Abstract
Hereditary atransferrinemia is a rare but instructive disorder that has previously been reported in only 8 patients in 6 families. It is characterized by microcytic anemia and by iron loading, and can be treated effectively by plasma infusions. We now report the first case known in the United States. We determined the sequences flanking the exons of the human transferrin gene and sequenced all of the exons and some of the flanking regions of the patient's DNA and that of her parents. The patient's DNA revealed a 10-base pair (bp) deletion, followed by a 9-bp insertion of a duplicated sequence. There was also a G→C transversion at complementary DNA (cDNA) nt 1429, predicting that a proline was substituted for the alanine in amino acid position 477 (Ala 477 Pro). The latter mutation occurs at an evolutionarily highly conserved site; 704 control alleles were screened and this point mutation was not found. Each of the patient's transferrin genes contains one mutation, ie, the patient is a compound heterozygote for these mutations, because one was found in each of her parents. In addition to these mutations, which we regard to be causative in the patient's atransferrinemia, a silent polymorphism at cDNA 1572 G→C was found in exon 13 as well as 2 previously unreported polymorphisms at IVS8 + 62 c→t and IVS14-4 c→a. The mutation in nt 1572 and that in intron 8 were common in the general population; the intron 14 mutation is rare.
Introduction
Atransferrinemia is a rare hereditary disorder characterized by iron overload and hypochromic anemia. The molecular basis of the deficiency of transferrin that occurs in this disease has not heretofore been identified in human patients, and the sequence of the human transferrin gene has not been determined. We now report the results of molecular analysis of the only patient known to us with this disease in the United States, and identify some previously unknown polymorphisms in the gene.
Patient, materials, and methods
Clinical history
A white woman, then 20 years of age, was first seen by one of us (V.F.F.) in March of 1984. She had been having heavy menstrual bleeding, lasting 5 days and had been treated with ferrous gluconate, 320 mg thrice daily from August 1982 to July 1983. In February 1984, she was examined by Dr E. Greenberg, of Carle Clinic, Urbana, IL, who found microcytic anemia, elevated serum ferritin, and “exceedingly low” serum transferrin. He referred her to the Mayo Clinic for further studies. Before 1983, she had not been known to be anemic; however, there was no record of prior blood tests. She had received no transfusions. In addition, she had previously been diagnosed with hypothyroidism, for which she was takingl-thyroxine. No other family members were known to have anemia.
Physical examination was unremarkable except for mild pallor. Laboratory examination in 1984 revealed hemoglobin concentration 10.6 g/dL, red blood count 4.46 × 1012/L Hct 32%, MCV 75.3 fL, serum iron concentration 15 μg/dL, serum total iron binding capacity 23 μg/dL, serum ferritin concentration greater than 2500 μg/L (in 1983 one ferritin level of 7500 μg/L had been recorded). No transferrin could be detected by radial diffusion in an Ouchterlony plate. A value of thyrotropic hormone (TSH) elevated to 11.9 mU/L and a total thyroxine of 3.8 μg/dL were consistent with the diagnosis of hypothyroidism. Serum transaminases AST and ALT were normal. Liver biopsy had been performed elsewhere and the specimen was reviewed at the Mayo Clinic. It showed marked hemosiderosis, especially of hepatocytes and Kupffer cells, without portal involvement, and was interpreted as suggestive of primary hemochromatosis in a precirrhotic phase. Hepatic iron concentration was 37 465 μg/g dry weight, or 670.85 μmol/L per gram giving a hepatic iron index of 35.3 (Normal less than 2). She had no arrhythmias and her cardiac silhouette showed no cardiomegaly.
A diagnosis of congenital atransferrinemia with iron overload was made. The hypothyroidism was ascribed to the iron overload. She was started on a program of monthly infusions of 500 mL of normal human plasma immediately preceded by removal of 480 mL of blood. This program provided sufficient transferrin to permit normal hemoglobin formation in a cohort of erythrocytes, and removal of excess iron by phlebotomy. To minimize risk of blood-transmitted viral pathogens, a small group of donors was recruited to serve as sources of plasma. During the ensuing 10 years she underwent this treatment monthly, with removal of 57.6 L of blood, estimated to contain 6.92 kg of hemoglobin, and 23.5 g of iron. Her venous blood hemoglobin concentration was tested before each phlebotomy, and was, on average, 12 g/dL. Despite considerable symptomatic improvement, in relief of fatigue, she became amenorrheic and by age 30 she exhibited marked osteoporosis, for which she was treated with a cyclic estrogen/progesterone combination, with subsequent relief of bone pain.
Fatigue and anemia recurred (hemoglobin concentration 10 g/dL) and she was found to have serum ferritin concentration less than 5 μg/L. The phlebotomy program was discontinued, and she was given a short course of oral iron, with symptomatic relief and increase of hemoglobin concentration to 12 g/dL. Examination of specimens from the patient's parents indicated approximately half-normal serum transferrin concentrations.
