Abstract
To investigate the clinical applicability of prophylaxis of post-transplant graft-versus-host disease by UV-B irradiation of stem cell preparations, the UV-B sensitivities of human lymphocytes and primitive hematopoietic progenitors were compared. The mononuclear cell fractions (MNC) derived from human cord blood and granulocyte–colony-stimulating factor–mobilized peripheral blood were used. After UV-B irradiation, lymphocyte proliferation ability, hematopoietic colony-forming cells, and apoptotic cells were analyzed. At a dose of 33 J/m2, significant differences were observed in the residual percentages of hematopoietic progenitors and lymphocyte functions [ANOVA, F (5,46) = 19.4; P < .0001], and the difference between CFU-C (85.2% + 24.0%; n = 8) and MLR (12.7% + 12.6%; n = 10) was significant (P < .0001). There were no significant differences in the residual percentages of CFU-C, HPP-CFC, and LTC-IC. Percentages of annexin V-positive cells in the total MNC and the CD34+cell population in MNC after UV-B irradiation were 69.8% and 18.7%, respectively. In conclusion, there was a range of UV-B doses over which T lymphocytes were inactivated but hematopoietic progenitors, including HPP-CFC and LTC-IC, were preserved.
Introduction
Ultraviolet B irradiation of donor inoculum is known to suppress lymphocyte proliferation and has been shown to prevent graft-versus-host disease (GVHD) and host-versus-graft rejection in a number of animal models.1-6 Because of the problems of T-cell depletion and selective CD34+ cell transplantation, this method has attracted attention for use in human allogeneic hematopoietic stem cell transplantation. One of the most important considerations is to what extent the hematopoietic stem cells are damaged by the UV-B dose used to inactivate T cells in the graft.7 In murine and rat models, lymphocytes have been shown to be more sensitive than hematopoietic stem cells.8,9 Human lymphocytes were reported to be more sensitive to UV-B than hematopoietic progenitors.10However, hematopoietic progenitors do not necessarily represent the cells responsible for long-term engraftment. Recently, cord blood transplantation and allogeneic peripheral blood stem cell transplantation have been conducted as alternatives to bone marrow transplantation. Unfortunately, the occurrence of GVHD remains a major problem. Therefore, we investigated the UV-B sensitivity of primitive hematopoietic progenitors, such as highly proliferative potential colony-forming cells (HPP-CFC) and long-term culture-initiating cells (LTC-IC), in cord blood and peripheral blood stem cells.
Materials and methods
Cell preparation
Cord blood and G-CSF–mobilized peripheral blood stem cells (PBSC) were used in this study. Cord blood was used within 24 hours of delivery, and PBSC were used just after cytapheresis. Informed consent was obtained from all donors. Mononuclear cells separated by Ficoll-Hypaque density gradient centrifugation were suspended in plain RPMI 1640 at a concentration of 1 × 106/mL. This fraction was designated as mononuclear cell fractions (MNC). At first 12 samples (cord, 5; PBSC, 7) were obtained to evaluate the UV-B sensitivity of lymphocytes and hematopoietic progenitors. An additional 10 samples (cord, 5; PBSC, 5) were obtained to evaluate the UV-B sensitivity of more primitive human hematopoietic progenitors.
UV-B irradiation
Aliquots of 2 mL MNC suspension were transferred to 60-mm plastic dishes and put on a shaker at 60 rpm. Samples were irradiated with a UV-B lamp (FL15E, UV-320; range, 300-320 nm; peak, 315 nm; UVP, San Gabriel, CA) at a dose of 0, 33, 66, 100, or 200 J/m2. Irradiation dose was adjusted by duration of irradiation.
Hematopoietic progenitor assay
Committed hematopoietic progenitors were assessed according to the method described by Sato et al.11 The total colony number was expressed as CFU-C. Colonies larger than 2 mm in diameter were counted as HPP-CFC.
