Abstract
The interleukin 9 (IL-9) pathway has recently been associated with the asthmatic phenotype including an eosinophilic tissue inflammation. The mechanism by which IL-9 affects eosinophils (eos) is not known. To investigate whether this cytokine has a direct activity on the development of eos and eosinophilic inflammation, a model of thioglycolate-induced peritoneal inflammation was used in IL-9 transgenic (TG5) and background strain (FVB) mice. In this model, a transient eosinophilic infiltration in the peritoneal cavity was observed in FVB mice 12 to 24 hours after thioglycolate injection that coincided with peak IL-5 and IL-9 release. In contrast, TG5 mice developed a massive eosinophilia that persisted at high levels (81% of total cells) even 72 hours after thioglycolate injection. Release of eosinophilic major basic protein (MBP), IL-4, and IL-5 to the peritoneal cavity of these mice was significantly increased when compared with the control FVB strain. To study the mechanism by which IL-9 exerts its effect on eos, bone marrow or peritoneal cells were cultured in the presence of IL-5, IL-9, or their combination in vitro. IL-5 alone was able to generate significant numbers of eos in TG5 but not FVB mice, whereas a combination of IL-5 and IL-9 induced marked eosinophilia in both strains indicating a synergism between these 2 cytokines. These data suggest that IL-9 may promote and sustain eosinophilic inflammation via IL-5–driven eos maturation of precursors.
Introduction
Eosinophilic granulocytes are recognized as proinflammatory cells implicated in protection against parasite infections and are believed to play an important role in the pathogenesis of asthma and allergy. The preferential accumulation of these cells in the inflamed tissue, however, remains an enigma.1 Eosinophils (eos) are nondividing, granule-containing cells that arise principally in the bone marrow from myeloid precursors.2 Maturation is known to be controlled by cytokine and growth factors including granulocyte-macrophage colony-stimulating factor, interleukin 3 (IL-3), and IL-5, the latter being specific for eos.3 4
Interleukin 9 (IL-9) is a member of the Th2 cytokine family discovered from the search for a growth-promoting activity that allowed for the antigen-independent proliferation of T-helper clones.5,6IL-9 plays a key role in mast cell differentiation by regulating the expression of mast cell proteases and the α-chain of the high affinity IgE receptor.7,8 Overexpression of IL-9 in vivo results in a massive mastocytosis in various tissues.9,10In addition, recent observations indicate that IL-9 has a role in the function of a number of other biologic targets such as B1 cells,11 immature neuronal cell lines, and hematopoietic progenitors.12 Although the genes encoding eos-activating cytokine growth factors and IL-9 are located on the long arm of chromosome 5 (5q31-q33) in close proximity,13 and the hematopoietic activities of this cytokine are apparent, so far there has been no direct indication of the involvement of IL-9 in eosinopoiesis.
In the present study we hypothesized that IL-9 has a significant function in development of selective eosinophilia in an inflammatory condition by promoting recruitment and maturation of these cells. To evaluate the contribution of IL-9 in local eosinophilia, we used a model of thioglycolate-induced peritoneal inflammation in IL-9 transgenic (TG5) and wild-type FVB/N (FVB) mice. We examined and compared the kinetics of the inflammatory events including analysis of cellular composition of bone marrow, blood and peritoneal lavage, local cytokine and chemokine production, and proliferative abilities of bone marrow precursor cells from TG5 and FVB mice. Further, we have used this model to study the effect of IL-9 and IL-5 on bone marrow–derived precursor cells in vitro. Our results suggest that IL-9 can play an important role in local eosinophilia by enhancing IL-5 activity.
Materials and methods
Animals
Six- to 8-week-old TG5 and FVB mice were used in this study under a protocol approved by the Institutional Animal Care and Use Committee of Magainin Pharmaceuticals Inc. TG5 mice were generated on a FVB/N background as described previously.14 Control mice (FVB/NJ) were purchased from Jackson Laboratory (Bar Harbor, ME).
Inflammation induced by thioglycolate
Thioglycolate-induced inflammation has the technical advantage of easy accessibility of the peritoneal cavity and recovery of large numbers of cells for further processing. Mice were injected intraperitoneally with 3 mL 3% Brewer thioglycolate (DIFCO, Detroit, MI) in phosphate-buffered saline (PBS). At 1, 6, 12, 24, 48, and 72 hours after injection, peritoneal cells were lavaged 3 consecutive times with 1 mL, 5 mL, and 5 mL sterile complete tissue culture medium (CTCM); RPMI 1640 (GIBCO BRL, Gaithersburg, MD), containing heat-inactivated fetal calf serum (FCS 10%; Hyclone, Logan, UT),l-glutamine (2 mM), 2-mercaptoethanol (5 mM), Hepes buffer (15 mM), penicillin (100 U/mL), and streptomycin (100 mg/mL) (GIBCO BRL). After centrifuging the 1-mL fraction (3000 rpm, 5 minutes, room temperature), the supernatant was aliquoted and stored at −20°C pending analysis of cytokines and released eosinophilic major basic protein (MBP). The cell pellet from the first fraction and the remaining fractions of lavage fluid were pooled and the cells washed twice with CTCM. The cells were resuspended in 5 mL CTCM and total cell numbers were counted. The cells were then aliquoted for protein extraction, tissue culture, and cytospin preparations. Bone marrow was extracted from the femur and tibia and single-cell suspension was prepared in sterile CTCM as above, for cytospins and cell culture. The small intestine, mesenteric lymph nodes, and lungs were also removed and immediately frozen in liquid nitrogen for investigation of RNA expression. Cytospin preparations were stained with Diff-Quik (Shandon, Pittsburgh, PA) and the cellular composition was assessed by standard morphology under immersion oil at × 400 magnification. At least 200 cells per slide were counted. The percentage and absolute numbers of different cell types were then calculated.
