Abstract
Development of the full repertoire of hematopoietic-lymphopoietic cells from a single stem cell requires specific contacts with stromal cells. The spatio-temporal organization of these cell associations in the bone marrow in ontogeny is, however, not well understood. In the adult, 10% of marrow cells form a cohort of compact aggregates, the hematon. In the hematon mesenchymal cells (Stro-1+), perivascular lipocytes (desmin+), endothelial cells (CD34+, Flk-1+, Sca-1+), and macrophages amalgamate with the hematopoietic progenitors long-term culture-initiating cells (LTC-IC), cobblestone area–forming cell (CAFC), high-proliferative-potential colony-forming unit (HPP-CFU), granulocyte-macrophage (GM)–CFU, and burst-forming unit–erythroid (BFU-E). During endochondral ossification of the femur, GM-CFU and day 7 CAFC numbers increased progressively from day 17 of gestation, but primitive, day 35 LTC-IC appeared from postnatal day 2. Unexpectedly, bone marrow (BM) taken between embryonic day 17 and day 5 was unable to support myeloid cell production in long-term cultures or to support day 35 LTC-IC growth. However, a gain in stromal cell competence occurred between days 7 and 10, which was correlated with the emergence of hematon in the BM. Thus, acquisition of hematopoietic competence by BM lags behind for approximately 10 days after the initial hematopoietic cell influx. In the adult, the hematon fraction was 3.7-fold enriched in day 35 LTC-IC over the buffy coat. It produced more GM-CFU and HPP-CFU in myeloid culture and more B cells in lymphopoietic “switch” cultures. It is reported that stromal hematopoietic units named hematons are specific morphogenetic structures that emerge at a well-defined postnatal stage of development in long bones, delineate discrete territories for hematopoietic stem cell seeding and development, embody the most productive hematogenous compartment in the BM, and probably enclose a morphogenetic organizer.
Introduction
Hematopoietic stem cells (HSCs) can ensure 3 vital functions—self-renewal, expansion, and development toward the full spectrum of hematolymphoid cell lineages.1-7 Fate-map analyses of HSCs in avian and mammalian embryos provide evidence that the association between endoderm and ventral mesoderm may gain hematopoietic competence at distinct anatomic locations. Putative hemangioblasts of the extraembryonic yolk sac generate hematopoietic islands from days 7 to 7.5 of gestation (E7-7.5) in the mouse,8,9 which ensure the rapid production of erythrocytes and macrophages until E12, when the yolk sac involutes. Yolk sac hematopoiesis is therefore incomplete; ephemeral and hematogenous islands do not seem to support substantially definitive HSCs amenable to long-term marrow repopulation in the adult.9-13
Recent investigations provide evidence that adult-type HSCs emerge at E8.5 from a distinct region of embryonic ventrolateral mesoderm, the para-aortic splanchnopleura (P-Sp), which later develops into the aorta-gonad-mesonephros region.9,12,14-16 Between E10 and E13, HSCs migrate to the liver primordium, which becomes the main hematopoietic organ with overwhelming erythropoiesis. HSCs may expand significantly in the liver primordium and later in the spleen,8,15,17 before definitive hematopoietic tissues develop in the bone marrow (BM). The cellular and molecular mechanisms that determine autonomous hematopoietic competence in the BM have not been characterized yet. BM development is predisposed by bone formation by the endochondral ossification of cartilaginous rudiments.18 On approximately E15-16, chondrocytes become hypertrophic and then undergo apoptotic cell death in the central diaphysis of long bone rudiments. Hypertrophied chondrocytes secrete vascular endothelial growth factor (VEGF) that triggers vascular cells to penetrate the perichondrium,19 bringing along osteoblast precursors and circulating hematopoietic cells, mostly primitive macrophages. The vasculature provides a fractal-type, arborized conduit20 for the recruitment of chondroclasts that resorb hypertrophied chondrocytes and for osteoblasts that depose a calcified spongioid shaft replacing the cartilage. Increasing numbers of hematopoietic colony-forming cells (GM-CFU and CFU-S) were detected in the femora from E17,8,21 suggesting that active hematopoiesis starts at approximately E17 to E18 in the mouse femur. Because a reciprocal correlation existed between colony-forming cell (CFC) contents in the liver primordium and the developing femur at perinatal stages, it was concluded that BM is colonized progressively by liver-derived HSCs.8,16 Indeed, fetal liver cells tagged by the in vivo transfer of a retrovirus-driven marker gene were later retrieved in the adult BM.22 However, it is not well established whether, at the initial step of endochondral bone formation, hematopoietic progenitor cells arise locally from previously seeded HSCs or are continuously seeded from the liver by the vasculature irrigating the femora. Clearly, the exact fate map23 of the BM primordium and spatiotemporal emergence of specific stromal cells, whereby the BM gains definitive hematopoietic competence during ontogenesis, have not been determined.
In the adult marrow, HSC development requires the support provided by bone tissue and by a network of stromal cells. Long-term BM cultures (LTBMC) display after several weeks rare hematogenous areas (cobblestone area [CA]) in the adherent layer,24,25 the presence of which is absolutely required for long-term HSC expansion. The enumeration of LTC-IC/CAFC on a competent stromal feeder layer has became the most reliable functional test to quantify HSCs in vitro.26-29 Searching for a preferential spatial location of HSCs in the mouse femur has led to contradictory data, though, leaving open whether HSC-associated stromal cells have a fixed territory allocated in the BM.30-36
We have postulated that critical stromal cells and hematopoietic progenitors form firm multicellular units under physiologic conditions. A cohort of preformed cell complexes, termed hematons, has been isolated in the low-density, floating layer of normal primate BM aspirates.37,38 Hematon complexes can be also isolated from the gently dispersed BM of mice, using repeated 1gsedimentations and decanting the buffy coat suspension.39,40 The hematon is a finely arborized stromal framework that includes mesenchymal cells, endothelial cells, and macrophages. These spherical particles are tightly packed with hematopoietic cells, including primitive cells with marrow-repopulating ability (MRA), CAFC, CFU-Sd12 in the mouse hematon, and HPP-CFC, BFU-E, GM-CFU, and differentiated postmitotic cell populations in both human and mouse.40 41
Stromal cells and hematogenous cells may be generated simultaneously during BM morphogenesis or may be attracted together by a putative organizer to form hematon complexes, such as the nephron in the kidney and the gustatory bud in the tongue or germinal centers in the lymph nodes. This study was aimed at characterizing the cells that constitute the hematon core complex, at determining the stage of its emergence in the femur during ontogeny, and at identifying when in development the BM stromal microenvironment gains functional autonomy.
Materials and methods
Mouse BM preparation
Embryonic tissues.