Long-term culture-initiating cell assay
LTC-IC assay was performed according to the method described by Issaad et al.12
Evaluation of lymphocyte responsiveness to concanavalin A and allogeneic stimulator
Aliquots of 180 μL cell suspension, 20 μL fetal calf serum, and conA (Sigma, St Louis, MO) solution (final concentration, 10 μg/mL) were mixed in 96-well microplates and incubated for 72 hours. For one-way mixed-lymphocyte reaction (MLR), 80 μL of both responder cell suspension (1 × 106/mL) and gamma-irradiated (30 Gy) allogeneic stimulator cell suspension (1 × 106/mL) and 40 μL of heat-inactivated human AB serum were mixed in 96-well microplates and incubated for 5 days. Each culture was pulse-labeled with 3H-thymidine (37 Bq) and further incubated for 18 hours. Then the cells were harvested, and 3H-thymidine in DNA was measured.
Evaluation of apoptotic cells
After UV-B irradiation, cells were incubated for 24 hours. Apoptotic cells were detected by flow cytometry using an apoptosis detection kit (Pharmingen, San Diego, CA), and a combination of fluorescein isothiocyanate-conjugated annexin V solution (Annexin-V-Fluos; Boehringer Mannheim, Mannheim, Germany) and propidium iodide solution (50 μg/mL in phosphate-buffered saline) (Sigma, St Louis, MO).
Evaluation of sensitivity of CD34+ cells and lymphocytes to UV-B in terms of apoptotic change
MNC were stained with phycoerythrin-conjugated anti-CD2, -CD4, -CD8, -CD19, -CD56, or -CD34 monoclonal antibodies (Pharmingen, San Diego, CA) for lymphocyte subsets, and cell surface binding of the annexin V of each subset was evaluated 24 hours after UV-B irradiation.
Statistical analysis
Statistical analyses were performed using ANOVA and the Scheffe post hoc test with StatView 4.02.
Results and discussion
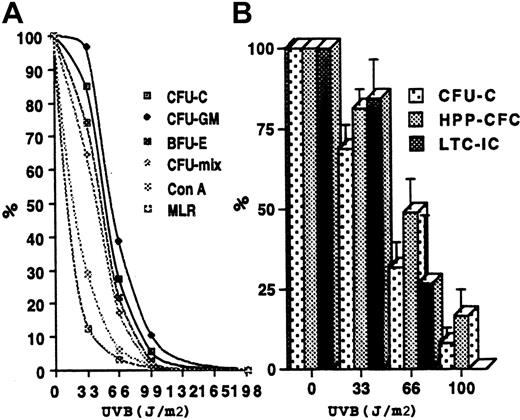
Residual percentages of conA response and MLR at a dose of 33 J/m2 were 29.2% ± 18.0% (n = 11) and 12.7% ± 12.6% (n = 10), respectively. In contrast, those of CFU-C, CFU-GM, CFU-E, and CFU-mix were 85.2% ± 24.0% (n = 8), 96.9% ± 17.8% (n = 8), 74.2% ± 30.1% (n = 8), and 64.5% ± 32.6% (n = 7), respectively (Figure1A). There was a significant difference in residual percentage between colony formation and proliferative responses [ANOVA, F (5,46) = 19.4;P < .0001]. Residual percentages of colony formation were all significantly higher than that of conA (P ≤ .0075) and MLR (P < .005), except conA response versus CFU-mix (P = .086). Thus, at a dose of 33 J/m2, the hematopoietic progenitors assayed under conventional culture conditions were better preserved than lymphocytes. This range was almost the same as that reported by Deeg et al,10 though they used human bone marrow as a source of hematopoietic progenitors.
Effect of UV-B on lymphocytes and hematopoietic progenitors.
(A) Dose-dependent reduction of lymphocyte proliferation and hematopoietic progenitors. The differences between the residual percentage of colony formation and lymphocyte proliferation at 33J/m2 were significant (see text). At 66 J/m2, only the difference between lymphocyte proliferation response and CFU-GM was significant (P < .005). (B) Preservation of more primitive hematopoietic progenitors after UV-B irradiation. MNC were separated from cord blood (n = 5) and PBSC (n = 5) and irradiated with various doses of UV-B. Residual percentages of CFU-C, HPP-CFC, and LTC-IC at doses of 33 J/m2 were 69% ± 25.1%, 81.4% ± 17.9%, and 84.5% ± 4.3%, respectively. These differences were not significant. Results are all expressed as means ± SD. Error bars in the graph represent SE.