Cell cultures and assessment of proliferative responses
Peritoneal- and bone marrow–derived cells pooled from 2 to 4 mice were used in each experiment. For the proliferation assay, cells were plated at 2 × 106/mL in 96-well round bottom tissue culture plates in triplicate and incubated for 48 hours (or as otherwise stated) in a humidified atmosphere of 5% CO2 at 37°C. Cell proliferation was assessed by thymidine uptake measurements following standard procedures and analyzed using a Packard Top Count (Packard Instrument Company, Meriden, CT). To investigate the direct effects of exogenously added IL-9 on proliferative response, recombinant murine IL-9 (R&D Systems Inc, Minneapolis, MN) was added to the culture samples at concentrations ranging from 0.5 to 50 ng/mL. For studying the effects of IL-9 and IL-5 on cellular differentiation of bone marrow precursors, 106 peritoneal lavage or bone marrow cells were plated in 6-well plates in the absence or presence of mIL-5 (1 ng/ml), mIL-9 (5 ng/ml), or a combination of both cytokines. After 96 hours, cells were harvested; total and differential cell counts were assessed using cytospin preparations as described above.
Analysis of cytokine and chemokine production
Eotaxin, MCP-3, and RANTES messenger RNA (mRNA) levels were determined by Northern blot analysis. Total RNA was isolated from tissue samples using Trizol reagent (Gibco/BRL) following the manufacturer's protocol. Total RNA (10 μg) was electrophoresed on 1% formaldehyde gels and transferred to GeneScreen Plus membranes (NEN Life Sciences, Boston, MA). Membranes were probed with α-dCTP32 radiolabeled complementary DNA (cDNA) fragments generated by reverse transcriptase-polymerase chain reaction (RT-PCR) using random primer labeling (Boehringer Mannheim, Indianapolis, IN). The cDNA sequences for RT-PCR primer design of eotaxin (accession no. U40672), MCP-3 (accession no. S71251), and RANTES (accession no. M77747) were obtained from Genbank.
Protein levels for IL-9, IL-4, IL-5, and eotaxin were determined in the peritoneal lavage fluid by enzyme-linked immunosorbent assay (ELISA). Capture and detecting antibodies and recombinant proteins for IL-9, IL-4, and IL-5 were purchased from Pharmingen (San Diego, CA) and for eotaxin, from R&D Systems. Eight serially diluted samples of standards were prepared with a dilution factor of 0.33. Cytokine levels were calculated using standard curves generated in each plate.
Immunolabeling of eosinophilic MBP
To confirm the presence of eosinophilia and to investigate activation of eos by detecting the release of the major granule product we have developed a rabbit polyclonal antibody against the murine eos MBP.14 Antibodies to murine MBP were prepared by immunizing rabbits with a peptide representing the amino-terminal sequence of the protein conjugated to keyhole limpet hemocyanin (KLH). The N-terminal peptide (TCRYLLVRRAE-NH2 residues 1-11 of the mature protein) was synthesized by automated solid phase peptide synthesis using 9-fluorenylmethyloxycarbonyl protection chemistry and was purified by reverse phase high-performance liquid chromatography (HPLC). The purified peptide was coupled to KLH and the conjugated peptide was used to immunize rabbits in Freund complete adjuvant. The antisera obtained from the second and subsequent bleeds were used for the detection of MBP by Western blot analysis. Cells (2 × 105) were lysed in modified RIPA buffer (Tris HCl 50 mM, pH 8, NaCl 150 mM, Triton × 100 1%, sodium deoxycholate 0.25%, EGTA 1 mM, NaF 1 mM, leupeptin 10 mg/mL, Pefabloc 2 mM) and cell debris was removed by centrifugation. Peritoneal lavage fluid samples were diluted twice in Laemli buffer. Lavage or cell lysates were fractionated on sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) gels (4%-20% Novex gel) and electrophoretically transferred onto Immobion-P membrane (Millipore, Bedford, MA). Membranes were blocked in 5% nonfat milk, washed, and probed with rabbit polyclonal MBP antiserum (1/1000) and with horseradish peroxidase-linked antirabbit antibody (1/10 000; Amersham, Pharmacia, Biotech, Piscataway, NJ). The chemiluminescence detection kit (Pierce, Rockford, IL) was used for detection.
Transfer of spleen cells and anti-IL-9 treatment
Spleen cells were isolated from FVB and TG5 mice. Red blood cells were removed by NH4Cl (0.15 M) treatment followed by 3 washes with PBS. Groups of 8-week-old female FVB mice were intraperitoneally injected with a total volume of 200 μL PBS containing 107 spleen cells isolated from FVB or TG5 mice on day 1. At day 7, mice were bled and eosinophil number was analyzed as described above. At day 8, mice were treated intraperitoneally with 500 μg of a mouse monoclonal anti-IL-9 neutralizing antibody. The anti-IL-9 antibody was made in C57B1/6 mice using mouse IL-9-OVA complex as immunogen. Control mice received 100 μL mouse serum. On day 12, mice were bled and eosinophil numbers were analyzed as described above.
Dataanalysis
Data were expressed as mean ± SEM. Analysis of variance (ANOVA) was used to determine significant variance among the differently treated groups. If significant variance was found, the t test was used to analyze the differences between individual groups. A P value less than .05 was considered as significant. Data were analyzed with the MINITAB standard statistical package (Minitab Inc, State College, PA).