C57BL/6 mice were purchased from IFFA CREDO (L'Arbresle, France), bred under a 12-hour light-dark schedule, and fed sterilized food (UAR, Epinay-sur-Orge, France) and acidified water ad libitum. Vaginal plugs were checked the morning after natural overnight mating. Mice were killed by cervical dislocation, and uteri were removed aseptically. Embryos were rinsed in phosphate-buffered saline, and femora were dissected with no. 55 watchmaker forceps (Drumond, Poly-Labo, France) and microsurgical knives prepared from 30-gauge needles. Femora from embryos and young mice were cleaned of muscle and cartilage, washed, and cut longitudinally into halves. The diaphyseal shaft was denuded from the ossified shell and dissociated with 2 30-gauge needles under a STEMI SV8 stereomicroscope (Zeiss, Oberkochen, Germany).
Purification of the buffy coat, hematon, and hematon–core complex fractions.
Eight- to 16-week-old mice were killed by cervical dislocation. Femora were cleaned, and the proximal (hip) and distal (knee) parts were opened using a 23-gauge needle. Then the BM was recovered by forcing 2-mL culture medium through the femoral shaft. BM pooled from 4 to 6 femora was pipetted vigorously 10 times, and particles were allowed to settle at 1g for 15 minutes. The upper cell suspension was transferred to a new tube, and the pellet was pipetted again 10 times in 1-mL culture medium and diluted to 5 mL. After 15-minute sedimentation, the 2 supernatants were combined and centrifuged (400g, 7 minutes) to obtain the “buffy coat.” The pellet was transferred to a Petri dish, and bone and muscle fragments were removed to obtain the purified hematon fraction. Hematon units were counted under the stereomicroscope in one-tenth aliquots of the total hematon fraction. Tiny hematon core particles were purified by forcing either the whole hematon fraction or single hematons through 25-gauge and 30-gauge needles 10 times each, followed by repeated 1gsedimentations.
Cell counting, staining, and vitality tests.
BM fractions were dissociated in LTC medium containing 0.1% type II/IV collagenase for 30 minutes at 37°C. Cells were washed 2 times in 5 mL medium, counted, and used in quantitative progenitor cell assays. Red blood cells were lysed in 0.1% acetic acid, and total nucleated cells (TNCs) were counted in a hemocytometer. BM film and cytospin preparations were stained with May-Grünwald-Giemsa. Cell vitality was determined by trypan blue (0.2%) exclusion. Apoptotic cell death in LTCs was analyzed by fluorescein isothiocyanate (FITC)–labeled annexin V–propidium iodide (PI) double staining (Coulter, Miami, Florida). Briefly, 5 × 105 cells were spun down (400g, 7 minutes), suspended in 490 μL incubation buffer with 5 μL FITC–annexin V and 5 μL PI, and incubated for 10 minutes at 4°C in the dark. Cells and apoptotic bodies were analyzed under an ICM-405 epifluorescence microscope (Zeiss) using a 515- to 565-nm filter for FITC and a 590-nm filter for PI.
In vitro assays for clonogenic cells
Semisolid cultures for myeloid and erythroid colony-forming cells.
HPP-CFC, GM-CFU, and BFU-E progenitor cells were determined in a modified40 double-layer, methylcellulose-agar culture system.42 Briefly, 0.7 mL 0.5% agar in a 35-mm Petri dish (ATGC) was overlaid with test cells in 1.5 mL 0.9% complete methylcellulose medium containing 1% bovine serum albumin (BSA) and 0.1 mmol/L 2-mercaptoethanol (2-ME) (HCC #4230; StemCell Technologies, Vancouver, British Columbia). Cells were stimulated with a mixture of murine recombinant hematopoietic growth factors (mrHGFs): 50 IU mrIL-1, 4 ng mrIL-3, 20 ng mrGM-CSF, and 100 ng hrG-CSF (Genzyme, TEBU, Le-Perray-en-Yuelines, France) for myeloid cultures and with mrHGFs plus 10 ng mrSCF and 3 U erythropoietin/mL for erythroid cultures. GM-CFU were counted after 7 days; HPP-CFC was counted on day 28 from the same dishes, and BFU-E was counted on day 14 of incubation.
Assay for long-term culture-initiating cells (LTC-IC/CAFC).
Stromal feeder cells were prepared using the BM hematon fraction 7 to 10 days before limiting dilution analysis (LDA); 2 × 107dispersed cells were seeded in 10 mL complete LTC medium in a 25-cm2 T-flask (ATGC). The adherent layer was trypsinized and washed, and aliquots of 3 × 105 cells in 100 μL LTC medium were seeded in 96-well flat-bottom microplates (ATGC). Complete LTC medium consisted of Iscove modified Dulbecco medium (IMDM, Flow Laboratories, Irving, United Kingdom) supplemented with 0.5 mg/L ascorbic acid, 37 mg/L myo-inositol, 10 mg/L folic acid, 5 × 10−5 mol/L 2-ME, 10−6mol/L hydrocortisone hemisuccinate (Sigma, St Louis, MO), 12.5% preselected horse serum, 12.5% heat-inactivated fetal bovine serum (FBS; Hybrimax; Sigma), and penicillin (100 IU/mL)–streptomycin sulfate (100 μg/mL). A total dose of 20 Gy was given at 1.4 Gy/min from a IBL 637 gamma irradiator equipped with a cesium Cs137 source (Cis-Bio International/ORIS Industry SA, Orsay, France), and 24 hours later serial half-dilutions of test cells in 100 μL medium (24 parallel wells) were seeded over feeder cells. In some experiments the mouse BM stroma cell line MS-5 was used as feeder without irradiation.43 Cultures were maintained at 33°C with weekly half-medium changes. Positive wells, containing at least 5 phase-dark cells under the stroma cells (CAFC) were counted under an ICM-405 inverted phase-contrast microscope (Zeiss). Ninety percent to 95% of positive wells contained more than 5 GM-CFU (range, 5-750) on day 35.
Long-term culture of fractionated bone marrow
Myeloid LTBMC.
The abilities of the buffy coat and hematon fractions to produce cells were studied in liquid cultures maintained without irradiated stromal feeder layers. Buffy coat cells and hematons were seeded at 5 × 105 cells per 2 mL LTC medium in 24-well Nunclon tissue culture dishes (Nunc, Inc, Naperville, IL). Myeloid LTC medium was identical to that described for LTC-IC/CAFC assays. Cell production was determined, using semisolid medium colony assays, in the nonadherent fraction and in adherent cells dispersed with 0.1% type II/IV collagenase and washed 2 times in Iscove modified Dulbecco medium–20% FCS.
Myeloid-lymphoid cell production in LTBM switch culture.
