Abstract
Approximately 20% of B-lineage acute lymphoblastic leukemias are not cured by traditional chemotherapy. The possibility was examined that residual leukemic cells that potentially contribute to relapse are harbored in association with fibroblastic stromal cells in the bone marrow. Modulation of cytarabine (Ara-C) and etoposide (VP-16) efficacy by bone marrow stromal cells in vitro was investigated. Stromal cell coculture was shown to sustain the proliferation of B-lineage leukemic cells and to reduce leukemic cell apoptosis when exposed to Ara-C or VP-16. Direct contact with stromal cells was essential for the protection of leukemic cells during chemotherapy, whereas soluble factors had negligible effect. Specifically, signaling mediated through interaction with the stromal cell adhesion molecule VCAM-1 was required to maintain the maximum viability of leukemic cells during Ara-C and VP-16 exposure. In contrast, the interaction of leukemic cells with fibronectin did not confer significant resistance to either chemotherapeutic agent. These observations suggest a role for the bone marrow microenvironment in modulating the response of B-lineage leukemic cells to Ara-C or VP-16, and they indicate specific molecular interactions that may be important in determining the sensitivity of leukemic cells to treatment.
Introduction
Acute lymphoblastic leukemia (ALL) is a disease that initiates and progresses in the bone marrow. The marrow microenvironment is presumed to play an essential regulatory role in the development of this cancer. In addition, the bone marrow microenvironment provides a primary site in which residual leukemic cells may survive standard chemotherapy.1 2 After treatment, surviving cells contribute to relapse and to poor prognosis of patients for whom ALL is not successfully eradicated by traditional chemotherapy. The role of bone marrow stromal cells in modulating the response of leukemic cells to chemotherapy has not been previously investigated.
Stromal cells influence the development of hematopoietic cells through the production of cytokines and through the signals mediated by direct contact of progenitor cells with stromal cells. The stromal cell adhesion molecules VCAM-1 and fibronectin have been identified as 2 of the critical molecules necessary for the adhesion of progenitors to stromal cells.3-6 Many of the developmental cues provided by stromal cells to normal hematopoietic progenitor cells have also been shown to impact the survival and expansion of leukemic cells. Like their normal counterparts, many B-lineage ALL cells express VLA-4, which can interact with VCAM-1 and fibronectin on the surfaces of stromal cells.7 Primary ALL cells isolated from patients maintain the greatest viability when in direct coculture with an adherent stromal cell layer, and this effect is not duplicated by stromal cell-conditioned medium.8 The optimal survival of leukemic cells through direct interaction with stromal cells indicates signals mediated through adhesion that cannot be completely substituted by soluble factors.
In the current study, we investigated bone marrow stromal cell modulation of Ara-C– and VP-16–induced cell cycle arrest and apoptosis of the ALL cell lines JM-1, SUP-B15, and RS4. Coculture of B-lineage leukemic cells with stromal cells diminished the effect of both chemotherapeutic agents on cell cycle progression and apoptosis. This effect could be attributed to the interaction of leukemic cells with VCAM-1 but not with fibronectin. These observations suggest a role for bone marrow stromal cells in maintaining leukemic cell division and survival during exposure to chemotherapy, and they are relevant to treatment strategies aimed at minimizing ALL relapse through the reduction of residual leukemic cells in bone marrow.
Materials and methods
Leukemia and bone marrow stromal cell cultures
Growth factor independent cell lines derived from patients with B-lineage acute lymphoblastic leukemia/lymphoma used in this study were obtained from the ATCC (Manassas, VA). The panel of cell lines chosen represented the diversity of phenotypes that characterize common and pre-B ALL. They included JM-1 (#CRL-10423; HLA DR+, CD10+, CD19+, surface Ig −VLA-4+, VLA-5−), RS4 (#CRL-1873; HLA DR+, CD9+, CD24+, VLA-4+, VLA-5+ cytoplasmic and surface Ig−), and SUP-B15 (#CRL-1929; HLA DR+CD5+, CD10+, CD13+CD38+, CD71+, cytoplasmic Ig+, Ph+, VLA-4+, VLA-5+). In addition to the expression of the antigens listed above, RS4 cells contained the (4;11)(q21;23) translocation frequently present in infants younger than 1 year of age with ALL. An additional T-lineage leukemic cell line, Jurkat (ATCC #TIB-152, CD3+, VLA-4+, VLA-5+), was included in viability experiments to evaluate lineage specificity of stromal cell effects. All leukemic cell lines were grown in medium with supplements, as recommended by the ATCC. The establishment of human bone marrow stromal cells by our laboratory has been previously described.9
Chemotherapeutic agents
Ara-C (Sigma, St Louis, MO) was stored at −20 °C at 10 μg/μL and VP-16 (Bristol Laboratories, Princeton, NJ) at a stock concentration of 1 g/50 mL. Both drugs were diluted in Iscove medium immediately before use. Experimental doses of Ara-C (.01-1.0 μg/mL) and VP-16 (1.0-5.0 μmol/L) were used to approximate doses described for use in regimens for acute lymphoblastic leukemia.10
Cell cycle analysis
To evaluate the cell cycle profile of B-lineage leukemic cells in the presence of stromal cells, JM-1 cells were collected after treatment with 5 μmol/L VP-16 or 1.0 μg/mL Ara-C for 24 to 48 hours in the presence or absence of an adherent stromal cell layer. JM-1 cells were fixed in EtOH, treated for 30 minutes with RNase (Sigma), and stained with propidium iodide for DNA analysis.