Results
IL-9 overexpression resulted in sustained eosinophilia in the peritoneal cavity of transgenic mice after thioglycolate injection
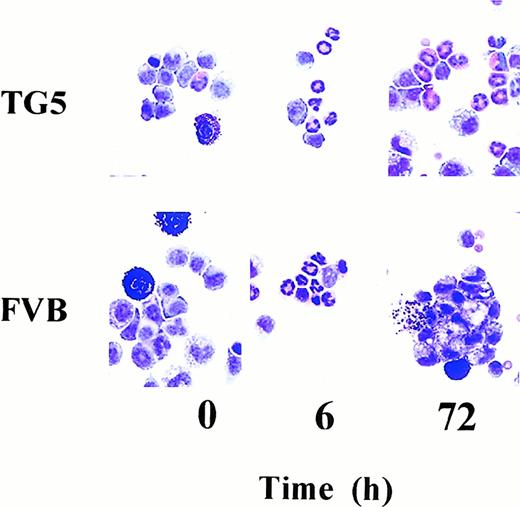
To study the role of IL-9 in development of tissue eosinophilia, we used a model of thioglycolate-induced peritoneal inflammation. Differential cell count of peritoneal cell lavage after thioglycolate administration demonstrated a sequential appearance of inflammatory cells beginning with a neutrophil influx, followed by eos that were finally replaced by macrophages in FVB mice (Figure1, Table1).
Cellular content of the peritoneal exudate harvested from TG5 and FVB mice before and after thioglycolate injection.
Photomicrographs of cytospin preparations were made from representative peritoneal lavage samples of IL-9 transgenic (TG5) and wild-type (FVB) mice. Following intraperitoneal injection with thioglycolate, mice were killed at different time points and their peritoneal lavage cellular content was analyzed. At 0 hour time point (before injection) both groups showed macrophages and scattered mast cells (left panels). In addition to these in TG5 mice a few eos are also seen in the peritoneal lavage fluid (upper left panel). Six hours after injection the picture is dominated by neutrophils in FVB and TG5 mice to a similar extent (middle panels). At 72 hours the neutrophils and eos disappeared and were replaced mainly by clustered macrophages in the peritoneal lavage of FVB mice (lower right panel). There was still a significant eosinophilia seen in TG5 mice (upper right panel). Cytospins were prepared and stained with Diff-Quik as described (original magnification × 1000).
Cellular content of the peritoneal exudate harvested from TG5 and FVB mice before and after thioglycolate injection.
Photomicrographs of cytospin preparations were made from representative peritoneal lavage samples of IL-9 transgenic (TG5) and wild-type (FVB) mice. Following intraperitoneal injection with thioglycolate, mice were killed at different time points and their peritoneal lavage cellular content was analyzed. At 0 hour time point (before injection) both groups showed macrophages and scattered mast cells (left panels). In addition to these in TG5 mice a few eos are also seen in the peritoneal lavage fluid (upper left panel). Six hours after injection the picture is dominated by neutrophils in FVB and TG5 mice to a similar extent (middle panels). At 72 hours the neutrophils and eos disappeared and were replaced mainly by clustered macrophages in the peritoneal lavage of FVB mice (lower right panel). There was still a significant eosinophilia seen in TG5 mice (upper right panel). Cytospins were prepared and stained with Diff-Quik as described (original magnification × 1000).
No difference in the kinetics of neutrophil infiltration was observed between FVB and TG5 mice (Figure 1, middle panel). At the peak of their appearance, 6 hours after injection, the proportions of neutrophils were 59% ± 8.6% and 46% ± 8.1% in FVB and TG5, respectively (Table 1). The presence of mast cells was constitutive in the peritoneal cavity of both strains (Figure 1, left panel) and no difference was observed after thioglycolate treatment.
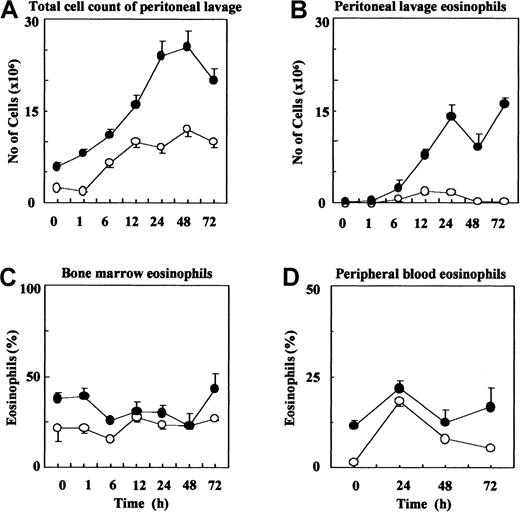
A remarkable strain difference was observed in both the extent and kinetics of eosinophilia (Figure 1, right panel and Table 1). Total cell and eos numbers in the peritoneal lavage were evaluated in FVB and TG5 mice before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection. Figure 2A shows that the average total cell numbers recovered from TG5 mice were significantly higher at each time point when compared to FVB mice (ANOVA:P < .01; Figure 2A). Moreover, eos reached a peak (20%, 1.96 × 106) 72 hours after thioglycolate injection followed by a decline in FVB mice (Figure 2B). In contrast, eosinophilia in TG5 mice started as early as 6 hours (20%, 2.42 × 106) and high levels (81%, 16.49 × 106) were still observed 72 hours after injection (ANOVA P < .001) (Figures 1 and 2B and Table1).
TG5 mice developed an enhanced and sustained eosinophilic inflammation following thioglycolate injection.
