Abstract
Beta-thalassemia major is characterized by ineffective erythropoiesis leading to severe anemia and extensive erythroid expansion. The ineffective erythropoiesis is in part due to accelerated apoptosis of the thalassemic erythroid precursors; however, the extent of apoptosis is surprisingly variable. To understand this variability as well as the fact that some patients undergoing allogeneic marrow transplantation are resistant to the myeloablative program, we attempted more quantitative analyses. Two groups of patients totaling 44 were studied, along with 25 healthy controls, and 7 patients with hemolysis and/or ineffective erythropoeisis. By 2 flow cytometric methods, thalassemic erythroid precursors underwent apoptosis at a rate that was 3 to 4 times normal. Because thalassemic marrow has between 5- to 6-fold more erythroid precursors than healthy marrow, this translated into an absolute increase in erythroid precursor apoptosis of about 15-fold above our healthy controls. In searching for the causes of the variability in thalassemic erythroid precursor apoptosis, we discovered tight direct correlations between the relative and absolute extent of apoptosis and the extent of erythroid expansion as measured either by the absolute number of marrow erythroid precursors or by serum soluble transferrin receptor levels. These results could mean that the most extreme rates of erythroid proliferation lend themselves to cellular errors that turn on apoptotic programs. Alternatively, extreme rates of erythroid hyperplasia and apoptosis might be characteristic of more severely affected patients. Lastly, extreme erythroid hyperplasia could generate such numbers of apoptotic erythroid precursors that marrow macrophages are overwhelmed, leaving more apoptotic cells in the sample.
Introduction
Homozygous β-thalassemia (Cooley anemia) is a devastating hereditary disease characterized by reduced (β+) or absent (β°) production of the β-globin chain of the healthy adult hemoglobin. The resultant imbalance in α versus β chain synthesis is responsible for the severe anemia, which kinetically is a composite of marked ineffective erythropoiesis, as well as hemolysis of peripheral red blood cells. The attempt to compensate for this anemia leads to extraordinary ineffective erythroid hyperplasia. Patients require long-term red blood cell transfusions, which inevitably lead to iron overload. The pathophysiology of β-thalassemia has been the subject of several extensive reviews.1,2 Ferrokinetic studies have shown that as many as 80% of the erythroid precursors die in the marrow.3,4Because the genetic defect is expressed in the hematopoietic marrow, allogeneic marrow transplantation became an important and successful option in the cure of such patients.5 During the process of transplantation, a sample of marrow from the patients is harvested for genotypic study and analysis and such marrow samples allowed us to identify for the first time that accelerated apoptosis occurs in the erythroid progenitors of patients with β-thalassemia major, and probably accounts in part for the observed intramedullary lysis.6 These initial studies were based on the identification of nucleosome degradation and as such were not quantitative. In this report, we proposed to quantitatively analyze the extent of erythroid expansion and to determine whether the degree of the erythroid hyperplasia had an impact on the severity of apoptosis and on the problem of the occasional persistence of the thalassemic clone after myeloablative therapy and allogeneic transplantation.7 The extent of apoptosis was evaluated and quantified using flow cytometric methods on isolated erythroid precursors from the marrow of the patients. Flow cytometry, morphology, and measurement of soluble transferrin receptor levels in plasma were used to quantify the extent of the erythroid expansion.
Materials and methods
Patients
Two groups of patients were studied sequentially. Informed consent was obtained according to approved protocols by the institutional review boards.
Group 1 patients.
Initially, 14 patients with severe β-thalassemia major and 10 controls (allogeneic bone marrow donors) were studied. Marrow samples were obtained routinely at the time of marrow transplantation according to protocols established by the Unità Operativa Ematologia, Ospedale di Pesaro Review Board. A single operator performed all marrow aspirates for this study. Bone marrow was aspirated from the posterior iliac crest into syringes containing medium supplemented 1:10 with heparin. Ten milliliters of aspirated marrow was added to 2.5 mL of CPD anticoagulant, 1.5 mL of fetal bovine serum (FBS) and 1.0 mL of TC-199 and the samples were shipped on ice to Stanford (CA) for analysis of apoptosis and cell death.8
Group 2 patients.