Evaluation of leukemic cell viability
B-lineage JM-1, RS4, and SUP-B15 or T-lineage Jurkat cells were cultured in medium alone or were cocultured with an adherent layer of bone marrow stromal cells for 24 to 72 hours in the presence or absence of VP-16 (1-5 μmol/L) or Ara-C (0.01-0.1 μg/mL). Leukemic cells were removed from adherent stromal cells by vigorous pipetting. Viability was evaluated by trypan blue exclusion in triplicate samples.
Annexin staining
After 48 and 72 hours of culture in the presence of 1 to 5 μmol/L VP-16 or 0.1 to 1.0 μg/mL Ara-C, JM-1 cells were collected and stained using an Annexin V–fluorescein isothiocyanate (FITC) kit (Genzyme, Cambridge, MA) according to the recommended protocol of the manufacturer to detect apoptotic cells. All treatment groups were established in the presence and absence of an adherent stromal cell layer. As a representative cell line, JM-1 cells were collected on a Becton Dickinson Flow Cytometer, and data analyzed using CellQuest software and cytometer (Becton Dickinson, Mountainview, CA).
Evaluation of JM-1 viability in stromal cell conditioned medium
Conditioned medium was collected from confluent cultures of stromal cells after 72 hours of incubation. JM-1 cells were subsequently cultured in 75% conditioned medium for 24 to 72 hours in the presence or absence of VP-16 (1 and 5 μmol/L) or Ara-C (0.01 and 0.1 μg/mL). Viability was evaluated by trypan blue exclusion in triplicate samples.
Glutaraldehyde fixation of stromal cells
To interrupt the metabolic activity of stromal cells while leaving surface proteins intact, confluent stromal cell layers were treated with glutaraldehyde as previously described.11 12Briefly, confluent stromal cells were treated with 2% glutaraldehyde (FisherChemical, Fair Lawn, NJ) for 5 minutes and rinsed 5 times with fresh medium. Stromal cells were then incubated for 12 hours in medium, rinsed, and incubated an additional 12 hours in fresh medium before the addition of JM-1 cells. Treatment groups included JM-1 cells in medium alone, JM-1 cells in 5 μmol/L VP-16 or 1.0 μg/mL Ara-C, with all groups cocultured with fixed and control stromal cells. After 48 and 72 hours of culture, JM-1 cells were collected, and viability of triplicate samples was evaluated.
Culture of JM-1 and RS4 cells on fibronectin-coated plates
To determine whether interactions with the stromal cell adhesion molecule fibronectin altered chemotherapy-induced apoptosis in leukemic cells, JM-1 (VLA-4+, VLA-5 −) or RS4 (VLA-4+, VLA-5+) cells were incubated on fibronectin-coated 24-well plates (Sigma) for up to 72 hours in the presence of 0.1 to 1.0 μg/mL Ara-C, 1 to 5 μmol/L VP-16, or medium alone. Matched samples were cultured in uncoated 24-well plates. Cells were collected by vigorous pipetting, and all samples were evaluated in triplicate by trypan blue exclusion.
Blocking VCAM-1 on bone marrow stromal cells
To determine whether the observed protective effect of stromal cells resulted from VCAM-1 binding, JM-1 or RS4 cells were incubated on confluent stromal cells treated with mouse antihuman VCAM-1 antibody (Santa Cruz Biotechnology, Santa Cruz, CA) during Ara-C and VP-16 treatment. Before the addition of leukemic cells and drugs, stromal cell layers were pretreated with 5 μg of a blocking anti–VCAM-1 monoclonal antibody for 30 minutes at room temperature. At 24-hour intervals, 2.5 μg/mL fresh antibody was added to cocultures. Viability of leukemic cells cultured on anti–VCAM-1–treated stromal cells was compared to leukemic cells on control stromal cells and to stromal cells treated with an identical concentration of isotype-matched control antibody. In addition, JM-1 and RS4 cell viability in medium, in the presence and absence of drug, was evaluated. At the termination of culture, leukemic cells were collected, and viability was evaluated in triplicate by trypan blue exclusion.
Results
Bone marrow stromal cells impact JM-1 cell cycle kinetics during chemotherapy exposure
As a representative B-lineage leukemic cell line, JM-1 cell cycle status was evaluated after treatment with VP-16 or Ara-C. Data shown represent cell cycle profiles of JM-1 cells after 24 hours of exposure to each chemotherapeutic agent (Table 1). After treatment with Ara-C or VP-16, JM-1 cells accumulated in G1 of the cell cycle. The presence of stromal cells (SC) in culture abrogated this G1 block. JM-1 cells treated with Ara-C in medium alone (NS) had 73% of cells in Go/G1, compared with 42% in Go/G1 when treated in the presence of stromal cells. JM-1 cells treated with VP-16 for 24 hours had 83% in Go/G1 compared to 58% in Go/G1 when treated in the presence of stromal cells. Consistent with this observation, stromal cell coculture maintained a higher proportion of JM-1 cells in S phase during treatment than cells exposed to chemotherapy in medium alone (Table 1). Untreated cultures had fewer cells in Go/G1when stromal cells were present than in cultures that did not contain stromal cells. Higher numbers of JM-1 cells in the S and G2/M phases of the cell cycle were also recorded when JM-1 cells were cultured with stromal cells than in control cultures that did not contain stromal cells. Absolute numbers of JM-1 cells were enumerated in all cultures. Stromal cell coculture modestly increased the absolute number of JM-1 cells recovered after treatment (Table1). In addition, after chemotherapy, JM-1 cells cocultured with stromal cells were collected and moved to new adherent layers, which confirmed their ability to repopulate cultures (data not shown).