Attempts to obtain purified human transferrin from several sources were unsuccessful. However, the monthly plasma infusions have been successful in alleviating the fatigue and the anemia, and permitting the removal of the excess iron. Now, at age 36, the patient is nearly asymptomatic. However, she remains amenorrheic.
Determination of transferrin intron sequences
A human genomic library from placenta in Lambda FIX II vector (Stratagene, La Jolla, CA) was screened with human transferrin complementary DNA (cDNA) to obtain clones for analysis of the intron/exon borders of the transferrin gene. The positive clones obtained were amplified with Expand Long Template Polymerase Chain Reaction (PCR) System (Boehringer Mannheim, Indianapolis, IN) using cDNA primers (GenBank Accession M12530) or primers corresponding to genomic sequences (GenBank Accession M15673, M21569, M21570, X76338,X76339, X76340, and AF058327). The amplified fragments were sequenced to obtain extensive intron sequence so that oligonucleotide primers could be made to amplify genomic DNA from the patient and controls.
Sequencing of the transferrin coding region
Genomic DNA was isolated from peripheral blood leukocytes by standard methods with informed consent. Amplification of all the transferrin exons were carried out by PCR on DNA from the patient and from a control. The oligonucleotide amplification primers used for each exon are listed in Table 1. The 50-μL PCR reaction contained 33.5 mmol/L Tris-HCl pH 8.8, 8.3 mmol/L (NH4)2SO4, 3.35 mmol/L MgCl2, 85μg/mL bovine serum albumin, 0.25 mmol/L dNTPs, 1.5 U Taq polymerase, and 0.5μg DNA. PCR was performed for 30 cycles consisting of 93°C for 30 seconds, 58C for 30 seconds, and 72C for 30 seconds, followed by a 7-minute 72C extension time. After amplification the PCR product was purified with a QIAquick PCR Purification Kit (Qiagen Inc, Chatsworth, CA) and sequenced on an Applied Biosystems Inc (Foster City, CA) automatic sequencer.
Allele Specific Oligonucleotide Hybridization (ASOH) was used to screen 352 control DNA samples for the missense mutation 1429 G→C found in exon 12 of the patient. Eighty-three control DNA samples were examined for the 3 newly identified intronic and silent exonic mutations to establish their gene frequencies.
Results
Fourteen positive clones from the human genomic placenta library were obtained. Additional intronic sequence from these clones has been deposited into GenBank Accession numbers AF288139-44, AF294270-71. Introns 3, 4, 5, 6, 8, 10 and 11, and 15 have been sequenced in their entirety.
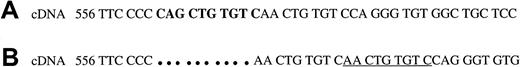
The entire coding region and all flanking intronic regions were sequenced in the patient. The patient's DNA was found to have 2 mutations. The first located in exon 5 was a 10-base pair (bp) deletion cDNA 562-571del, followed by a 9-bp duplication cDNA 572-580. Figure1 diagrams this rearrangement. A termination codon results 27 amino acids downstream. The second mutation was found in exon 12 and was a G→C transversion at cDNA 1429, causing a proline to be substituted for an alanine at amino acid 477 (Ala 477 Pro). The transferrin gene has been shown to be very polymorphic1 2 and to confirm that the nt 1429 transversion was not a common polymorphism, 704 control alleles were screened for the presence of this mutation. All were found to have the normal sequence at this position.
The normal sequence of exon 5 of the transferrin gene and the rearrangement found in the patient with atransferrinemia.
Comparison of the normal sequence of exon 5 of the transferrin gene (A) and the rearrangement found in the patient with atransferrinemia (B). The 10-bp sequence that is deleted from the mutant gene, cDNA 562-571, is shown in bold in the normal sequence. The 9-bp duplication that has been inserted into the mutant gene is underlined. The rearrangement leads to a frameshift and an early termination.
The normal sequence of exon 5 of the transferrin gene and the rearrangement found in the patient with atransferrinemia.
Comparison of the normal sequence of exon 5 of the transferrin gene (A) and the rearrangement found in the patient with atransferrinemia (B). The 10-bp sequence that is deleted from the mutant gene, cDNA 562-571, is shown in bold in the normal sequence. The 9-bp duplication that has been inserted into the mutant gene is underlined. The rearrangement leads to a frameshift and an early termination.