HSCs for myeloid and lymphoid cell lineages were assayed using myeloid cultures (2 × 106 cells in 2 mL medium) in 35-mm Petri dishes and were maintained for 4 weeks at 33°C, as described above for standard LTBMC.44 Medium and nonadherent cells were then removed, and adherent cells were washed 3 times with lymphoid culture medium containing RPMI-1640 medium (HEPES modification; Sigma), 5% FBS (Hybrimax, Sigma), 50 μmol/L 2-ME, and antibiotics. Cultures were incubated at 37°C, and TNC and emerging B lymphocytes were analyzed from the nonadherent suspension on days 7, 14, and 21, from the adherent layer on day 21 by flow cytometry, and on Giemsa-stained cytospin preparations.
Organotypic microcultures.
Single hematon units, or hematon core complexes, were isolated under the STEMI SV8 stereomicroscope (Zeiss). Single aggregates were transferred in flat-bottom microwells, and the development of native CA was analyzed over time.
Assay of native and secondary CA-forming cell complexes.
The buffy coat suspension and partially dissociated hematon fractions were diluted in 24 mL LTC medium and seeded in 384-microwell cloning plates (Greiner, Nürtingen, Germany). Adherent stroma cell colonies (F-CFU) and discrete foci containing hematopoietic progenitor cells under stromal cells (CA) were counted in each microwell over time under an ICM-405 microscope (Zeiss).
Cell marker studies
Cytochemistry.
Acetylcholinesterase (ACE) reaction was used to identify megakaryocytes, acid phosphatase was used to identify macrophages, osteoclasts/chondroclasts were detected by tartrate-resistant acidic phosphatase (#387; Sigma), and osteoblasts were detected by alkaline phosphatase (#104; Sigma) reaction. Lipocytes were identified by staining with oil red.
Flow cytometry.
Collagenase-dissociated BM fractions (5 × 105 cells) were washed in PBS with 1% BSA/0.1% Na azide and incubated for 30 minutes with fluorochrome-labeled antibodies. The mouse B-cell lineage was analyzed using rat FITC-labeled anti-CD45R, B220 antibody (Caltag, Burlingame, CA) after the adsorption of test cells with 10% whole rat serum in DPBS for 40 minutes. Cells were washed twice in 1% BSA/DPBS, and the percentage of labeled cells was determined by flow cytometry on an Epics II fluorescence-activated cell sorter (Coulter).
Immunostaining.
Hematopoietic progenitor cells were identified in native cell aggregates on cytospin slide preparations with antibodies to Sca-1 (Ly6A/E, mouse IgG-FITC; Immunotech/Coulter, Marseille, France), CD117 /c-kit (RAM IgG-PE; Immunotech), CD34 (RAM-IgG- FITC; Immunotech), Thy-1 (RAM IgG2c-FITC; Immunotech), CD41 (RAM IgG-FITC; Immunotech), CD49d/VLA-4 (RAM IgG-FITC; Caltag), and stroma cells were identified with antibodies to Stro-1 (RAM pcIgG, kindly provided by Dr Paul Simmons), desmin 33 (mouse IgG; DAKO, Glostrup, Denmark), Flk-1/KDR (MAH IgG-FITC; Santa Cruz Biotech, Santa Cruz, CA), VCAM-1 (GAH IgG-FITC; Santa Cruz Biotech), αSM actin (MAH IgG-Cy3; Caltag), ICAM-1 (RAH IgG; Caltag), Notch-1 (GAH IgG; Santa Cruz Biotech), and MMP-9–gelatinase-B (GAH IgG; Santa Cruz Biotech). Cells were washed in DPBS, fixed in methanol at −20°C for 5 minutes, and, before staining, rehydrated in PBS/0.5% albumin/0.05% NaN3. Nuclear factors were detected after permeabilization by adding 0.2% NP-40 to the staining solution. Anti-Hox-11 (RAM IgG), anti-Oct-2 (RAH IgG), and CBF-A (GAH IgG) were from Santa Cruz Biotech. They were detected at 1:100 to 1:500 dilutions with FITC-labeled secondary antibodies. Preparations were washed, mounted with the antifading compound ProLong (Molecular Probes, Eugene, OR), and analyzed under a Leica DMR epifluorescence microscope.
Histology.
Embryos or dissected tissues were fixed in 2% paraformaldehyde–0.1% glutaraldehyde in PBS for 60 minutes at 20°C, then washed 3 times for 60 minutes in PBS at 4°C. Selected specimens were further cleaned; they were then dehydrated in 30% and 50% (vol/vol) ethanol in water for 10 minutes, in 50% ethanol in Unicryl (British BioCell, Cardiff, United Kingdom) for 30 minutes, and in 100% Unicryl overnight at −20°C. Samples were finally embedded in Unicryl using UV light polymerization for 2 to 3 days. Semithin sections (2 μm) were cut on a Reichert ultramicrotome and stained with hematoxylin/fast green.
Statistical analysis
Cells and colonies were counted in triplicate cultures; data represent the mean (SD). The significance of differences between experimental data was calculated using Student t test. Limiting dilution analyses of LTC-IC/CAFC populations were performed on 24 parallel microcultures using 3 serial half-dilutions. The input number of cells seeded per well was plotted against the log percentage of negative wells on days 7 and 35 of culture. Then the frequency of LTC-IC/CAFC (1 test cell/x input cells) was extrapolated from the linear regression curves at the log percentage of −0.37.26 Statistical analyses were performed with StatMate, and graphics were made with Prism software (GraphPad, San Diego, CA).
Results
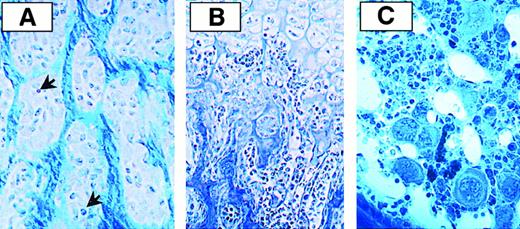
Histologic structure of the developing femur
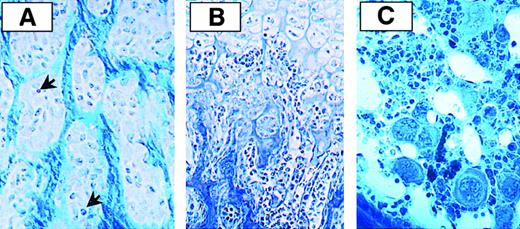
Chondrocytes become hypertrophied and undergo cell death by apoptosis at the central diaphysis between E16 and E18. Mesenchymal cells migrate from the perichondrium to the cartilaginous BM primordium and differentiate into osteoblasts that form a spongy bone shaft filling the whole diaphysis (Figure 1A). Capillary endothelial cells penetrate the BM primordium, bringing along blood cells, mostly macrophages and red blood cells, from the circulation. Osteolysis starts at the central, periosteal diaphysis; in newborns, the inner mass consists of a fluid phase at the center and 2 compact spongy bone cones resembling sand-glass. The central artery undergoes a series of fractal bifurcations that follow the way of retracted, apoptotic chondrocytes. At this stage neither erythroid cells nor megakaryocytes can be discerned (Figure 1B). In young adult mice the diaphysis is filled with BM parenchyma and by a voluminous vascular bed, whereas the epiphysis contains trabecular bone alveoli that enclose whole BM with many erythroid and megakaryocytic islands (Figure 1C).