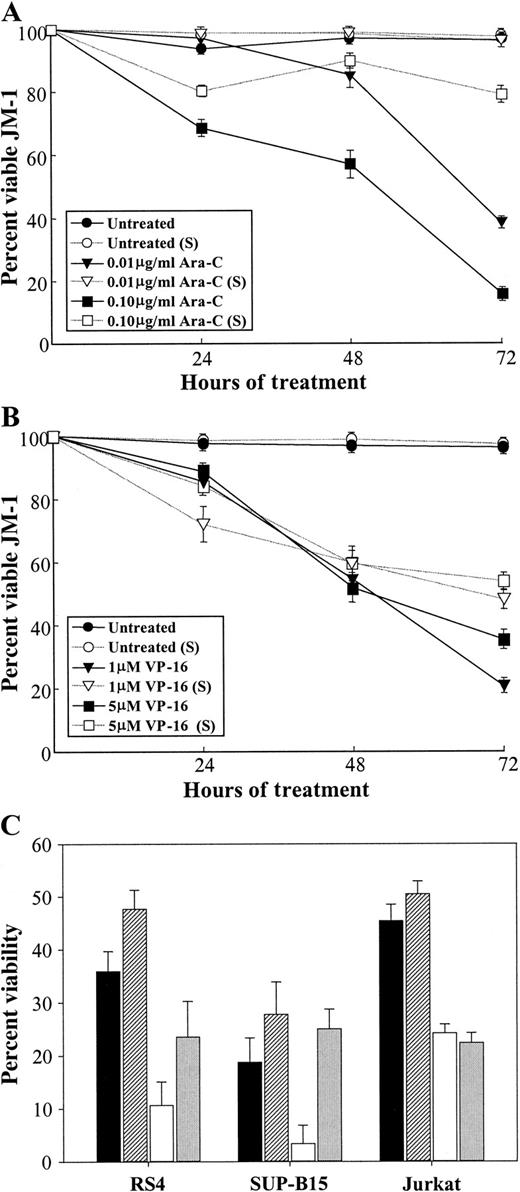
Coculture of B-lineage leukemic cells with bone marrow stromal cells decreases the effectiveness of VP-16 and Ara-C
To determine whether coculture with a stromal cell underlayer affected leukemic cell survival during chemotherapy exposure, 3 B-lineage leukemic cells lines and T-lineage Jurkat cells were grown on stromal cells and compared to cells maintained in medium alone. In all cases, stromal cell coculture resulted in increased JM-1, RS4, and SUP-B15 cell viability during treatment (Figure1). After 72 hours of treatment with 0.1 μg/mL Ara-C, JM-1 cell viability was reduced to 16% in medium alone compared to 79% when cocultured with bone marrow stromal cells (Figure1A). JM-1 cells treated with 5 μmol/L VP-16 in medium were 35.3% viable, compared to 53.8% when treated with stromal cells (Figure 1B). Untreated leukemic cells cultured on stromal cells remained approximately 100% viable and were not different from controls maintained in medium alone. Protection by stromal cell coculture was also observed when RS4 or SUP-B15 cultures were evaluated at 48 hours (Figure 1C). Stromal cell coculture consistently resulted in higher viability of B-lineage leukemic cells after treatment. RS4 cells treated with VP-16 in medium were 10.7% viable, compared to 23.6% when treated in the presence of stromal cells. VP-16 treatment of SUP-B15 cells reduced viability to 3.4% in medium alone, compared to 25.1% when treated during stromal cell coculture (Figure 1C). Comparable trends were noted at 24 and 72 hours (data not shown). Stromal cell protection was also observed during Ara-C treatment (Figure 1C). In contrast, Jurkat cell viability after treatment with Ara-C or VP-16 was not improved by stromal cells (Figure 1C). Similar viability data were recorded when leukemic cells were removed by vigorous pipetting or trypsinization.
B-lineage leukemic cell viability is enhanced during Ara-C or VP-16 treatment by bone marrow stromal cells.
(A) JM-1 cells were cultured in medium alone or with an adherent layer of bone marrow stromal cells for 24 to 72 hours in the presence or absence of Ara-C or (B) VP-16 at indicated concentrations. Leukemic cells were removed by vigorous pipetting, and viability was evaluated by trypan blue exclusion in triplicate samples. Data shown are representative of 4 independent experiments. (C) RS4, SUP B-15, or Jurkat cells were cultured for 48 hours in medium containing 0.1 μg/mL Ara-C (solid black bars) or 1 μmol/L VP-16 (open bars). Leukemic cells were treated with the same concentration of Ara-C (hatched bars) or VP-16 (light gray bars) during coculture with an adherent layer of bone marrow stromal. Leukemic cells were removed by vigorous pipetting, and viability was evaluated as above. Data shown are mean ± SEM and are representative of 2 independent experiments.
B-lineage leukemic cell viability is enhanced during Ara-C or VP-16 treatment by bone marrow stromal cells.
(A) JM-1 cells were cultured in medium alone or with an adherent layer of bone marrow stromal cells for 24 to 72 hours in the presence or absence of Ara-C or (B) VP-16 at indicated concentrations. Leukemic cells were removed by vigorous pipetting, and viability was evaluated by trypan blue exclusion in triplicate samples. Data shown are representative of 4 independent experiments. (C) RS4, SUP B-15, or Jurkat cells were cultured for 48 hours in medium containing 0.1 μg/mL Ara-C (solid black bars) or 1 μmol/L VP-16 (open bars). Leukemic cells were treated with the same concentration of Ara-C (hatched bars) or VP-16 (light gray bars) during coculture with an adherent layer of bone marrow stromal. Leukemic cells were removed by vigorous pipetting, and viability was evaluated as above. Data shown are mean ± SEM and are representative of 2 independent experiments.