Bone marrow samples were obtained for clinical purposes from 30 patients with transfusion-dependent β-thalassemia major and 15 controls in the Bone Marrow Transplantation Center in Pesaro. Sixteen male and 14 female patients with severe β-thalassemia major, ranging in age from 2 to 31 years (mean 13.8 ± 7.9; median 12), were studied. All patients were chronically transfused. Twenty-one patients had received more than 100 red blood cell transfusions, no one had received less than 10 transfusions. Fourteen patients were regularly chelated. Eleven had been splenectomized. All patients stopped transfusional and pharmacologic support at least 2 weeks before being tested.
To determine whether increased apoptosis was specific for the erythroid hyperplasia that occurs in thalassemic patients, 7 additional studies were performed in Pesaro on anemic patients with disorders of hemolysis and/or ineffective erythropoeisis. These patients were analyzed exactly as the thalassemic patients.
Bone marrow aspirates were obtained by aspiration from the posterior iliac crest into syringes containing medium supplemented with EDTA. Bone marrow aspirates in a 5-mL volume were performed always by the same operator and in the same quadrant of the posterior iliac crest. Two films from the same marrow aspirates were prepared and stained by the May-Grunwald-Giemsa method. The differential count (500 cells counted) was then performed and the myeloid:erythroid (M:E) ratio determined. Complete blood count was determined using an automated cell counter (Sysmex SF300; Toa Medical Electronics, Kobe, Japan).
Isolation and harvesting of erythroid precursors.
For group 1 patients, the marrow samples, still cold, arrived at Stanford after 36 to 48 hours and were subjected to Ficoll separation (Isoprep 1077; Robbins Scientific Corp, Sunnyvale, CA) to concentrate the cells and remove red blood cells (RBCs). Then the erythroid precursors were separated as before6 using CD45 negativity as the marker. However, rather than panning, magnetic bead column separation (Miltenyi Biotech, Auburn, CA) was used. CD45 micromagnetic beads were added to the suspension of marrow cells, incubated on ice for 30 minutes, then washed twice with phosphate-buffered saline (PBS) containing 0.5% FBS, and 1 mmol/L EDTA. The cells were then suspended in 0.5mL of the same buffer and passed through a Miltenyi magnetic column. Because the CD45 antigen is strongly expressed on leukocytes and monocytes, the immunobeads bind to these cells and not the erythroid precursors.6 Passing the suspension over a magnetic column binds the CD45 positive cells, whereas the CD45 negative erythroid precursors pass freely through the column from which they are collected and counted.
For group 2 patients, the bone marrow mononuclear cells were immediately isolated by density gradient centrifugation using Ficoll-Hypaque (specific gravity 1.077) (Lymphoprep; Nyegard, Oslo, Norway) following standard methods of Ficoll-separation technique. The cells were washed twice with PBS containing 0.01% bovine serum albumin (BSA), and resuspended in PBS. Isolation of the erythroid precursors cells was accomplished by negative selection incubating 10 × 106 bone marrow cells, with 1 mg of anti-CD45 magnetic immunobeads (Immunotech International, Marseille, France), suspended in 1 mL of PBS supplemented with 30% fetal calf serum. The suspension was incubated 10 minutes at 4°C, mixing after 5 minutes. Marrow erythroid precursor differential counts (200 to 500 cells counted) were performed on the May-Grunwald-Giemsa cytospin preparations.
Measurement of apoptosis by flow cytometry
Group 1 patients.
To be confident about the extent of apoptosis in the separated erythroid precursors, 2 methods were used. The well-studied Hoechst dye 33342 kinetically labels nuclei of cells undergoing apoptosis.9 To 0.5 mL containing 1 × 106erythroid precursors, we added 10 μL of Hoechst 33342 (10 μg/mL) (Molecular Probes, Eugene, OR) and incubated the mixture for exactly 4 minutes at 37°C, after which the samples were immediately placed on ice. Just before flow cytometry 10 μL of propidium iodide (PI) (20 μg/mL) (R&D Systems, Minneapolis, MN) was added to identify dead cells (PI positive) as well as apoptotic cells (Hoechst 33342 positive).