Histology of the developing mouse femur.
(A) E17 femur embedded in Unicryl and stained with hematoxylin/fast green shows spongy bone. Osteoblasts are aggregated in nodules and depose a calcified bone matrix in their surroundings. Arrows point to hematopoietic cells. (B) An abundant vascular conduit that follows the way of hypertrophied chondrocytes characterizes the newborn femur. (C) Proximal region of the femur from a young adult mouse containing spongy bone filled with bone marrow. Megakaryocytes form islands with erythroid and myeloid cells.
Histology of the developing mouse femur.
(A) E17 femur embedded in Unicryl and stained with hematoxylin/fast green shows spongy bone. Osteoblasts are aggregated in nodules and depose a calcified bone matrix in their surroundings. Arrows point to hematopoietic cells. (B) An abundant vascular conduit that follows the way of hypertrophied chondrocytes characterizes the newborn femur. (C) Proximal region of the femur from a young adult mouse containing spongy bone filled with bone marrow. Megakaryocytes form islands with erythroid and myeloid cells.
Emergence and expansion of hematopoietic progenitor cells and hematon units
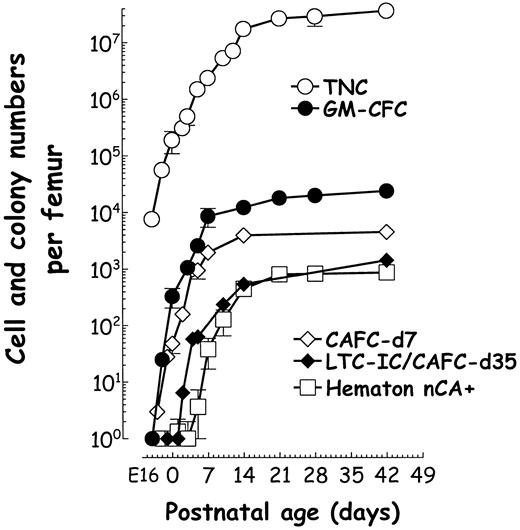
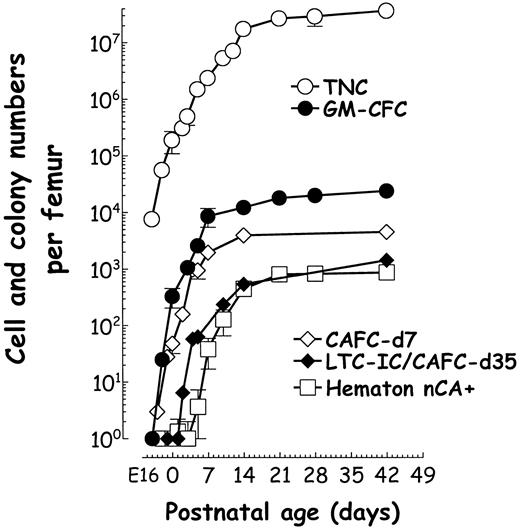
TNC and CFU in culture were determined in femora dissected from fetuses, pups, and young adult mice. From E16 hematopoietic cells could be carefully mechanically dissociated from the cylindrical ossified diaphysis. In one femur there were as few as 12 × 103TNC and no CFU on E16, 60 × 103 TNC and 28 ± 12 CFU at E17, and the numbers increased logarithmically until postnatal day 14. The frequency of early and late LTC-IC/CAFC in the femur was also studied by LDA using the MS-5 stroma cell line. Day 7 CAFC could be detected in the femur from E17; however, day 35 LTC-IC/CAFC appeared only after birth between day 2 and day 5, and the numbers increased and reached inflection on day 14 or so (Figure2).
Expansion of marrow cells and emergence of the hematon during perinatal ages.
The femoral inner mass was recovered from 8 to 12 embryos or little mice. Half of each tissue was used to prepare a single-cell suspension for quantitative colony assays and the other half to count hematons and native cobblestone colonies at day 7 in LTC. The numbers of TNC (○), total GM-CFC and HPP-CFC (●), and day 7 CAFC (⋄) increased logarithmically from E17. Day 35 LTC-IC/CAFCs (♦) appear at day 2, and hematon units containing native CA (■) emerge from days 5 to 7.
Expansion of marrow cells and emergence of the hematon during perinatal ages.
The femoral inner mass was recovered from 8 to 12 embryos or little mice. Half of each tissue was used to prepare a single-cell suspension for quantitative colony assays and the other half to count hematons and native cobblestone colonies at day 7 in LTC. The numbers of TNC (○), total GM-CFC and HPP-CFC (●), and day 7 CAFC (⋄) increased logarithmically from E17. Day 35 LTC-IC/CAFCs (♦) appear at day 2, and hematon units containing native CA (■) emerge from days 5 to 7.
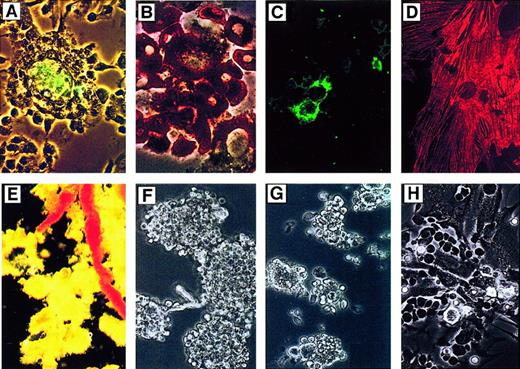
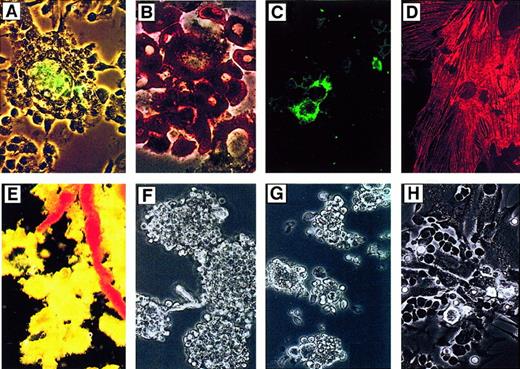
The emergence of multicellular hematon units was assessed in the sediment fraction during microscopic examination and in liquid cultures. Close associations of osteoblasts and hematopoietic cells (mainly macrophages and osteoclasts) could be discerned from E17. These cells were tightly compacted in the alveolar ossicle, from which they could be released but could not form adherent CAs or maintain long-term hematopoiesis in culture (Figure 3A-D). Hematon complexes emerged and could be purified and counted in the femora of mice from day 7 to day 8, after 1g sedimentation of mechanically dissociated femoral shafts. The number of hematons increased rapidly with age and reached steady values from day 35 to day 48 (Figure 2). In native isolates many hematons are joined together, resembling a bunch of grapes, by fine capillaries (Figure 3E-F) but are, however, disrupted during mild mechanical shearing. Further disruption through a 30-gauge needle was used to obtain the most compact core of hematons (Figure 3G) that form CAs in liquid culture (Figure 3H).