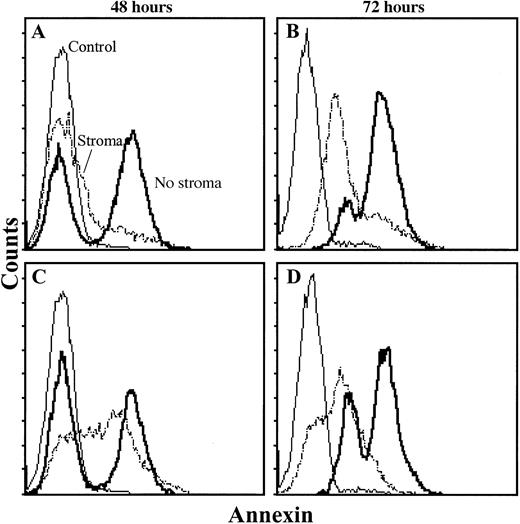
Apoptosis is reduced in leukemic cells treated with chemotherapy in the presence of an adherent stromal cell layer
To determine whether VP-16 and Ara-C induced apoptotic cell death, JM-1 cells were evaluated by annexin staining after chemotherapy exposure in the presence or absence of bone marrow stromal cells. The presence of stromal cells resulted in reduced numbers of apoptotic JM-1 cells in cultures treated with VP-16 or Ara-C (Figure2).
Chemotherapy-induced apoptosis of JM-1 cells is delayed by coculture with stromal cells.
After 48 and 72 hours of culture in 0.1 μg/mL Ara-C (A, B) or 5 μmol/L VP-16 (C, D), JM-1 cells were collected as described and stained with Annexin-V–FITC. Samples included untreated JM-1 control cells (control), JM-1 cells treated on an adherent stromal cell layer (stroma), and JM-1 cells treated in medium alone (no stroma). JM-1 cells were collected on a Becton Dickinson Flow Cytometer, and data were analyzed using CellQuest software.
Chemotherapy-induced apoptosis of JM-1 cells is delayed by coculture with stromal cells.
After 48 and 72 hours of culture in 0.1 μg/mL Ara-C (A, B) or 5 μmol/L VP-16 (C, D), JM-1 cells were collected as described and stained with Annexin-V–FITC. Samples included untreated JM-1 control cells (control), JM-1 cells treated on an adherent stromal cell layer (stroma), and JM-1 cells treated in medium alone (no stroma). JM-1 cells were collected on a Becton Dickinson Flow Cytometer, and data were analyzed using CellQuest software.
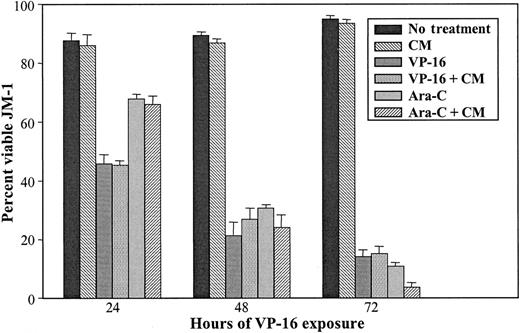
Soluble stromal cell-derived factors do not enhance leukemic cell survival during VP-16 or Ara-C treatment
To determine whether soluble factors derived from stromal cells altered the response of leukemic cells to chemotherapy, JM-1 cells were cultured in stromal cell-conditioned medium in the presence or absence of VP-16 or Ara-C as described, and viability evaluated. No significant differences in JM-1 viability were observed during Ara-C or VP-16 treatment in conditioned medium compared to control fresh medium (Figure 3).
Stromal cell-conditioned medium does not significantly alter the response of JM-1 cells to Ara-C or VP-16.
JM-1 cells were cultured in 75% stromal cell conditioned medium for 24 to 72 hours in the presence or absence of VP-16 or Ara-C, as described in “Materials and methods.” Viability was evaluated by trypan blue exclusion in triplicate samples. Data shown are mean ± SEM and are representative of 3 independent experiments.
Stromal cell-conditioned medium does not significantly alter the response of JM-1 cells to Ara-C or VP-16.
JM-1 cells were cultured in 75% stromal cell conditioned medium for 24 to 72 hours in the presence or absence of VP-16 or Ara-C, as described in “Materials and methods.” Viability was evaluated by trypan blue exclusion in triplicate samples. Data shown are mean ± SEM and are representative of 3 independent experiments.
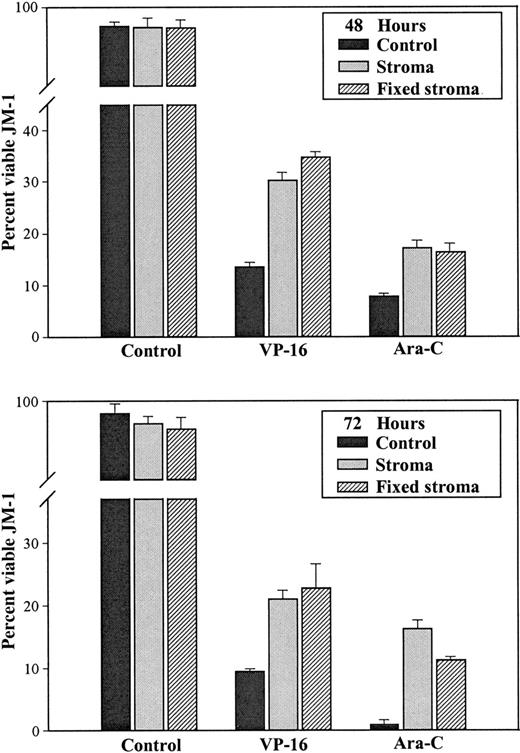
Interaction with stromal cell surface proteins altered the response of JM-1 cells to Ara-C and VP-16
Stromal cells were fixed in 2% glutaraldehyde and used in coculture experiments as described above. Viability of JM-1 cells treated on control or fixed stroma was significantly higher than medium alone in all groups (Tukey test; P = < .001). Coculture with untreated stromal cells increased the viability of JM-1 cells exposed to VP-16 from 16% to 30% after 48 hours and from 9% to 24% after 72 hours. Glutaraldehyde-fixed stromal cells increased the viability of VP-16–treated JM-1 cells to 34% and 26% at 48 and 72 hours, respectively. JM-1 viability during treatment with Ara-C was increased comparably by coculture with control or fixed stromal cells (Figure 4). Adherence of JM-1 cells to stromal cells was not affected by fixation (data not shown).