(A) Total cell numbers of peritoneal lavage samples were assessed using Coulter counter before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection as described. Counts per milliliter were adjusted to the volume recovered in each animal. (B) Absolute eos cell numbers in peritoneal lavage fluid were calculated using the number of total cells (as above) and the percentage of eos assessed from cytospin preparations in each animal. (C) Cytospin preparations from bone marrow samples were analyzed for eos cell counts before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection. (D) Peripheral blood smears from the tail vein were analyzed for eos cell counts before and 24, 48, and 72 hours after thioglycolate injection. Differential cell counts were made by counting at least 200 cells in each sample. Results are expressed as percentage of total counted cells. For each study values are expressed as mean ± SEM (n = 4 samples were studied for each time point and each genotype). Open circles indicate cell numbers in control (FVB) mice; solid circles, cell numbers in transgenic mice TG5.
TG5 mice developed an enhanced and sustained eosinophilic inflammation following thioglycolate injection.
(A) Total cell numbers of peritoneal lavage samples were assessed using Coulter counter before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection as described. Counts per milliliter were adjusted to the volume recovered in each animal. (B) Absolute eos cell numbers in peritoneal lavage fluid were calculated using the number of total cells (as above) and the percentage of eos assessed from cytospin preparations in each animal. (C) Cytospin preparations from bone marrow samples were analyzed for eos cell counts before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection. (D) Peripheral blood smears from the tail vein were analyzed for eos cell counts before and 24, 48, and 72 hours after thioglycolate injection. Differential cell counts were made by counting at least 200 cells in each sample. Results are expressed as percentage of total counted cells. For each study values are expressed as mean ± SEM (n = 4 samples were studied for each time point and each genotype). Open circles indicate cell numbers in control (FVB) mice; solid circles, cell numbers in transgenic mice TG5.
Quantitative evaluation of bone marrow preparations showed slightly but significantly higher eos numbers and more immature forms with eosinophilic cytoplasm in TG5 mice (ANOVA P < .05) when compared with FVB (Figure 2C). In peripheral blood samples TG5 mice displayed an elevated eos number (11.5% ± 2.1%) when compared with FVB mice (1.5% ± 1.6%; P < .01) at baseline (Figure2D). After injection there was an increase in eos in the peripheral blood of both strains but the numbers remained significantly higher in TG5 mice than in FVB mice (ANOVA P < .05; Figure 2D).
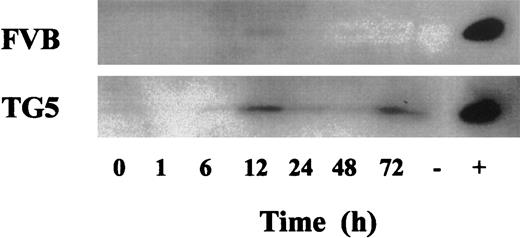
MBP release paralleled eosinophilia in peritoneal lavage
Active eos express an array of preformed highly toxic cationic proteins such as MBP. To confirm the presence and activation of eos in the peritoneal lavage, Western blot analysis was performed on supernatant of peritoneal lavage samples with a polyclonal antimurine MBP antiserum. In FVB mice, a transient appearance of the 14-kd MBP signal correlated with the peak of peritoneal eosinophilia 12 hours after thioglycolate injection (Figure 3). Similarly, in TG5 mice, MBP levels appeared at 12 hours and persisted up to 72 hours after thioglycolate injection. Although eosinophilia of the peritoneal cavity was associated with release of MBP in both strains, TG5 mice showed sustained and increased levels of MBP. These data indicate that eosinophilic tissue inflammation in vivo was associated with elevated levels of MBP, a molecular marker of mature eos.
MBP release in the peritoneal cavity in TG5 and FVB mice.
Representative Western blots of MBP content analysis from peritoneal lavage supernatant samples. Western blots were performed using a rabbit polyclonal antiserum developed in our laboratory as described. Each panel shows protein of expected molecular weight (14 kd) 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection. Eosinophilic cell lysates derived from IL-9 transgenic bone marrow preparations were used as positive controls. Splenic cell lysate preparations were used as negative control.
MBP release in the peritoneal cavity in TG5 and FVB mice.
Representative Western blots of MBP content analysis from peritoneal lavage supernatant samples. Western blots were performed using a rabbit polyclonal antiserum developed in our laboratory as described. Each panel shows protein of expected molecular weight (14 kd) 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection. Eosinophilic cell lysates derived from IL-9 transgenic bone marrow preparations were used as positive controls. Splenic cell lysate preparations were used as negative control.
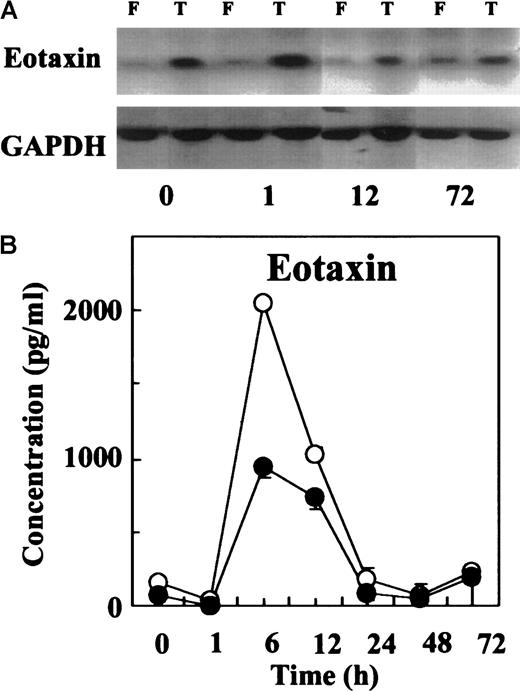
Eotaxin mRNA and protein production preceded influx of eos in the peritoneal lavage
The CC-type chemokines such as eotaxin, RANTES, MCP-1, and MCP-3 are potent factors for attracting eos to sites of allergic inflammation. To study whether the rapid and enhanced eos influx in TG5 mice in response to thioglycolate stimulation was associated with up-regulation of CC chemokines, the expression of eotaxin, RANTES, and MCP-3 genes was analyzed in mesenteric lymph nodes by Northern blot. Although mRNA expression for MCP-3 and RANTES remained below the detection levels (data not shown), a constitutive expression of eotaxin was observed in the mesenteric lymph nodes of TG5 but not FVB mice. Thioglycolate injection up-regulated mRNA expression for eotaxin 1 hour after thioglycolate injection in both strains (Figure4A). Despite the higher mRNA expression in the mesenteric lymph nodes, levels of eotaxin protein in the peritoneal fluid of TG5 mice were not statistically different from FVB mice by ELISA. (Figure 4B). These data suggest that factors other than eotaxin may be involved in promoting eosinophilia to these sites in TG5. However, eotaxin had parallel kinetics in the 2 strains with a peak 6 hours after injection, preceding the peak of eosinophilia (Figure 4B) suggesting that eotaxin may play a role in part for initial eos recruitment.