Adherent cells in LTC from newborn femur (A-D) and features of hematon preparations from young adult mice (E-H).
Cultured marrow from newborn femur contains several adherent cell types but lacks hematopoietic foci containing CA. (A) Osteocalcine-positive osteoblasts surrounded by hematopoietic cells. (B) A tartrate-resistant acid phosphatase–positive giant, multinuclear osteoclast surrounded by macrophages. (C) Cell island containing MMP-9/gelatinase-B–positive cells. (D) Firmly adherent αSM-actin–positive stroma cells at day 14 in culture. In young adult marrow, hematons resemble a bunch of grapes around capillaries after removal of the bulk buffy coat suspension. (E) Stereomicroscope view. (F) Phase-contrast microscope view. (G) Purified fraction of the hematon core complex. (H) More than 90% of core complexes develop in native CA at days 2 to 7 in culture.
Adherent cells in LTC from newborn femur (A-D) and features of hematon preparations from young adult mice (E-H).
Cultured marrow from newborn femur contains several adherent cell types but lacks hematopoietic foci containing CA. (A) Osteocalcine-positive osteoblasts surrounded by hematopoietic cells. (B) A tartrate-resistant acid phosphatase–positive giant, multinuclear osteoclast surrounded by macrophages. (C) Cell island containing MMP-9/gelatinase-B–positive cells. (D) Firmly adherent αSM-actin–positive stroma cells at day 14 in culture. In young adult marrow, hematons resemble a bunch of grapes around capillaries after removal of the bulk buffy coat suspension. (E) Stereomicroscope view. (F) Phase-contrast microscope view. (G) Purified fraction of the hematon core complex. (H) More than 90% of core complexes develop in native CA at days 2 to 7 in culture.
In adult mice 5% to 10% of BM cells in a femur form the hematon aggregate fraction, whereas most cells constitute the buffy coat suspension.39,40 45 In young adult mice the frequency of day 7 LTC-IC/CAFC was 1/2200 in the hematon and 1/9000 in the buffy coat, and the frequency of day 35 LTC-IC/CAFC was 1/6800 in the hematon and 1/22 000 in the buffy coat fraction (n = 5; 3.7- ± to 1.2-fold enrichment;P < .01). However, there were approximately twice as many LTC-IC/CAFC per femur in the buffy coat (Table1).
Gain of stromal cell competence correlates with hematon emergence in the bone marrow
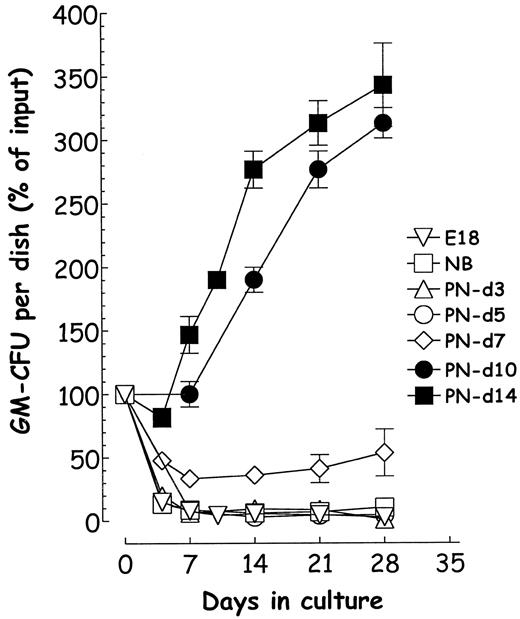
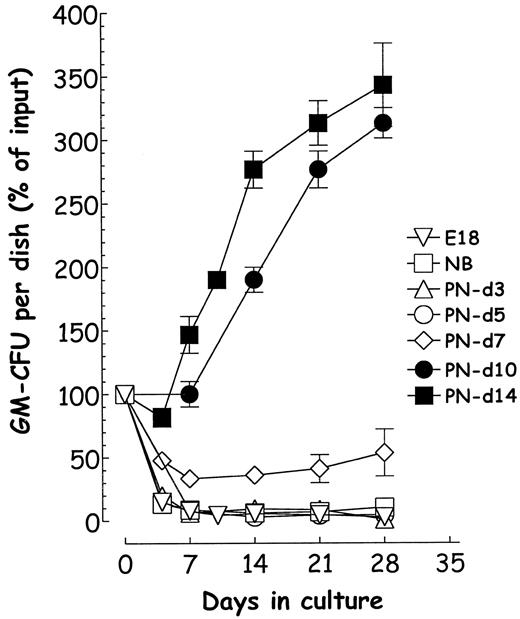
Because blood carries progenitor cells, the presence of hematopoietic cells in the femur between E17 and postnatal day 2 does not prove that these arise locally from previously seeded HSCs. First, LTBMC that imitates many functional aspects of in vivo hematopoiesis was used to assess the competence of femoral BM during ontogenesis. The expansion of TNCs and GM-CFU populations in LTBMC was observed over time. Figure 4 shows that the femoral shaft taken from fetuses or mice until day 5 was not able to sustain the expansion of hematopoietic progenitor cells in culture. Femoral BM cells gained autonomous hematopoietic competence from day 5 to day 8. This function was correlated with the emergence in the femur of compact hematon units containing native CA-forming cell complexes.
Developmental age-related gain of autonomous cell production ability in the femur.
Total cells from femora were dissociated and seeded in triplicate LTCs, and nucleated cells, GM-CFU, and HPP-CFC were measured over time. All 3 cell populations declined rapidly between E17 through day 5. Productive cultures were obtained only from mice aged older than 7 days. E18 (▿), NB (■), postnatal (PN) day 5 (○), day 7 (◊), day 14 (■).
Developmental age-related gain of autonomous cell production ability in the femur.
Total cells from femora were dissociated and seeded in triplicate LTCs, and nucleated cells, GM-CFU, and HPP-CFC were measured over time. All 3 cell populations declined rapidly between E17 through day 5. Productive cultures were obtained only from mice aged older than 7 days. E18 (▿), NB (■), postnatal (PN) day 5 (○), day 7 (◊), day 14 (■).