Glutaraldehyde fixation of bone marrow stromal cells does not alter chemotherapy protection.
Confluent stromal cells were treated with 2% glutaraldehyde for 5 minutes and were thoroughly rinsed before the addition of JM-1 cells. Matched control stromal cells were cultured in medium alone. JM-1 cells cultured on control or glutaraldehyde-treated stromal cells were exposed to 5 μmol/L VP-16 or 1.0 μg/mL Ara-C. Chemotherapy-treated JM-1 cells were also evaluated in medium alone. After 48 and 72 hours of culture, JM-1 cells were collected, and viability of triplicate samples were evaluated by trypan blue exclusion.
Glutaraldehyde fixation of bone marrow stromal cells does not alter chemotherapy protection.
Confluent stromal cells were treated with 2% glutaraldehyde for 5 minutes and were thoroughly rinsed before the addition of JM-1 cells. Matched control stromal cells were cultured in medium alone. JM-1 cells cultured on control or glutaraldehyde-treated stromal cells were exposed to 5 μmol/L VP-16 or 1.0 μg/mL Ara-C. Chemotherapy-treated JM-1 cells were also evaluated in medium alone. After 48 and 72 hours of culture, JM-1 cells were collected, and viability of triplicate samples were evaluated by trypan blue exclusion.
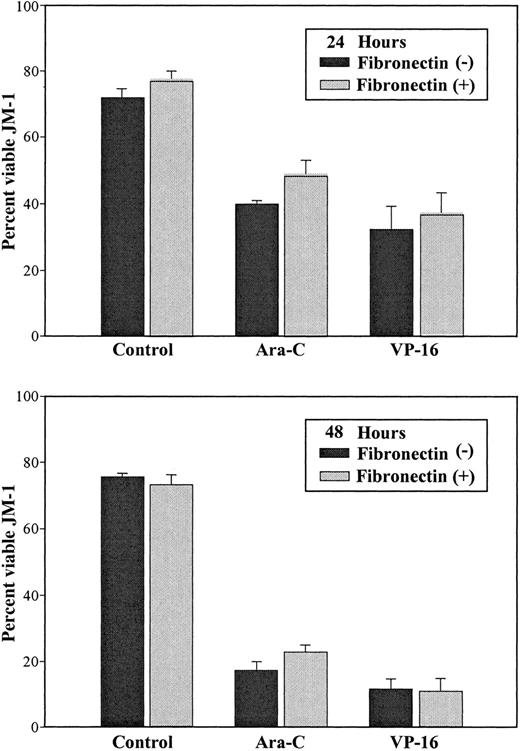
Interaction with fibronectin did not enhance survival of JM-1 or RS4 cells during chemotherapy exposure
To determine whether interaction with the stromal cell adhesion molecule fibronectin conferred part of the protection against chemotherapy-induced apoptosis in JM-1 or RS4 cells, leukemic cells were incubated on fibronectin-coated plates in the presence of Ara-C, VP-16, or medium alone as previously described. Incubation of JM-1 cells on fibronectin-coated plates during 24 hours or 48 hours of Ara-C and VP-16 exposure did not protect JM-1 cells from chemotherapy-induced cell death (Figure 5).
Adhesion to fibronectin does not protect JM-1 cells from Ara-C– or VP-16–induced cell death.
JM-1 cells were incubated in 24-well plates for 24 or 48 hours in the presence of 1.0 μg/mL Ara-C, 5 μmol/L VP-16, or medium alone (control). Culture plates used were coated with fibronectin (black bars) or uncoated (gray bars). JM-1 cells were collected by vigorous pipetting and evaluated in triplicate by trypan blue exclusion. A representative graph of 3 independent experiments is presented. Data shown are mean ± SEM.
Adhesion to fibronectin does not protect JM-1 cells from Ara-C– or VP-16–induced cell death.
JM-1 cells were incubated in 24-well plates for 24 or 48 hours in the presence of 1.0 μg/mL Ara-C, 5 μmol/L VP-16, or medium alone (control). Culture plates used were coated with fibronectin (black bars) or uncoated (gray bars). JM-1 cells were collected by vigorous pipetting and evaluated in triplicate by trypan blue exclusion. A representative graph of 3 independent experiments is presented. Data shown are mean ± SEM.