Apoptotic erythroid precursors were also identified and measured using fluorescein isothiocyanate-labeled Annexin V (FITC-AnV) (Boehringer, Mannheim, Germany) or Annexin V kit (R&D Systems). Annexin V (AnV) binds to phosphatidylserine that has moved from the inner to the outer leaflet of the plasma membrane phospholipid bilayer, a very early event in apoptosis.10-12 After washing twice with PBS, 1 × 106 CD45 negative cells were resuspended in 0.5 mL of binding buffer (10 mmol/L hepes/NaOH, pH 7.4,140 mmol/L NaCl, 2.5 mmol/L CaCl2). FITC-AnV was added to a final concentration of 0.5 μg/mL. Cells were incubated 10 minutes at room temperature. To identify the proportion of dead cells, 10 μL of the 20 μg/mL PI stock solution were added to the cell suspension. The mixture was then analyzed by flow cytometry. This assay allows us to discriminate alive erythroid precursors (AnV−/PI−), dead precursors with a damaged plasma membrane (AnV+/PI+), and apoptotic precursors with a still functional plasma membrane barrier (AnV+/PI−).
Group 2 patients.
Having established the fact that both methods produced similar results,13 we relied on the Annexin V method to which we added further measurements to identify the extent of the erythroid expansion as well as the other cellular components of the marrow. Apoptosis was evaluated by FACS analysis on the bone marrow erythroid precursors (CD45 negative), using FITC-AnV (Kit Bender MedSystems Diagnostic GmbH, Vein, Austria). After washing twice with PBS 5 × 105, CD45 negative cells were resuspended in 1 mL of binding buffer (10 mmol/L hepes/NaOH, pH 7.4, 140 mmol/L NaCl, 2.5 mmol/L CaCl2). FITC-AnV was added to 195 μL of the cell suspension to a final concentration of 1 μg/mL. Cells were incubated 10 minutes at room temperature, then washed once and resuspended in 190 μL of binding buffer. To identify the proportion of dead cells, 10 μL of the 20 μg/mL PI stock solution was added to the cell suspension, resulting in a final concentration of PI 1 μg/mL. The mixture was then analyzed by flow cytometry. Quantitative fluorescent analysis was performed using a FACScan (EPICS ELITE, Coulter, Hialeah, FL). From the analysis of forward and 90° light scatter, a gate was established to include all leukocytes. Ten thousand cellular events were recorded in all experiments at this gate. To calculate the total number of reactive cells per milliliter of bone marrow samples, the percentage of the reactive cells was multiplied by the total number of white bone marrow cells per milliliter of the sample.
Measurement of the extent of erythroid expansion
Erythroid expansion was evaluated both by FACS analysis on bone marrow mononuclear cells and by an enzyme-linked immunosorbent assay (ELISA) on peripheral blood sera.
FACS analysis.
Immunophenotypic analysis was performed using commercial mouse monoclonal antibodies conjugated to phycoerythrin or fluorescein directly against the following human leukocyte differentiation antigens: CD45 FITC (2D1, Becton Dickinson Immunocytometry System, San Jose, CA), CD71 FITC (YDJ.1.2.2 Immunotech International, Marseille, France), and CD16 PE (B73.1, Becton Dickinson Immunocytometry System). For each of the above, 500 000 cells were seeded into each tube and incubated for 20 minutes at 4°C with a saturating concentration of each conjugated monoclonal antibody, then washed twice. The samples were then analyzed by flow cytometry using the same procedure previously described.
Serum samples and enzyme immunoassay.
Blood samples were obtained from the antecubital vein and left to clot at room temperature, and then centrifuged and immediately aliquoted and stored at −80°C until assayed. Soluble transferrin receptor levels were measured by a commercially available sandwich ELISA kit (Amgen Diagnostics, Thousand Oaks, CA).
Statistical analysis
Data are expressed as mean ± SD unless otherwise specified.