An additional silent polymorphism at cDNA 1572 G→C (Leu 524 Leu) was found in exon 13 of the patient but not in the concurrent control sample. Two previously unreported polymorphisms in intervening sequences were also found in the patient. The patient was heterozygous at these positions, IVS8 + 62 c→t and IVS14-4 c→a. The latter mutation is apparently uncommon. It was present in the patient's mother, but no other examples were found among 72 white subjects, 4 African-Americans, or 7 Asians. It does not have a negative effect on the splice consensus. On the other hand, the cDNA 1572 and the IVS8 + 62 c→t polymorphisms proved to be common with cDNA 1572G→C, having a frequency of 0.254 and IVS8 + 62 c→t one of 0.354.
Examination of DNA from the parents of the patient showed that her mother had the exon 5 rearrangement (10-bp del, 9-bp duplication) and the father had the cDNA 1429 G6C mutation, indicating that they were in trans in the patient.
Discussion
In 1961, Heilmeyer and coworkers3 described atransferrinemia in a young girl with severe hypochromic anemia and marked, generalized iron overload. Table2 summarizes the cases that have been documented. A hypotransferrinemic mouse (trf[hpx]), a mutant strain exhibiting transferrin deficiency, marked anemia, hyperabsorption of iron, and elevated hepatic iron has also been described.4It has been known for more than a decade that a splicing abnormality was present in these mice,5 and the mutation and the splice site mutation has recently been identified.6Although the mutation is slightly “leaky,” ie, a small amount of gene product appears to be made, the homozygous animals generally survive less than 2 weeks if not treated.6
Because transferrin functions to deliver iron to the developing erythron, as well as to other tissues, atransferrinemia results in reduced delivery of iron to the marrow and reduced hemoglobin synthesis. The predominant clinical features of the deficiency are pallor and fatigue. Some patients have mild hepatomegaly. Two patients died at age 7 from refractory congestive heart failure. The autopsy in both showed marked hemosiderosis and fibrosis of liver, pancreas, thyroid, myocardium, and kidneys, but no iron in the marrow. Both of these patients had received numerous transfusions. An increased number of infections appears to occur in patients with atransferrinemia; Heilmeyer's patient had recurrent infections, and another patient died of pneumonia.
During the time that excess iron is accumulating in the body, before replacement therapy, there is increased iron absorption from the gastrointestinal tract, accelerated plasma iron clearance, and diminished incorporation of iron into hemoglobin (ranging from 7% to 55%; normal 30% to 100%).7,8 In our patient and in others who have been reported, the infusion of either normal plasma or purified apotransferrin was followed in 10 to 14 days by reticulocytosis and then by a rise in hemoglobin concentration. The 2 Japanese patients had been given 1 to 2 g of highly purified apotransferrin intravenously every 3 to 4 months for 4 to 7 years with good effect and without the development of antitransferrin antibodies.9 The Slovak patient was also given apotransferrin infusions and desferrioxamine to remove excess iron. This patient now has arthropathy and siderosis of synovial membranes. The use of purified transferrin reduces the risk of hepatitis that would attend infusion of whole plasma. If this therapy is repeated once or twice monthly, the patient becomes hematologically normal within a few months, although iron stores and serum ferritin concentration remain elevated. This response permits removal of excess iron by phlebotomy.
Acquired forms of atransferrinemia have been described in association with the nephrotic syndrome10,11 and in a patient with erythroleukemia.12 One patient has been described with a functional disorder of transferrin due to transferrin-IgG-antitransferrin immune complexes.13
Because transferrin is expressed almost entirely in the liver, cDNA is generally not available. Therefore, sequencing the transferrin coding sequence requires that the genomic DNA sequences flanking the exons be known. Having determined these, we were able to sequence the coding sequence and intronic/exon junctions of the patient's DNA, and we found 2 mutations. One of these was a deletion that created a frame shift. There can be no doubt that this mutation would result in a null transferrin allele. The other mutation, predicting an alanine-to-proline amino acid substitution, is a nonconservative change that could well have a major functional effect on transferrin. Notably, the alanine normally present at this position was conserved not only in all species in which the serum transferrin sequence was known, including the rat,14rabbit,15 horse,16 pig,17 and bull (Medline accession #U02564), but even lactoferrin from species including the buffalo18 and goat.19 Because no other mutation was found, we conclude that this patient was a compound heterozygote for these 2 mutations and that this resulted in the virtual absence of serum transferrin and the clinical syndrome, which is associated with this deficiency. One may speculate that the substitution of proline for alanine results in the synthesis of a defective protein that is unstable, so that little transferrin antigen appeared in the serum of our patient. The relatively mild course and late onset of clinical manifestations in our patient might suggest that the mutation was indeed “leaky” and that some functional transferrin, albeit below the limits of detection, was present.
Supported by grants DK53505-02 and HL 25552-10 and RR00833 from the National Institutes of Health, and funds from the Stein Endowment Fund.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
E. Beutler, The Scripps Research Institute, 10550 N Torrey Pines Rd, La Jolla, CA 92037; email: beutler@scripps.edu.