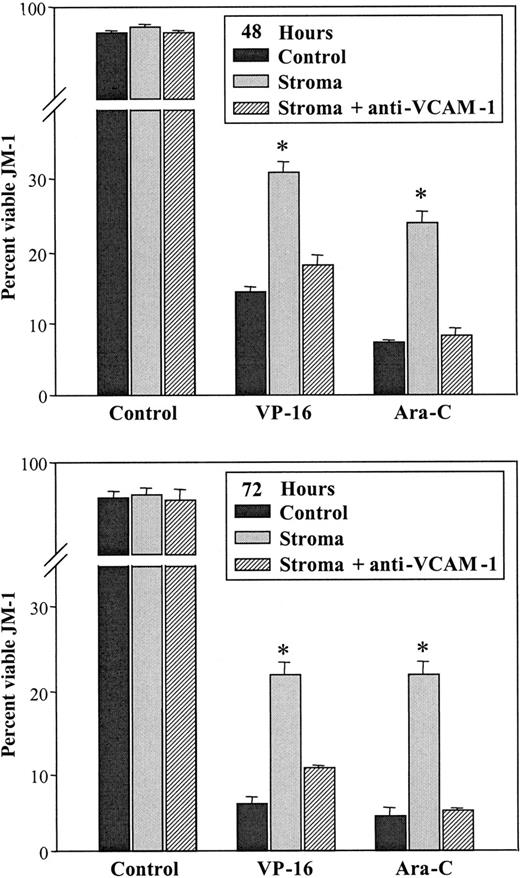
Signaling through adhesion of JM-1 or RS4 cells to VCAM-1 was required for maximal protection from Ara-C– and VP-16–induced cell death
To evaluate the contribution of VCAM-1 in adhesion in protection from chemotherapy, binding was interrupted using a blocking anti–VCAM-1 antibody. After culture in 0.1 μg/mL Ara-C or 5 μmol/L VP-16 as previously described, viability of JM-1 or RS4 cells was significantly lower in cultures containing stromal cells treated with anti–VCAM-1 antibody than in untreated stromal cells (Figure6). After 48 hours of treatment with Ara-C, JM-1 cells in medium alone had viability reduced to approximately 8% from a control value of 96%. The presence of stromal cells increased Ara-C– or VP-16–treated JM-1 viability to approximately 23%. Treatment of stromal cells with anti–VCAM-1 antibody abrogated the protective effect of stromal cell coculture. Treatment of stromal cell layers with a matched isotype control antibody did not diminish the protective capacity of stromal cells in any sample (data not shown).
Disruption of VCAM-1 binding abrogates stromal cell protection of JM-1 cells during chemotherapy.
JM-1 cells were incubated on confluent stromal cells treated with mouse antihuman VCAM-1 antibody during Ara-C and VP-16 treatment. Before the addition of leukemic cells and chemotherapeutic drugs, stromal cell layers were pretreated with 5 μg anti–VCAM-1; 2.5 μg/mL fresh antibody was added at 24-hour intervals, as described in “Materials and methods.” Viability of leukemic cells cultured on anti–VCAM-1–treated stromal cells was compared to that of JM-1 cells on control stromal cells and to that of stromal cells treated with an isotype-matched control antibody. In addition, JM-1 cells in medium, in the presence and absence of drug, were included. After 48 to 72 hours of culture, JM-1 cells were collected and evaluated in triplicate by trypan blue exclusion. Data shown are mean ± SEM and are representative of 3 independent experiments.
Disruption of VCAM-1 binding abrogates stromal cell protection of JM-1 cells during chemotherapy.
JM-1 cells were incubated on confluent stromal cells treated with mouse antihuman VCAM-1 antibody during Ara-C and VP-16 treatment. Before the addition of leukemic cells and chemotherapeutic drugs, stromal cell layers were pretreated with 5 μg anti–VCAM-1; 2.5 μg/mL fresh antibody was added at 24-hour intervals, as described in “Materials and methods.” Viability of leukemic cells cultured on anti–VCAM-1–treated stromal cells was compared to that of JM-1 cells on control stromal cells and to that of stromal cells treated with an isotype-matched control antibody. In addition, JM-1 cells in medium, in the presence and absence of drug, were included. After 48 to 72 hours of culture, JM-1 cells were collected and evaluated in triplicate by trypan blue exclusion. Data shown are mean ± SEM and are representative of 3 independent experiments.
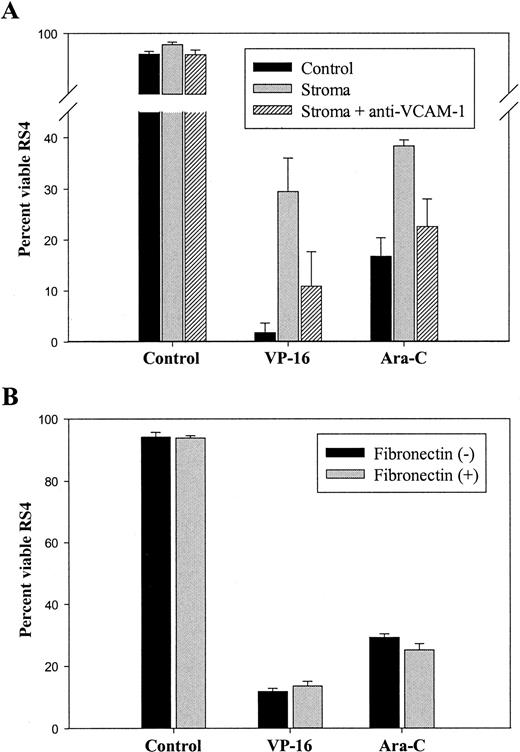
Similarly, incubation of RS4 cells with anti–VCAM-1–treated bone marrow stromal cells diminished the protective capacity of stromal cells during Ara-C and VP-16 treatment (Figure7B). After 72 hours of treatment in medium alone, RS4 viability was reduced to 17% in Ara-C and 2% in VP-16 treated cultures. Stromal cell coculture during treatment increased the viability of RS4 cells exposed to either chemotherapeutic drug. Consistent with JM-1 cells, incubation of stromal cells with anti–VCAM-1 antibody reduced the viability of RS4 on stromal cells from 38% to 23% in cultures containing Ara-C and from 30% to 11% in cultures exposed to VP-16 (Figure 7B). JM-1 and RS4 cells were shown to lack VCAM-1 expression by flow cytometric analysis (data not shown).