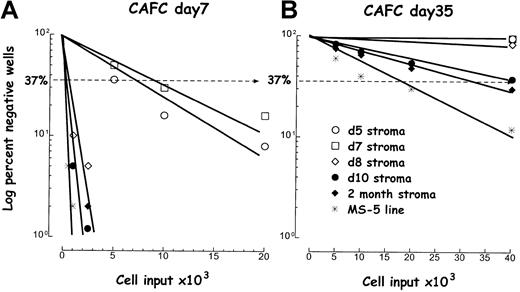
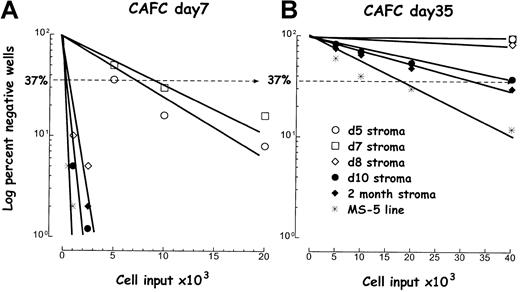
Next, we addressed whether competence acquisition resulted from a gain of stromal cell function or from HSC homing. Stromal feeder layers were prepared from 5-, 7-, 8-, and 10-day-old and 2-month-old femora, and their competence was determined by LDA using BM progenitor cells. Stromal cells established from the femur before day 8 supported poorly the proliferation of late day 7 CAFC (Figure5A) and could not support the long-term expansion of primitive day 35 LTC-IC/CAFC (Figure 5B). These results indicate that until day 5, the lack of competent stromal cells or their putative progenitors may represent a limiting factor for HSC seeding, expansion, or both. This stage corresponds to the onset of HSC (day 35 LTC-IC) seeding and expansion in the femur (Figure 2).
Age-related gain of stromal cell competence.
Stromal layers were prepared from the femur at different ages, then their capacity to support day 7 CAFC and day 35 LTC-IC/CAFC from normal marrow was compared using LDA. Single-cell suspensions of reporter cells were seeded in 24 replicates at each of the 4 dilutions. Log percentage of wells negative for CAFC are plotted against initial cell input and 1× values were intrapolated at the −37% value. (A) Day 7 CAFC. (B) Day 35 LTC-IC/CAFC. Symbols represent stromal cells prepared at different postnatal ages: day 5 (○), day 7 (■), day 8 (⋄), day 10 (●), 2 months (⧫). The MS-5 cell line (*) was used as a control reference.
Age-related gain of stromal cell competence.
Stromal layers were prepared from the femur at different ages, then their capacity to support day 7 CAFC and day 35 LTC-IC/CAFC from normal marrow was compared using LDA. Single-cell suspensions of reporter cells were seeded in 24 replicates at each of the 4 dilutions. Log percentage of wells negative for CAFC are plotted against initial cell input and 1× values were intrapolated at the −37% value. (A) Day 7 CAFC. (B) Day 35 LTC-IC/CAFC. Symbols represent stromal cells prepared at different postnatal ages: day 5 (○), day 7 (■), day 8 (⋄), day 10 (●), 2 months (⧫). The MS-5 cell line (*) was used as a control reference.
The hematon has higher cell-production ability than the buffy coat in LTC
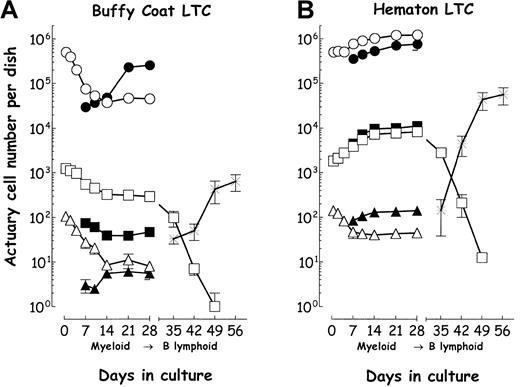
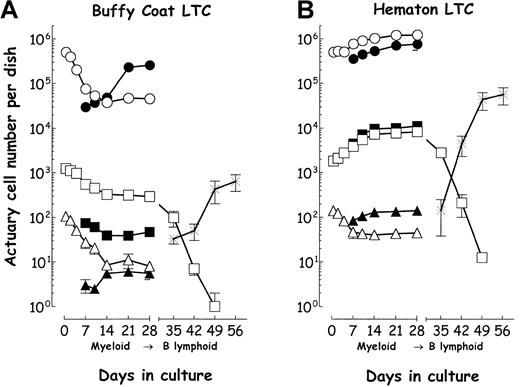
Relative richness of the hematon in stromal cell-associated progenitor cells suggested that it produced more progenitor cells in standard LTBMC over time. Aliquots (5 × 105 cells) of the buffy coat and hematon fractions were seeded in 2 mL LTC medium. Although there were initially fewer primary F-CFU in the buffy coat cultures, both cell fractions developed a semiconfluent layer after 8 to 10 days. Cell vitality studies using annexin V/PI double-labeling showed that double-labeled apoptotic bodies accounted for 5% to 15% during the first week in both culture systems. The TNC, GM-CFU, and HPP-CFC populations in the nonadherent and adherent cell compartments were monitored. TNC and GM-CFU declined in the nonadherent fraction, but those in the adherent layer of the buffy coat cultures gradually expanded (Figure 6A); those in both compartments expanded in hematon cultures (Figure 6B). Hematon cultures generated 6 times more nucleated cells, 16 times more HPP-CFC, 55 times more GM-CFU, and 18 times more BFU-E (not shown) than did the buffy coat on day 28 in culture.
Myelopoietic and B-lymphopoietic capacity of buffy coat and hematon in LTC.
TNC and CFU were determined from the nonadherent (NA) and adherent cell fractions (AD). Buffy coat (A) and hematon (B) cultures. Commutation from myelopoiesis (Dexter conditions) to B lymphopoiesis (Whitlock-Witte conditions) in LTC was measured by analyzing the GM-CFU and B220+ cell populations. TNC-NA (○), TNC-AD (●), GM-CFU-NA (■), GM-CFU-AD (▪), HPP-CFC-NA (▵), HPP-CFC-AD (▴), B220+ B lymphocytes (*). Representative experiments repeated 3 times with similar results are shown. Data points represent the mean (±1 SEM) of 4 determinations.
Myelopoietic and B-lymphopoietic capacity of buffy coat and hematon in LTC.
TNC and CFU were determined from the nonadherent (NA) and adherent cell fractions (AD). Buffy coat (A) and hematon (B) cultures. Commutation from myelopoiesis (Dexter conditions) to B lymphopoiesis (Whitlock-Witte conditions) in LTC was measured by analyzing the GM-CFU and B220+ cell populations. TNC-NA (○), TNC-AD (●), GM-CFU-NA (■), GM-CFU-AD (▪), HPP-CFC-NA (▵), HPP-CFC-AD (▴), B220+ B lymphocytes (*). Representative experiments repeated 3 times with similar results are shown. Data points represent the mean (±1 SEM) of 4 determinations.