Groups were compared by Mann-Whitney U test. Correlation between 2 parameters were estimated by the Pearson coefficient of correlation and by linear regression analysis. All tests were 2-tailed and a significance level of .05 was used.
Results
Marrow erythroid hyperplasia
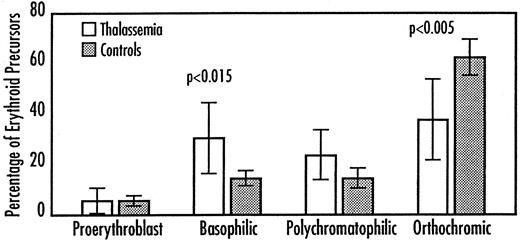
For these measurements, exactly 5 mL of marrow was aspirated. Nucleated marrow cells were counted by an automated cell counter. The absolute number of nucleated marrow cells was 45 ± 32 × 106 in the thalassemic patients and 16 ± 5 × 106 in the controls (P < .001). There were about 2.8 times as many marrow cells in the thalassemic samples. Moreover 21 of 30 patients showed an inverted M:E ratio as evaluated by the differential count of the bone marrow cells on the May-Grunwald-Giemsa–stained marrow films.14 The percentages of the nucleated marrow cells that are erythroid precursors determined by flow cytometry as detected either by CD45 negativity or by CD71 positivity (transferrin receptor), respectively, were as follows: 37 ± 15 for the thalassemics versus 19 ± 5 for the controls (P < .001), and 25 ± 17 for the thalassemics versus 9 ± 2 for the controls (P < .05). Proportionately, there are 2 to 3 times more erythroid precursors in the thalassemic samples. An erythroid precursor differential count was also performed. Thalassemic patients had a preponderance of younger forms as indicated by an increased percentage of basophilic erythroblasts (P < .015) and a decreased percentage of orthochromic erythroblasts (P < .005), when compared with controls (Figure 1). An increased number of CD16+ cells was also observed in thalassemic patients compared with controls (6.5 ± 3.3 versus 3.1 ± 1.4 × 106/mL, P < .005).
Marrow erythroid precursor differential counts were made on direct marrow aspirates.
Values are expressed as mean ± SD of the percentages.
Marrow erythroid precursor differential counts were made on direct marrow aspirates.
Values are expressed as mean ± SD of the percentages.
Apoptosis
As before,6 cytologic analysis of the CD45 negative cell suspensions showed that at least 95% of the mononuclear cells present were erythroid precursors (not shown).
Group 1 patients.
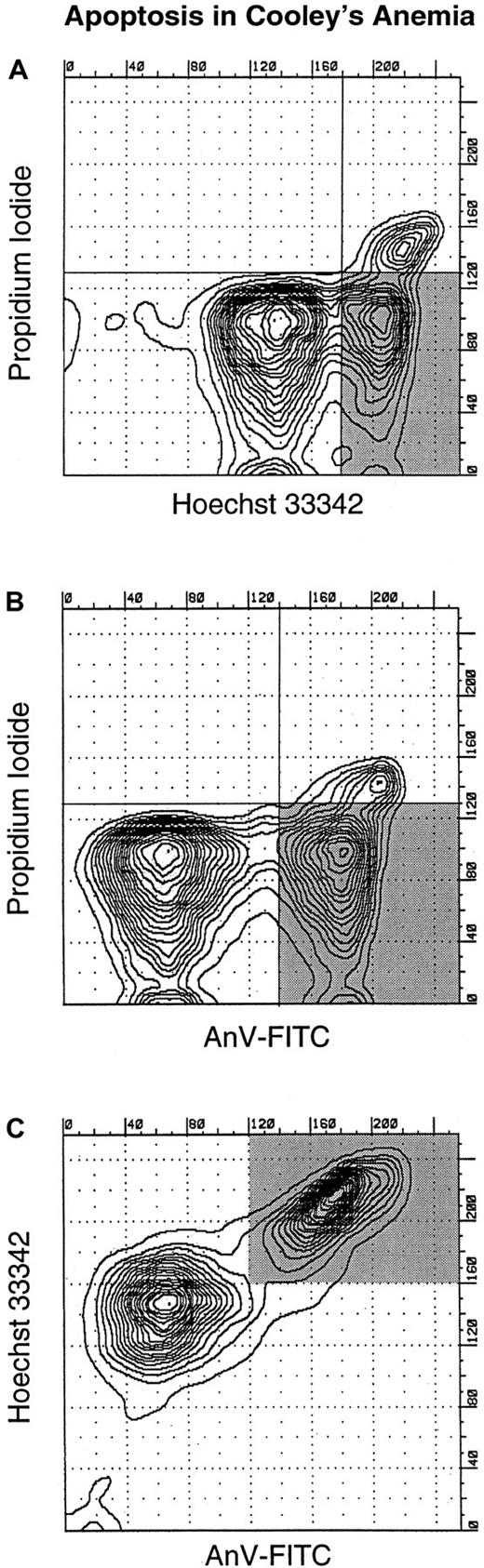
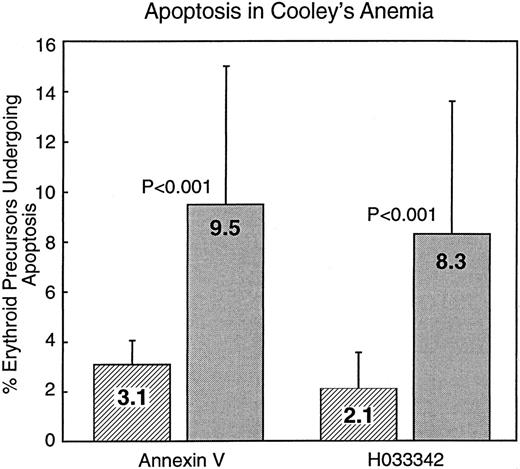