Fibronectin does not protect VLA-4+VLA-5+ RS4 cells from Ara-C or VP-16–induced cell death.
(A) RS4 cells were incubated in 24-well plates for 72 hours in the presence of 0.1 μg/mL Ara-C, 5 μmol/L VP-16, or medium alone (control). Culture plates used were coated with fibronectin (black bars) or uncoated (gray bars). RS-4 cells were collected by vigorous pipetting and were evaluated in triplicate by trypan blue exclusion. (B) RS-4 cells were incubated on confluent stromal cells treated with mouse antihuman VCAM-1 antibody during Ara-C and VP-16 treatment. Before the addition of leukemic cells and chemotherapeutic drugs, stromal cell layers were pretreated with 5 μg anti–VCAM-1; 2.5 μg/mL fresh antibody was added at 24-hour intervals, as described in “Materials and methods.” Viability of leukemic cells cultured on anti–VCAM-1–treated stromal cells was compared to RS-4 cells on control stromal cells. Data shown are mean ± SEM and are representative of 2 independent experiments.
Fibronectin does not protect VLA-4+VLA-5+ RS4 cells from Ara-C or VP-16–induced cell death.
(A) RS4 cells were incubated in 24-well plates for 72 hours in the presence of 0.1 μg/mL Ara-C, 5 μmol/L VP-16, or medium alone (control). Culture plates used were coated with fibronectin (black bars) or uncoated (gray bars). RS-4 cells were collected by vigorous pipetting and were evaluated in triplicate by trypan blue exclusion. (B) RS-4 cells were incubated on confluent stromal cells treated with mouse antihuman VCAM-1 antibody during Ara-C and VP-16 treatment. Before the addition of leukemic cells and chemotherapeutic drugs, stromal cell layers were pretreated with 5 μg anti–VCAM-1; 2.5 μg/mL fresh antibody was added at 24-hour intervals, as described in “Materials and methods.” Viability of leukemic cells cultured on anti–VCAM-1–treated stromal cells was compared to RS-4 cells on control stromal cells. Data shown are mean ± SEM and are representative of 2 independent experiments.
Discussion
Recognition that microenvironmental cues impact tumor cell response to treatment is not unique to leukemic cells. Previous studies have investigated the responses of various tumor cell types to chemotherapy and reported an association of responses with metastatic site. In one report, the response of colon carcinoma to doxorubicin and 5-flurouracil was correlated with 3 distinct anatomic sites: lung, liver, and spleen.13 In vivo sites that conferred maximal doxorubicin resistance had elevated levels of protein kinase-C activity in the carcinoma cells tested.14 These observations suggest that signaling pathways may be impacted by factors that are unique to specific sites in the microenvironment. In the current report, we describe the effect of bone marrow stromal cells on survival of 3 B-lineage leukemic cell lines. The presence of an intact stromal cell layer conferred dramatic protection from chemotherapy-induced apoptotic cell death. This protective effect of stromal cells could be attributed to the expression of VCAM-1 on the stromal cell surface. This observation has significant implications for the design of new chemotherapeutic regimens to treat this disease.
VLA-4 expression on leukemic cells of lymphoid and myeloid origin has been shown to facilitate adhesion to bone marrow stromal cells through binding to VCAM-1 in vitro.4,15,16 Pre-incubation of an adherent cell layer with anti–VCAM-1 antibody significantly blocked the adhesion of pre-B ALL cells derived from 19 patients.17 This report was consistent with observations of normal immature B-cell precursors that were shown to have reduced adhesion to marrow-derived fibroblasts when treated with antibodies to the α and β chains of VLA-4.18 Functional relevance of these observations was suggested by an in vivo model in which a variant pre-B ALL cell line, which lacked VLA-4 expression, had reduced ability to establish leukemia in sublethally irradiated SCID mice.19 In this study, mice with established leukemia had significantly less marrow infiltration with the VLA-4−variant of NALM-6.19 Consistent with in vivo data from this study, VLA-4− cells had reduced binding to, and migration beneath, an adherent murine stromal cell layer.19 These reports emphasize the role of VLA-4 interactions with VCAM-1 in mediating the adhesion of leukemic cells to stromal cells in the marrow and support the usefulness of in vitro coculture models in which stromal and leukemic cell interactions can be studied.
The importance of understanding interactions between leukemic progenitor cells and the bone marrow microenvironment is based not only on the marrow being the site in which disease is initiated, but also on the finding that bone marrow is the site of first relapse for approximately 60% to 70% of childhood ALL.1,2 If the initial relapse is at an extramedullary site, such as the central nervous system, marrow disease has often developed and is detectable by PCR.1 In a study of 13 children with ALL relapse outside the bone marrow, disease was detected in marrow samples of 12 children.1 In vivo models have suggested a negative correlation between the number of residual leukemic cells in the marrow and disease-free survival,20 making interactions between leukemic cells and bone marrow stromal cells important to investigate.
In the current study it was noted that the cell cycle progression of JM-1 cells is maintained when stromal cells are present in cultures during chemotherapy exposure, in contrast to disrupted cycling of leukemic cells exposed to chemotherapy in the absence of stromal cells (Table 1). Modestly increased numbers of JM-1 cells were recovered from cultures after treatment during coculture (Table 1). Regulation of the expression or activity of proteins that control cell cycle progression is one way stromal cells may influence malignant cells associated with it in vivo. Signals that alter intracellular phosphorylation are a potentially rapid and effective method by which stromal cells modulate production or activity of leukemic cell proteins. A recent report suggested Rb phosphorylation as one factor impacted by stromal cell coculture of a leukemic cell line BLIN-2.21Hyperphosphorylation of Rb subsequent to exposure to stromal cells may contribute to dysregulated cell cycle progression and may be one mechanism by which stromal cells augment leukemic cell proliferation.