Eotaxin expression in TG5 and FVB mice.
(A) Representative Northern blots showing eotaxin mRNA production in mesenteric lymph nodes from TG5 (T) and FVB (F) mice. Mesenteric lymph nodes were harvested before and 1, 12, and 72 hours after thioglycolate injection. Hybridization with a GAPDH probe confirmed that comparable amounts of RNA had been loaded in each lane. (B) Time course of immunoreactive eotaxin protein release in the peritoneal lavage was analyzed using ELISA. Supernate samples were harvested before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection, respectively. Values are expressed in pg/mL as mean ± SEM (n = 4 for each time point and each genotype). Open circles indicate cell numbers in FVB mice; solid circles, cell numbers in TG5 mice.
Eotaxin expression in TG5 and FVB mice.
(A) Representative Northern blots showing eotaxin mRNA production in mesenteric lymph nodes from TG5 (T) and FVB (F) mice. Mesenteric lymph nodes were harvested before and 1, 12, and 72 hours after thioglycolate injection. Hybridization with a GAPDH probe confirmed that comparable amounts of RNA had been loaded in each lane. (B) Time course of immunoreactive eotaxin protein release in the peritoneal lavage was analyzed using ELISA. Supernate samples were harvested before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection, respectively. Values are expressed in pg/mL as mean ± SEM (n = 4 for each time point and each genotype). Open circles indicate cell numbers in FVB mice; solid circles, cell numbers in TG5 mice.
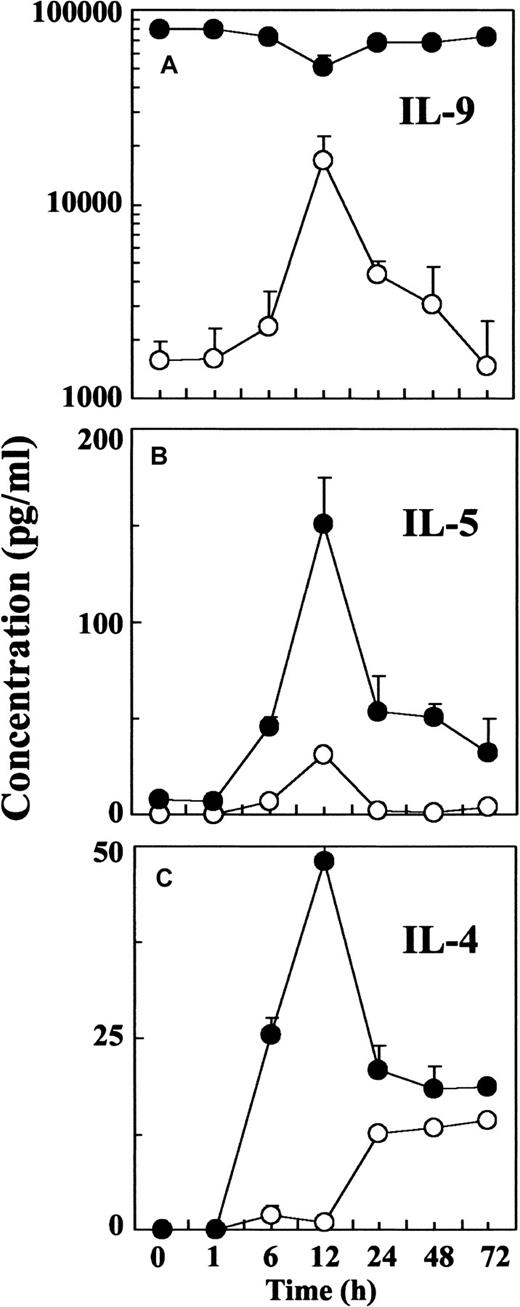
TG5 mice showed enhanced IL-4 and IL-5 production in response to thioglycolate injection
Analysis of cytokine production in the peritoneal lavage showed that the peak and resolution of eosinophilia observed in peritoneal lavage closely followed the kinetics of IL-9 release in FVB mice (Figure 5A). In addition, the peak of IL-9 production in these mice coincided with the peak of IL-5 release 12 hours after thioglycolate injection. IL-5 levels returned to the baseline (< 5 pg/mL) by 24 hours in FVB mice (Figure 5B). Transgenic mice that constitutively showed approximately 80 ng/ml IL-9 in the peritoneal lavage fluid produced 10-fold higher levels of IL-5, which failed to return to baseline even 72 hours after injection (Figure 5B). IL-4 production started earlier in TG5 mice and showed similar kinetics to IL-5 release with peak levels 50-fold higher than in FVB mice 12 hours after injection (Figure 5C).