Figure2shows the flow cytometric analysis of bone marrow from a patient with β-thalassemia major. The proportion of cells that are dead (PI reactive), apoptotic (reactive with Hoechst 33342 and FITC-AnV but not with PI), and alive and not apoptotic (PI, Hoechst 33342 and AnV negative) are reported. The lower scan (Figure 2C) shows that FITC-AnV and Hoechst 33342 identify the same population of the erythroid precursors. Figure 3 summarizes the results of studies on 14 group 1 patients and 10 controls and shows that there is a significant (P < .001) 3- to 4-fold increase in the percentage of thalassemia major erythroid precursors undergoing apoptosis. This increase in apoptosis was detected by 2 quite different methods (described in “Materials and methods”). However, the error bars in Figure 3 indicate the heterogeneity of the values obtained with both methods. This puzzling heterogeneity as well as a desire to better understand the quantitative extent of the increase in thalassemic erythroid precursors leads us to do more quantitative experiments. It was also thought that a more quantitative approach to the extent of erythroid expansion might explain the occasional difficulty experienced in eradication of the thalassemic clone by our myeloablative protocol.
Flow cytometric analysis of purified erythroid precursors from a patient with Cooley anemia.
(A) Reactivity with Hoechst 33342 on the abscissa and PI on the ordinate. The closeness of the contour lines reflects the numbers of cells reacting. There are 3 definable populations: PI reactive cells are dead; Hoechst 33342 are reactive, but PI nonreactive are apoptotic (shaded area); and the remaining cells (PI and Hoechst 33342 nonreactive) are alive and not apoptotic. Panel B is similar to A, except that FITC-AnV reactivity is recorded on the abscissa. The shaded area identifies the apoptotic population. (C) Reactivity of the erythroid precursors with FITC-AnV on the abscissa and Hoechst 33342 on the ordinate. The 2 methods identify the same apoptotic population (shaded area).
Flow cytometric analysis of purified erythroid precursors from a patient with Cooley anemia.
(A) Reactivity with Hoechst 33342 on the abscissa and PI on the ordinate. The closeness of the contour lines reflects the numbers of cells reacting. There are 3 definable populations: PI reactive cells are dead; Hoechst 33342 are reactive, but PI nonreactive are apoptotic (shaded area); and the remaining cells (PI and Hoechst 33342 nonreactive) are alive and not apoptotic. Panel B is similar to A, except that FITC-AnV reactivity is recorded on the abscissa. The shaded area identifies the apoptotic population. (C) Reactivity of the erythroid precursors with FITC-AnV on the abscissa and Hoechst 33342 on the ordinate. The 2 methods identify the same apoptotic population (shaded area).