Development of B cells from the hematon in myelopoietic-lymphopoietic switch cultures
The development of B lymphocytes in LTC was studied to quantify putative HSCs in the buffy coat and hematon fractions. B lymphocytes rapidly die in myeloid LTBMC containing hydrocortisone, but HSCs survive for several weeks and can be commuted to B-cell development. For 4 weeks 2 × 106 cells were maintained in myeloid LTC at 33°C, then adherent layers were washed and cultures were maintained in B-lymphocyte culture medium at 37°C. B lymphocytes emerged in both buffy coat (Figure 6A) and hematon (Figure 6B) cultures, but there were 8.6 ± 2.4 times more B lymphocytes (B220+) in the hematon cultures than in the buffy coat after 21 days (n = 4; P < .001). B lymphocytes appeared in CAs shortly after commutation but later spread over and under a larger number of stromal cells. Immunostaining in situ was used to further characterize developing B cells. Oct-2 and Hox-11 were detected in B cells that expanded over stromal cells 7 days after commutation, but there were only few positive cells among those that grew under stromal cells (not shown).
Isolation and analysis of native hematon core complexes
The hematon core complex was isolated on dissociation through a 30-gauge needle. This technique produced approximately 1500 to 2000 tiny cell aggregates (20-50 cells per aggregate), which corresponded to approximately 30 to 50 × 103 cells in a femur. This fraction contained almost all native, early, developing day 7 CA and 30 times more day 14 CA than did the buffy coat suspension.
The functional heterogeneity of hematon core complexes in day 8 mice and in young adults was analyzed using individual organ microcultures. In day 8 femora 52% ± 8% (n = 3) of hematons contained the core complex that yielded 3 ± 1.5 (range, 1-5) native CA by day 7. In the adult, 87% ± 5% of microaggregates (n = 6) developed native CA by day 7; however, the number of core complexes per hematon was similar to what it was in the day 8 femur (3.2 ± 1.5; range, 1-6). The percentage of core complexes that remained productive for more than 35 days was 35% ± 10% in day 8 femora and 56% ± 12% in adult femora.
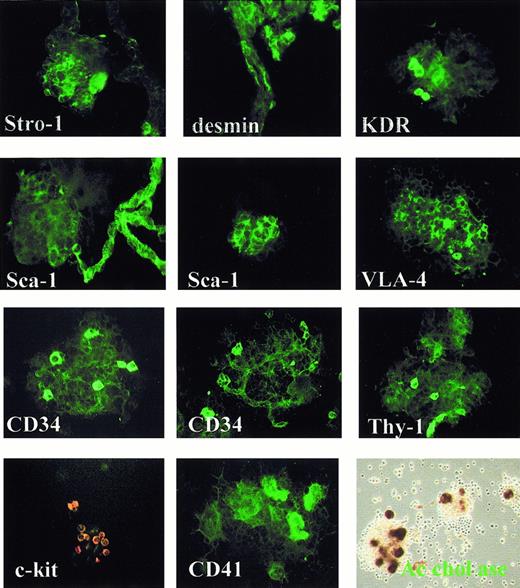
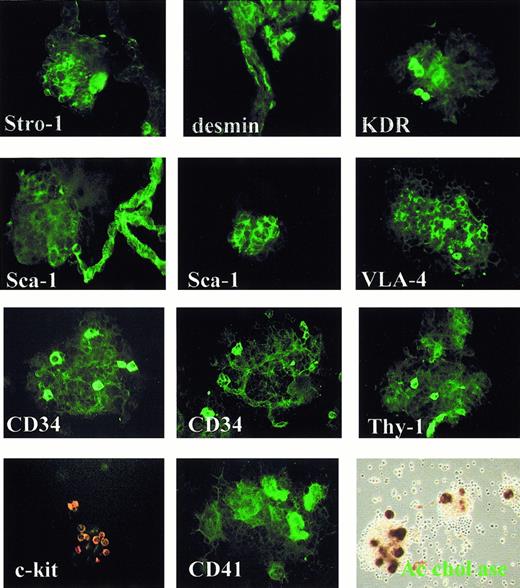
Immunostaining showed distinct stromal cells building up hematons—Stro-1+ mesenchymal cells, desmin+perivascular preadipocytes, Flk-1+, Sca-1+, and CD34+ vascular endothelium, and MMP-9+macrophages at discrete locations within or in intimate association with the hematon core complex. The high concentration of Sca-1+, CD117/c-kit+, Thy-1+, CD34+, and CD41+ hematopoietic cells further indicates the presence of early progenitor cells in the hematon (Figure7).
Stromal and hematopoietic cell composition of the hematon core complex.
The hematon core complex fraction was purified from young adult mice, washed in PBS/0.5% BSA/0.1% Na azide, and cytocentrifuged. Immunostaining of native preparations with antibodies to Stro-1, desmin, Flk-1, Sca-1, VLA-4, CD34, Thy-1, c-kit, CD41, and acetylcholinesterase reaction on adherent core complexes at day 4 in culture show the discrete localization of cells within the hematon core complex or in close contact with the vascular endothelium.
Stromal and hematopoietic cell composition of the hematon core complex.
The hematon core complex fraction was purified from young adult mice, washed in PBS/0.5% BSA/0.1% Na azide, and cytocentrifuged. Immunostaining of native preparations with antibodies to Stro-1, desmin, Flk-1, Sca-1, VLA-4, CD34, Thy-1, c-kit, CD41, and acetylcholinesterase reaction on adherent core complexes at day 4 in culture show the discrete localization of cells within the hematon core complex or in close contact with the vascular endothelium.