Cytokine production in the peritoneal lavage of TG5 and FVB mice after thioglycolate injection.
Time course of immunoreactive IL-9 (A), IL-5 (B), and IL-4 (C) protein release in the peritoneal lavage was analyzed using ELISA. Supernate samples were harvested before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection, respectively. Open circles indicate cell numbers in FVB mice; solid circles, cell numbers in TG5 mice. Values are expressed in pg/mL as mean ± SEM (n = 4 for each time point and each genotype).
Cytokine production in the peritoneal lavage of TG5 and FVB mice after thioglycolate injection.
Time course of immunoreactive IL-9 (A), IL-5 (B), and IL-4 (C) protein release in the peritoneal lavage was analyzed using ELISA. Supernate samples were harvested before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection, respectively. Open circles indicate cell numbers in FVB mice; solid circles, cell numbers in TG5 mice. Values are expressed in pg/mL as mean ± SEM (n = 4 for each time point and each genotype).
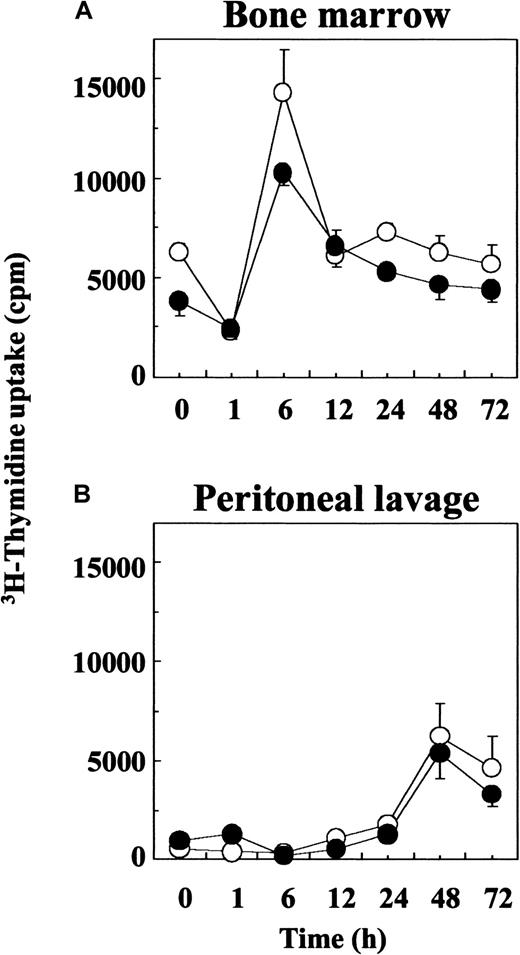
IL-9 did not enhance proliferative ability of bone marrow-derived cells
A potential mechanism by which IL-9 works to enhance eosinophilia may be through the enhanced stimulation of CD34+ progenitor cells. To assess this hypothesis, we analyzed the proliferative response of progenitor cells from the bone marrow and the peritoneal cavity by 3H-thymidine incorporation before and at different time points after thioglycolate injection. In both strains, bone marrow cells showed a sharp increase of proliferation 6 hours after injection (Figure 6A). In the peritoneum the numbers of proliferating cells also increased and reached a peak 48 hours after thioglycolate injection in both strains (Figure 6B). There was no difference in the proliferation of cells from either bone marrow or peritoneal lavage from TG5 or FVB mice, suggesting that no global difference occurs on the activation of progenitor cells from TG5 mice, which exhibit a higher degree of eosinophilia after thioglycolate injection compared to FVB mice.
Proliferative capability of bone marrow derived precursors from TG5 and FVB mice after thioglycolate injection.
3H-thymidine uptake was measured in 48-hour cultures as described. Cells were harvested from bone marrow (A) and peritoneal lavage (B) before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection. Cells were pooled from 2 to 4 animals in each group and plated in triplicates. Open circles indicate cell number in FVB mice; solid circles, cell numbers in TG5 mice. Values are mean ± SEM (n = 4 separate experiments).
Proliferative capability of bone marrow derived precursors from TG5 and FVB mice after thioglycolate injection.
3H-thymidine uptake was measured in 48-hour cultures as described. Cells were harvested from bone marrow (A) and peritoneal lavage (B) before and 1, 6, 12, 24, 48, and 72 hours after thioglycolate injection. Cells were pooled from 2 to 4 animals in each group and plated in triplicates. Open circles indicate cell number in FVB mice; solid circles, cell numbers in TG5 mice. Values are mean ± SEM (n = 4 separate experiments).