Summary of group 1 studies using both Hoechst 33342 and FITC-AnV.
Controls, ▨; thalassemics, ░. Mean values are shown within the bars, and the error lines indicate the SD values.
Summary of group 1 studies using both Hoechst 33342 and FITC-AnV.
Controls, ▨; thalassemics, ░. Mean values are shown within the bars, and the error lines indicate the SD values.
Group 2 patients.
Marrow aspirates of 30 more patients with β-thalassemia major were obtained and the extent of apoptosis in their erythroid precursors was evaluated by the FITC-AnV method (Table1). The proportion of thalassemic erythroid precursors undergoing apoptosis (CD45−/AnV+/PI−) was about 3-fold greater than the controls. These values were very similar but slightly lower than the values obtained in the group 1 patients.
Because the marrow cellularity is increased 2.8-fold in the patients and they have about twice as many erythroid precursors proportionately, one would expect that the absolute increase in thalassemic erythroid precursors would be 5 to 6 times greater than in the controls, ignoring the extension of marrow space and extramedullary erythropoiesis. With a 3-fold increase in the proportion of erythroid precursors undergoing apoptosis (Figure 3, Table 1), the absolute increase in thalassemic erythroid precursors undergoing apoptosis would be expected to be about 15-fold, which is close to the 14-fold increase actually observed (Table 2).
Seven anemic but nonthalassemic patients, representing erythroid expansion due to hemolysis or ineffective erythropoeisis, were also studied (Table 3). All had evidence of erythroid expansion but neither the percentage of erythroid apoptosis nor cell death was increased, when compared with our healthy controls (Table 1).
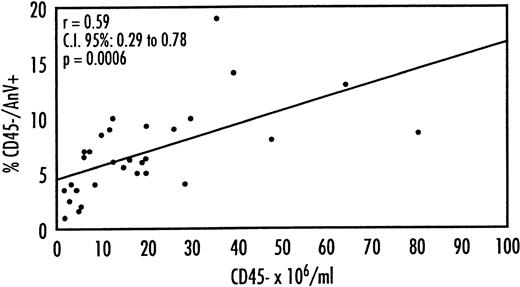
Correlation between erythroid hyperplasia and apoptosis
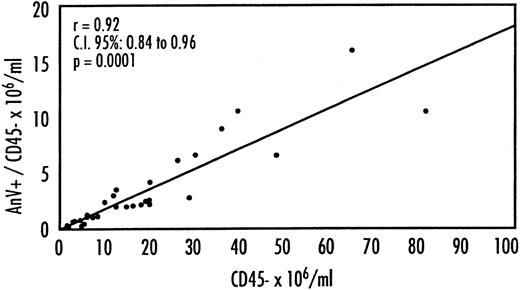
In searching for an explanation for the variation in levels of apoptosis in the β-thalassemic patients (Figure 3, Tables 1 and 2), we observed tight direct correlations between both the relative (Figure4) and absolute (Figure5) numbers of apoptotic erythroid precursors (CD45−/AnV+) and the extent of erythroid expansion as indicated by the absolute numbers of CD 45 negative erythroid precursors (r = 0.59,P < .001; r = 0.92, P < .001, respectively). When the relative and absolute numbers of apoptotic erythroid precursors were plotted against the absolute number of CD71 positive marrow cells (an alternative marker of erythroid precursors), similar tight direct correlations were obtained (not shown).
Correlation between the percentage of the apoptotic erythroid precursors (AnV+/PI−/CD45−) and the total number (× 106) of erythroid precursors (CD45−).
Correlation between the percentage of the apoptotic erythroid precursors (AnV+/PI−/CD45−) and the total number (× 106) of erythroid precursors (CD45−).
Correlation between the total numbers (× 106) per milliliter of apoptotic erythroid precursors (AnV+/PI−/CD45−) and the absolute number of erythroid precursors (CD45−) (× 106)/mL.
