdoctoral fellow of the Wisconsin Affiliate of the American Heart Association (96-F-Post-49).
Reprints:Peter J. Newman, Blood Research Institute, The Blood Center of Southeastern Wisconsin, PO Box 2178, Milwaukee, 53201-2178; e-mail: pjn@smtpgate.bcsew.edu.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.