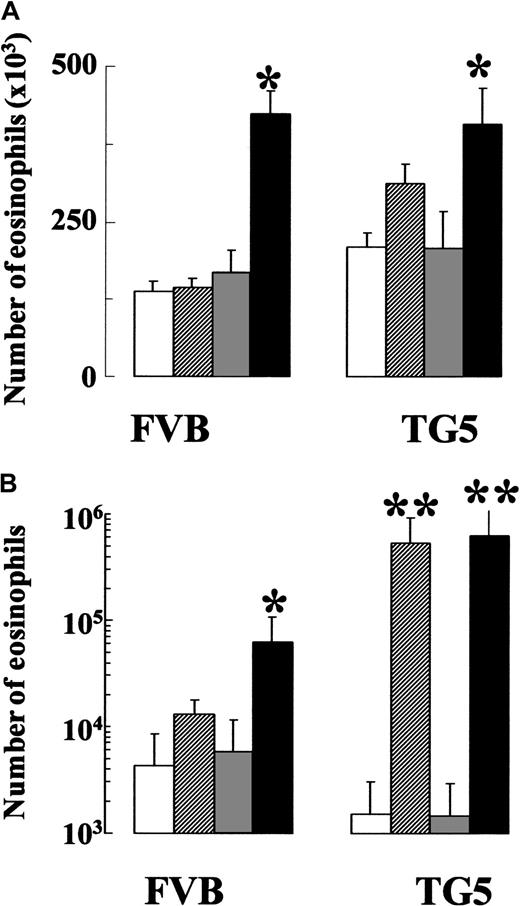
IL-5 and IL-9 showed synergistic effects in inducing eosinophilia
Interleukin-5 is a potent eos differentiation and maturation factor. To understand the effect of IL-9 on eos maturation and its relationship to IL-5, we assayed the effects of IL-9 and IL-5 alone or in combination on bone marrow and peritoneal lavage isolated cells in vitro. Bone marrow was harvested from naı̈ve FVB or TG5 mice, and cells were cultured in the presence of IL-5, IL-9, or their combination. Cultures plated in the presence of IL-5 alone resulted in the formation of eos, in contrast to cultures plated in IL-9 alone where no eos were observed after 4 days of culture. Interestingly, cultures to which IL-5 and IL-9 were added together showed significantly increased numbers of eos from bone marrow cells derived from both untreated FVB and TG5 mice (Figure7A), suggesting that IL-9 can increase IL-5 responsiveness of bone marrow precursor cells. In light of the data above, we next determined whether the enhanced eosinophilia observed in the peritoneal cavity of TG5 mice was due to an increase in IL-5 responsiveness of bone marrow precursor cells found locally in the peritoneum. To test this hypothesis, we performed a similar experiment using peritoneal lavage cells harvested 48 hours after thioglycolate injection. We chose the 48-hour time point because of the high proliferation rate of these cells (see above), suggesting the presence of precursor cells in this population. In FVB mice, whereas IL-9 alone had no effect, the combination of IL-5 and IL-9 induced a significant increase in eos number in comparison with IL-5 alone (P < .05; Figure 7B), confirming the synergism between IL-5 and IL-9 observed previously in bone marrow cell culture. Furthermore, addition of IL-5 strikingly increased the number of eos in cultures from TG5 (but not FVB) mice, when compared with the effects of medium alone (P < .01; Figure 7B). Exogenous addition of IL-9 did not further increase the eos number (Figure 7B). In contrast to IL-5, addition of IL-4 had a moderate effect on increasing eos in cultured peritoneal cells from both FVB and TG5 mice. The numbers were 8467 ± 1495 (with IL-5) versus 2050 ± 673 (with IL-4) compared with 960 ± 370 (medium alone) for FVB, and 623 467 ± 72 137 (with IL-5) versus 115 867 ± 22 122 (with IL-4) compared with 64 933 ± 15 606 (medium alone) for TG5 (n = 3 for each point). The minimal increase of eos in TG5 cells cultured in the presence of IL-4 indicated that IL-4 has no synergistic effect with IL-9 on eos maturation. Moreover, IL-4 has no synergistic effect with IL-5 on eos maturation (data not shown). These results suggest that the significantly higher IL-4 levels observed in vivo most likely play a role different from that of IL-5 in sustaining eosinophilia in the IL-9 transgenic mice.
Synergistic effects of IL-5 and IL-9 in eos maturation.
Cells harvested from bone marrow of naı̈ve animals (A) and peritoneal lavage of thioglycolate-injected mice (B) were cultured in medium alone (open bars), with IL-5 (hatched bars), with IL-9 (gray bars), and with the combination of IL-5 and IL-9 (black bars) for 96 hours. After 96 hours cell cultures were analyzed for total and eos numbers. *P < .05; **P < .01 denotes significant differences between the marked group and the medium controls (open bars). Values are expressed as mean ± SEM (n = 4 separate experiments). In each experiment 2 to 4 samples were pooled from each group before culture.
Synergistic effects of IL-5 and IL-9 in eos maturation.
Cells harvested from bone marrow of naı̈ve animals (A) and peritoneal lavage of thioglycolate-injected mice (B) were cultured in medium alone (open bars), with IL-5 (hatched bars), with IL-9 (gray bars), and with the combination of IL-5 and IL-9 (black bars) for 96 hours. After 96 hours cell cultures were analyzed for total and eos numbers. *P < .05; **P < .01 denotes significant differences between the marked group and the medium controls (open bars). Values are expressed as mean ± SEM (n = 4 separate experiments). In each experiment 2 to 4 samples were pooled from each group before culture.
Cell death was marked in both mouse strains when peritoneal lavage cells were cultured with medium or IL-9 alone because eos decreased from 16% to 1% of the original in these cultures. The combination of IL-5 and IL-9 significantly increased numbers of FVB cells in the cultures; however, the number of eos was still only 76% of the original (P < .05). By contrast, in TG5 mice the number of eos exceeded the initial number in the presence of IL-5 (152%) and in the presence of IL-5 and IL-9 (175%) by the end of the peritoneal cell culture period indicating de novo eosinophilopoiesis.