Correlation between the total numbers (× 106) per milliliter of apoptotic erythroid precursors (AnV+/PI−/CD45−) and the absolute number of erythroid precursors (CD45−) (× 106)/mL.
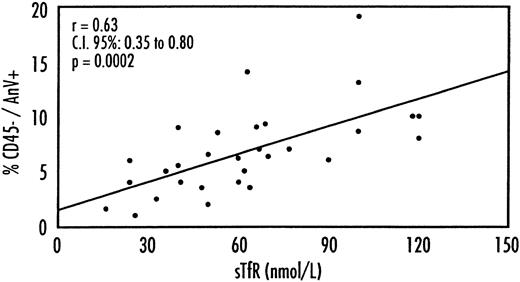
An indicator of overall erythropoietic activity that is independent of the variations in marrow aspiration, sampling, and flow cytometry is the serum level of soluble transferrin receptor15 (sTfR). There was again a strong correlation between the extent of erythroid expansion expressed by sTfR levels and both the proportion (Figure6) and absolute numbers (not shown) of thalassemic erythroid precursors undergoing apoptosis. No such correlations between apoptosis and numbers of erythroid precursors were observed in comparable studies on healthy control marrow samples (not shown).
Correlation between the percentage of the apoptotic erythroid precursors (AnV+/PI−/CD45−) and levels of serum transferrin receptor (sTfR).
Correlation between the percentage of the apoptotic erythroid precursors (AnV+/PI−/CD45−) and levels of serum transferrin receptor (sTfR).
Discussion
We had 3 aims in this study: (1) to discover the extent and severity of apoptosis in the erythroid precursors of patients with β-thalassemia major as a likely contributing factor to the extensive ineffectivity seen in these patients in which as many as 80% of erythroid precursors die in the marrow; (2) to understand why in a well-characterized genotypic disorder there should be such heterogeneity in the extent of apoptosis; and (3) to shed light on why myeloablative therapy does not regularly destroy the thalassemic clone.
To extend and quantify our first qualitative demonstration of increased apoptosis in β-thalassemia major erythroid precursors,6we used 2 quantitative flow cytometric methods. These were chosen to reflect both plasma membrane and nuclear alterations in the apoptotic process. Both methods gave concordant results in showing that they identified the same population of erythroid precursors (Figure 2) and that there was a 3- to 4-fold significant increase in percentage of erythroid precursors undergoing apoptosis in patients versus controls (Figure 3). It should be recalled that in our early study6we found no evidence of increased apoptosis in thalassemic CD45 positive myeloid and lymphoid marrow cells.
These studies on group 1 patients, although providing requisite quantitative data, uncovered interesting biologic problems. One was that the extent of apoptosis was quite variable in patients who seemed to be clinically and genotypically quite similar. The second was that measurement of the percentage of erythroid precursors undergoing apoptosis greatly underestimated the problem in β-thalassemia major, in which there is enormous erythroid hyperplasia. Thus, the absolute number of apoptotic erythroid precursors in patients is likely to be very much increased.3-6,16 17
To analyze these questions we needed a more quantitative approach to the analysis of erythroid precursors in β-thalassemic and healthy marrow. Furthermore, there are clinical clues from the thalassemic marrow transplantation program at Pesaro that patients with extreme erythroid hyperplasia may have a higher frequency of graft rejection with reversion to thalassemic erythropoiesis. If quantitative measurement of the extent of erythroid expansion were to be predictive of the outcome of bone marrow transplantation, it would be a useful addition to our current clinical assessment that is based on regularity of chelation, hepatomegaly, and presence of portal fibrosis.5 7
Therefore, we extended the study to group 2 patients specifically trying to assess the impact of the extent of erythroid expansion. Our results show that the extent of the thalassemic erythroid hyperplasia quantitatively evaluated by absolute counts of CD45 negativity and CD71 positivity, directly correlates with the relative and absolute extent of erythroid precursor apoptosis (Figures 4 and 5). The use of the soluble serum transferrin receptor level15 as an index of overall erythropoiesis showed similar direct correlations with the relative extent of apoptosis (Figure 6).