In addition to maintaining proliferation during treatment, stromal cell coculture delayed the onset of apoptosis in JM-1 and enhanced viability of JM-1, RS4, and SUP-B15 cells (Figures 1 and 2). We previously described the regulation of bcl-2 and bax in normal murine pro-B cells by contact with bone marrow stromal cells.22 Based on similarities between B-lineage ALL cells and normal B-cell progenitors, it is likely that the stromal cell microenvironment may impact expression of these apoptotic regulatory molecules in leukemic cells as well. Interestingly, elevated bcl-2 expression has been shown to block chemotherapy-induced apoptosis of the human pre-B leukemic cell line, 697, in response to a wide variety of agents, including etoposide (VP-16) and 1-β-D-arabinofuranosyl-cytosine (Ara-C).23,24 Chronic lymphocytic leukemia cells (CLL) have also been shown to have glucocorticoid and chemotherapy sensitivity affected by the endogenous ratio of BCL-2:BAX.25 A recent report indicated that the human B-lymphoma cells line, JLP119, altered BAX conformational changes during etoposide treatment if stimulated with VCAM-1 or IL-4, mediators that can be found in the bone marrow microenvironment.26These observations emphasize stromal cell influence of apoptotic regulatory molecules as a likely mechanism by which the microenvironment modulates response to chemotherapy.
In the current study, stromal cell-conditioned medium conferred negligible protection to leukemic cells during VP-16 and Ara-C exposure (Figure 3). Therefore, the role of proteins on the stromal cell surface was investigated with glutaraldehyde-fixed stromal cells (Figure 4). Previous reports have shown this fixation process to disrupt adequately the metabolism of adherent 3T3 cells, allowing investigation of the role of signaling through ligand–receptor interactions in the absence of cytokine production.11 It has been reported that signaling between stromal cells and hematopoietic progenitors can be bidirectional, with the adhesion of hematopoietic cells to stromal cells altering stromal cell function.27 This presented the possibility that the adhesion of JM-1 cells to stromal cells resulted in alterations of stromal cell function that were protective during chemotherapy. However, in our study, adhesion to fixed stromal cells resulted in viability of chemotherapy-treated JM-1 cells that was not different from viable stromal cells (Figure 4). In addition, we investigated the possibility that stromal cell adherent layers may sequester chemotherapeutic agents, with diminished leukemic cell death during coculture resulting from reduced drug concentrations in the culture medium. However, comparisons of Ara-C and VP-16 activity in medium cocultured on stromal cells layers versus medium alone indicated no significant change in effectiveness of drug (data not shown). JM-1 cells were killed as efficiently by Ara-C or VP-16 pre-incubated for 48 hours on a confluent stromal cell layer as they were by the same concentration of drug incubated for 48 hours in medium alone (data not shown). These observations support the conclusion that signals that protect leukemic cell survival primarily result from cell surface interactions.
It is interesting that the interaction of JM-1 cells with surface VCAM-1 was protective during Ara-C and VP-16 exposure (Figures 6 and7B) but that fibronectin was not (Figures 5, 7A). Both VCAM-1 and fibronectin bind to VLA-4 on JM-1 cells; however, these ligands bind VLA-4 at different sites on the molecule.28 These data suggest that VCAM-1 binding results in distinctly different intracellular signals in JM-1 cells than results from fibronectin binding. Alternatively, the activation state of VLA-4 might not have been such that optimal binding to, or signaling through, VLA-4 occurred. To determine whether the presence of VLA-5, in addition to VLA-4, on the leukemic cell surface supported protection through interaction with fibronectin, the response of RS4 cells expressing both receptors was investigated. Again, interaction with fibronectin did not significantly protect from Ara-C– or VP-16–induced cell death (Figure7A). This observation further supports the importance of signaling that occurs downstream of interaction with VCAM-1. Interestingly, Jurkat cells that express both VLA-4 and VLA-5 did not benefit from interaction with stromal cells during Ara-C or VP-16 exposure (Figure1C). This suggests the presence of intracellular pathways that are unique to B-lineage leukemic cells and that can be regulated by interaction with the bone marrow microenvironment. However, significant components appear common to B-lineage ALL cells because JM-1, RS4, and SUP-B15 were uniformly protected from chemotherapy-induced cell death by stromal cell coculture, in spite of phenotypic differences (Figure1).
The role of stromal cells in protecting tumor cells from chemotherapy has clinical and biologic implications. In addition to leukemic cells, epithelial tumors, including breast29 and prostate30 cancer, have been shown to metastasize to the bone marrow. As do leukemic cells, residual tumor cells in these diseases that escape treatment contribute to relapse. For that reason, it will be essential to evaluate the effect of stromal cells on chemotherapeutic regimens used for various tumors. Understanding the role of stromal cells in the maintenance of minimal residual disease in hematopoietic and epithelial tumors is essential for the design of improved therapies to eradicate affected cells. This is particularly important because of the aggressive phenotype of tumor cells at relapse,31 which contributes to disease that is often refractory to standard treatment and ultimately to poor clinical outcome.
Acknowledgments
The authors thank Drs Kenneth S. Landreth and Solveig G. Ericson for critically reviewing this manuscript.
Supported in part by the Elsa U. Pardee Foundation (L.F.G.), and a West Virginia University Research Development Grant (L.F.G.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Laura F. Gibson, Department of Pediatrics, Health Sciences Center, West Virginia University, P. O. Box 9214, Morgantown, WV 26506; e-mail: lgibson@hsc.wvu.edu.