Discussion
During the past decade major progress has been achieved in the elucidation of the emergence, development, and function of primitive and adult-type HSCs in avian11,53 and mammalian ontogeny.9,12-15,17,46-48 The cellular mechanisms and molecular stimuli that determine gain of autonomous hematopoietic activity in bone cavities remain, however, unidentified. Decipherment of the BM fate map during ontogeny and identification of specific territories in which stromal cells interact with HSCs is hampered by the lack of a technique permitting the isolation, quantification, and functional characterization of native stromal–hematopoietic cell complexes. Yet it was shown previously that adult BM contains the hematon, a cohort of preformed aggregates of stromal cells and hematopoietic progenitors.38-40
We investigated the development of fetal and early postnatal mouse marrow, with special reference to hematon emergence, and established, first, that chondrogenesis, endochondral bone formation, and the formation of a primary, vascularized spongy bone shaft occur in sequence and clearly before the onset of autonomous hematopoiesis. Our study results confirm a gradual increase in GM-CFU and day 7 CAFC numbers in the femur, starting from E17.8 Surprisingly, however, day 35 LTC-IC/CAFC were not detectable by LDA (using the MS-5 stroma cell line as a support) until 2 days after birth, and long-term culture femur marrow cells could not sustain hematopoiesis in Dexter culture until approximately 5 days after birth. Such cultures contained chondrocytes, vascular endothelial cells, osteoblasts, osteoclasts, and adherent colony-forming macrophages that expanded slowly over time but failed to switch to a productive stage. Earlier works postulated that marrow hematopoiesis starts by HSC seeding to the femora at E17.8,9,21,49 BM stroma from newborn mice did maintain the expansion of adult GM-CFU in LTBMC, but this activity was approximately 4 times weaker than in adult stroma.50,51 Our own results clearly show that day 5 to day 7 stroma could not support day 35 LTC-IC/CAFC growth, which is in contrast to day 8, day 10, and adult stroma that had gained this functional activity. These observations argue against the development of stromal cell–associated hematopoietic stem cells in the bone marrow until approximately day 5. Increasing CFU numbers encountered in the femur between E17 and day 5 may therefore reflect blood volume enlargement caused by the development of marrow vasculature rather than true marrow seeding by HSCs. The fetal bloodstream indeed carries stem cells, clonogenic progenitors,49 52 and monocytes/macrophages that play a role in tissue remodeling. Committed progenitors may seed the fetal and early postnatal marrow and establish a first line of terminal hematopoiesis therein before true stem cells colonize bone cavities after the first week of life.
The spongy bone that develops transitorily during limb formation at the metaphysis provides a base plate for the development of BM tissue. MMP-9–gelatinase B is a key regulator of growth plate angiogenesis and chondrocyte apoptosis,53 and VEGF, secreted by hypertrophic chondrocytes, couples cartilage remodeling, ossification, and angiogenesis during endochondral bone formation.19Interestingly, Flt-1 activation in monocytes is associated with chemotaxis.54 This mechanism may explain invasion of the femur by primitive macrophages and chondroclast-osteoclast progenitors at a very early stage of endochondral ossification.18These data and our results suggest at this time that enzymes involved in osteolysis and lysis of matrix proteins prevent the formation of marrow microenvironment.
Second, we documented in this study that the acquisition of autonomous hematopoietic competence in BM is not continuous but that it coincides with the cessation of hematopoiesis in the liver.8Importantly, this gain of BM function is correlated with the emergence of hematon units in the femur, the enumeration for which we have developed a quantitative assay. Once compact hematon particles emerge at days 5 to 7, their number rapidly reaches a near plateau value, indicating that BM gain of function follows a stepwise “one-hit” kinetics. This suggests that one or several cell types migrate to the femora at a well-defined developmental stage and that resultant cell-cell interactions play an inductive role in the organization of specialized HSC regulatory territories. Stereomicroscopic observations of the BM shaft, prepared by careful microdissection and mild erosion, revealed the intimate association of hematons with the vasculature (Figure 2D-F). Immunostaining showed overlapping expression patterns of several cell markers—Sca-1, CD34, or Flk-1—on both hematopoietic and vascular endothelial cells (Figure 7). Thus, the development of definitive BM tissue and the emergence of hematons may be dictated by a budding/branching-type morphogenetic processus55 whose exact cellular mechanism and molecular control remain to be elucidated.
Third, quantitative analysis of buffy coat suspensions and hematon fractions in young adult mice indicates that though the latter contains fewer cells (5%-10% of TNC in a femur), hematons enclose a wide spectrum of stromal cell–associated HSC/multipotent hematopoietic progenitor cells and almost all native CA-forming cells. The hematon core complex may be a primordial niche in BM because it can generate hematopoietic progenitor cells autonomously in long-term microculture in the absence of irradiated feeder cells and any “community effect” from neighboring cells.
The cell production capacity of buffy coat and hematon fractions was assessed in LTBMC. The hematon generated 55 times more GM-CFU and 15 times more HPP-CFC than did the buffy coat on day 28 of LTC. Mouse LTBMC provides a tool to study the commutation of myelopoiesis to B lymphopoiesis at the level of primitive HSCs.44,56 In the current experiments, hematon LTC generated 8 times more B lymphocytes than did the buffy coat cultures 3 weeks after commutation. Funk et al45 detected no significant difference in early B-lymphocyte colony-forming potential among BM aggregate and suspension fractions immediately after isolation. Because committed B-cell progenitors rapidly die in myeloid LTC conditions, our results indicate that the hematon contains more stromal cell–associated myelopoietic-lymphopoietic HSCs than does the buffy coat fraction.
Restricted location of hemopoietic niches (native CA), greater frequency of LTC-IC/CAFC, and presence of common myelopoietic-lymphopoietic HSCs in the hematon explain the higher cell production observed in hematon LTC than in buffy coat LTC and suggest that stromal cells in the hematon provide specific factors that control the expansion and differentiation of HSC/multipotential hematopoietic cells. These specialized niches are limited in number, so they may constitute a rate-limiting regulatory system in maintaining HSC self-renewal and commitment. Our data support earlier notions suggesting that specific regulatory territories for HSC/hematopoietic progenitor cells exist30 and are saturable in the femur.33
This study also implies that the technique used for BM recovery and dissociation before quantitative analysis may significantly influence the outcome of experiments—removal of the aggregate fraction by filtration eliminates more than 50% of stromal cells, nearly 100% of stromal cell–associated progenitor cells, and approximately 30% of total HSCs (LTC-IC/CAFC, day 35). Isolation of hemopoietic niches from the hematons by limited erosion and the use of short-term microculture systems provide a tool for further analysis of the role of stromal cells in the control of HSC functions, such as asymmetric cell division, expansion, and differentiation commitment.
Acknowledgments
We thank Dr Paul Kincade (Oklahoma Cancer Center, Oklahoma City, OK), Dr Nydia G. Testa (Paterson Institute for Cancer Research, Manchester, United Kingdom), Dr Georges Uzan and Dr Michèle Souyri (INSERM U-506), and Dr Jean-Paul Thièry (CHB, Hôpital Paul Brousse, Villejuif) for helpful discussions. We also thank Dr Laure Coulombel (Hôpital Cochin, Paris) for kindly providing the MS-5 stroma cell line and Dr Pierre Charbord (INSERM U 506) for help with antibodies to Stro-1.
Supported in part by Institut du Cancer et d'Immunogénétique grants 07/1998 and 03/1999 and by subventions from Hôpital Paul Brousse and from Université Paris-Sud XI, UFR Kremlin-Bicêtre. Supported also by a grant from the Groupe d'Etude Hémostase et Thrombose (J.C.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Istvàn Blazsek, INSERM Unité506, Hôpital Paul Brousse, 12-14, Avenue Paul Vaillant-Couturier, 94807 Villejuif Cedex, France; e-mail:U506@infobiogen.fr.