An important question is whether increased erythroid apoptosis is a specific pathophysiologic lesion in β-thalassemia major or whether it occurs in other forms of hemolysis or ineffective erythropoiesis characterized by erythroid expansion. Our studies on 7 patients with several sorts of hemolytic anemia and ineffective erythropoiesis (Table3) show that hemolysis or erythroid expansion per se does not increase the proportion of apoptotic erythroid precursors.
An important consideration is whether ineffective erythropoiesis is invariably characterized by increased erythroid apoptosis. There is morphologic evidence of increased erythroid apoptosis in congenital dyserythropoietic anemia18 in which erythropoiesis is ineffective. Ineffective hematopoiesis has been reported in 19 patients with myelodysplastic syndrome (7 RA, 7 RAEB, 5 RAEBt).19However, in 2 reports on megaloblastic anemia encompassing 17 patients with folate or cobalamin deficiency, using methods similar to this20 and our prior study,21 there was no increase in erythroid apoptosis even though there was distinct evidence (increased PI+) of intramedullary erythroid cell death.20 Neither of our 2 patients with sideroblastic anemia showed an increased proportion of apoptotic erythroid precursors (Table 3). Therefore, the association of increased erythroid apoptosis with ineffective erythropoiesis is not invariable.
There are several hypotheses, not mutually exclusive, which might explain why profound erythroid expansion should lead to a relative and absolute increase in thalassemic erythroid precursor apoptosis. When a cell line is forced by physiologic or pathologic mechanisms to increase its proliferative rate, the chances for errors increase, leading to aberrations that are detected by the affected cells, which then turn on their apoptotic programs.22 23
A second explanation is that we measure erythroid precursor apoptosis directly from our patients' marrow at a single point in time. However, one of the biologic aims of apoptosis is to identify damaged cells and remove them, thus limiting any damage such cells might do. Phosphatidylserine is translocated from the inner to the outer layer of the plasma membrane24,25 of apoptotic cells, where it can be recognized and the affected cells removed by macrophages.26,27 Therefore, our measurement of apoptosis is a composite of the erythroid precursors undergoing apoptosis at that moment versus the ability of marrow macrophages to remove them. At the higher levels of erythroid hyperplasia, the extent of apoptosis may exceed the ability of marrow macrophages to remove such cells, leading to higher apparent levels of apoptosis. The number of CD16+cells (described in “Results”), many of which are macrophages, is increased 2-fold in the marrow of our thalassemic patients, and the in vitro capacity of macrophages to phagocytose thalassemic versus normal erythroid precursors is also increased 2-fold,28 leading to a possible quadrupling of phagocytic capacity. In contrast, the absolute increase in apoptosis in our patients is 14-fold. However, the activation or up-regulation of thalassemic phagocytes may further increase their effectiveness.29 This hypothesis does not explain the decreased number of orthochromic erythroblasts observed in our patients (Figure 1).
A third explanation is that, for unclear reasons, the patients with greatly increased apoptosis and erythroid expansion have a more severe disease.
It is not clear why patients with extreme erythroid hyperplasia may be resistant to the preparative myeloablative therapy and reject their graft. We are currently testing the role of hypertransfusion in the preparative program in such patients to reduce the extreme erythroid hyperplasia.
Acknowledgment
We thank Dr Locatelli for providing a bone marrow sample from a patient with sideroblastic anemia.
Preliminary reports of this work in progress were presented at the annual meetings of the American Society of Hematology in 1996, (Blood; 88 suppl 1, Abstract:2817, 1996), 1998 (Blood 92 suppl 1 Abstract 3134, 1998) and 1999 (Blood 94 suppl 1 Abstract 1868, 1999).
Supported by Fondazione Berloni contro la Talassemia, Pesaro, Italy, and a grant from the NIH RO1-DK 13682 (S.L.S.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Guido Lucarelli, Unità Operativa di Ematologia e Centro Trapianto di Midollo Osseo, Azienda Ospedale di Pesaro, 61100 Pesaro, Italy; e-mail:g.lucarelli@wnt.it.