Effect of UV-B on lymphocytes and hematopoietic progenitors.
(A) Dose-dependent reduction of lymphocyte proliferation and hematopoietic progenitors. The differences between the residual percentage of colony formation and lymphocyte proliferation at 33J/m2 were significant (see text). At 66 J/m2, only the difference between lymphocyte proliferation response and CFU-GM was significant (P < .005). (B) Preservation of more primitive hematopoietic progenitors after UV-B irradiation. MNC were separated from cord blood (n = 5) and PBSC (n = 5) and irradiated with various doses of UV-B. Residual percentages of CFU-C, HPP-CFC, and LTC-IC at doses of 33 J/m2 were 69% ± 25.1%, 81.4% ± 17.9%, and 84.5% ± 4.3%, respectively. These differences were not significant. Results are all expressed as means ± SD. Error bars in the graph represent SE.
We further conducted HPP-CFC and LTC-IC assays in combination with conventional hematopoietic progenitor assays. Percentages of residual CFU-C, HPP-CFC, and LTC-IC were reduced in a dose-dependent manner in the UV-B dose range from 0 to 100 J/m2 (Figure 1B). There were no significant differences in the percentages of residual activity among them at 33 J/m2 [ANOVA, F (2,20);P = .336] or 66 J/m2 [ANOVA, F (2,20); P = .378]. These results suggested that the sensitivity of primitive hematopoietic progenitors (HPP-CFC and LTC-IC) to UV-B was similar to that of hematopoietic progenitors (CFU-C). Thus, at a dose of 33 J/m2, the human primitive hematopoietic progenitors important for long-term marrow engraftment were well preserved, whereas lymphocyte proliferative ability was markedly reduced. To our knowledge, this is the first report of the sensitivity of human primitive hematopoietic progenitors to UV-B.
Many studies have been performed to elucidate the effects of UV-B on lymphocytes.13-15 Yaron et al16 reported that UV-B irradiation induced apoptosis in resting T cells. We confirmed the increases in annexin V-positive and propidium iodide-negative cells (confirmed apoptotic cells) or TUNEL-positive cell in MNC and in cells positive for lymphocyte markers after UV-B irradiation in a dose-dependent manner (data not shown). We further evaluated the sensitivities of MNC and CD34+ cells in MNC to UV-B with respect to apoptotic changes. At a dose of 33 J/m2, the percentage of annexin V-positive cells in the CD34+ population was only 18.7%, whereas that of MNC was 69.8% (Table 1). This suggested that the CD34+ cells were more resistant to UV-B than lymphocytes in terms of apoptotic changes. This was consistent with the previous result reported by Yaron et al17 and the results of colony formation and lymphocyte proliferation assay reported in this paper.
At 33 J/m2, approximately 15% of MLR activity was still observed, whereas approximately 15% inhibition of LTC-IC was seen at 33 J/m2 and 60% at 66 J/m2. Therefore, a UV-B dose range from 33 to 66 J/m2 appeared too toxic. These observations indicated the preservation of potential ability to cause both GVHD and GVL effects in the irradiated inoculum. Because the GVL effect is supposed to be important for the prevention of tumor relapse and is raised by T cells directed toward allogeneic minor peptides, the effects of UV-B on presentation of these peptides should be addressed.
In contrast, in an animal model, bone marrow irradiated with a low dose of UV-B could be grafted into cyclosporin A (CyA)-treated recipients without causing GVHD.18 CyA might prevent GVHD and GVL effects caused by the preserved lymphocytes, whereas it might not damage the hematopoietic stem cells. In this sense, UV-B irradiation with CyA treatment might be applicable in humans, especially in non-neoplastic disease.
Finally, caution is still necessary in the use of UV-B irradiation, because UV-B has the potential to cause gene mutation in preserved hematopoietic stem cells that could cause unacceptable long-term risk in patients.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Hiroshi Azuma, Hokkaido Red Cross Blood Center, Yamanote 2-2 Nishi-ku, Sapporo 063-0002, Japan; e-mail:azuma@hokkaido.bc.jrc.or.jp.