Adoptive transfer of TG5 spleen cells induces peripheral blood eosinophilia in an IL-9–dependent manner
To prove that IL-9 is responsible for eliciting eosinophilia in vivo, we performed adoptive transfer experiments using splenic lymphocytes from TG5 and control (FVB) mice. IL-9 concentrations measured 7 days after the transfer rose to 200 pg/mL in FVB mice that received TG5 spleen cells. By contrast, no detectable serum IL-9 was observed in FVB mice injected with FVB spleen cells. Seven days following adoptive transfer, mice were bled and eos numbers were determined as described above. In recipients of TG5 spleen cells the percentage of eos in peripheral blood leukocytes significantly increased to 14.6% ± 2.25% while it remained 1.8% ± 0.37% in recipients of FVB cells (P < .01, n = 5). Eight days after transfer, mice were treated intraperitoneally with 500 μg of a mouse monoclonal anti-IL-9 neutralizing antibody. Peripheral blood eosinophilia was investigated again 4 days later and was found completely abrogated in mice treated with anti-IL-9 antibody (1.6% ± 0.5%; P < .01, n = 5) but not in sham-treated mice (11.0% ± 3.60%).
Discussion
The genes for IL-9 and its receptor have recently been strongly implicated in the pathogenesis of allergic asthma in humans16-18 and in murine models of airway hyperresponsiveness.10,19,20 We have previously shown in murine models that intratracheal administration of recombinant murine IL-9 in naı̈ve C57BL/6 mice resulted in airway eosinophilia20 and that IL-9 transgenic mice developed an exaggerated Th2-type response including an abnormally enhanced tissue eosinophilia following allergic sensitization.21 These studies suggested a role for IL-9 in the development of tissue eosinophilia but its mechanism of action remained unclear. In this report we show that in vivo expression of IL-9 is capable of eliciting and sustaining tissue eosinophilia, and that this cytokine may be pivotal in the maturation process of eos precursors.
A model of thioglycolate-induced local inflammatory response was used to investigate the changes in IL-9 transgenic (TG5) and normal wild-type (FVB) mice. Thioglycolate is an irritant that generates rapid inflammatory responses through sequential influx of neutrophils, lymphocytes, eos, and macrophages from peripheral blood and bone marrow.22 Analysis of the cellular content of the peritoneal inflammatory exudate revealed that IL-9 transgenic mice developed a massive, persistent eosinophilia after thioglycolate injection. The kinetics of neutrophil infiltration in the peritoneum was not affected in TG5 mice suggesting a specific effect of IL-9 on the eos lineage. Quantitative analysis of bone marrow, peripheral blood, and peritoneal lavage samples confirmed that constitutive IL-9 expression in TG5 mice was associated with an enhanced eosinophilia in response to thioglycolate stimulation.
We validated the presence and activation of these cells by investigating the supernatant fractions of peritoneal lavage samples with an anti-MBP antiserum developed in our laboratory. Active eos release preformed toxic granule proteins; the most abundant of them is MBP. Its functional relevance is supported by studies showing that MBP is involved in tissue destruction.23 In this model, eosinophilic tissue inflammation was associated with release of MBP in both FVB and TG5 mice with the latter strain showing increased levels and sustained release.
Mobilization of peripheral blood and bone marrow eos is a critical early step in their trafficking to the site of inflammatory reactions. In a previous study, we have shown that IL-9 induces CC chemokine expression in lung epithelial cells, which is associated with airway eosinophilia in IL-9 transgenic mice.24 The enhanced and persistent eosinophilia in TG5 mice observed in our present model could, however, be the result of not only an influx of mature cells but also an up-regulated maturation of bone marrow precursors promoted by IL-9. Recruitment of mature eos into the site of inflammation is largely dependent on elevated chemokine release.25,26 The CC chemokine eotaxin is a potent and specific chemoattractant for these cells,26,27 but other chemokines such as RANTES27 and MCP-328 were also shown to have significant chemotactic activities on eos. Thioglycolate-induced peritoneal inflammation resulted in undetectable levels of MCP-3 and RANTES (data not shown), but we found a constitutive expression of eotaxin mRNA in the mesenteric lymph nodes, which was up-regulated 1 hour after thioglycolate injection in both TG5 and FVB mice. Although we found higher levels of eotaxin mRNA expression in TG5 mice, the immunoreactive protein released to the peritoneal cavity (detected by ELISA in the supernatant and by Western blot in the cellular fraction of peritoneal lavage) was lower in these animals. This discordance may be due to the binding of eotaxin to the abnormally high numbers of eos found in TG5 mice, and as a consequence, a rapid degradation that resulted in reduced levels of eotaxin detection by immunologic methods.
Interleukins 4 and 5 may play elementary roles in the development of eosinophilia by multiple pathways.29,30 A blockade of either of these cytokines significantly impairs or abolishes the eosinophilic response on allergic sensitization.31,32 IL-5 is considered as the key cytokine in selective eos recruitment, activation, survival, and chemotaxis, and it is thought to be the exclusive cytokine to promote terminal differentiation of the committed eos precursor.3 Although the direct effect of IL-9 on the production of these cytokines is unclear, it appears that high levels of IL-9 expression in transgenic mice markedly enhanced IL-4 and IL-5 release in response to thioglycolate injection providing a significant positive feedback on the maintenance of tissue eosinophilia in transgenic mice. The cellular source of IL-4 and IL-5 in this inflammatory response is not clear, but it is possible that IL-9–primed Th2 cells or resident mast cells were capable of releasing these cytokines in a coordinated fashion, with a single peak 12 hours after thioglycolate injection. FVB mice showed that the peak and resolution of eosinophilia closely followed the kinetics of IL-5 production, which importantly also coincided with IL-9 release. In addition, the sustained eosinophilic response observed in the peritoneal cavity of TG5 mice was associated with persisting production of IL-5. Thus, together with IL-5, IL-9 appears to have a regulatory role in development of eosinophilia.
Although IL-4 production was also up-regulated in TG5 mice, we found no detectable levels of this cytokine during the course of eosinophilia in normal FVB mice. IL-4 had moderate effect on eosinopoiesis in cell cultures even in TG5 mice, indicating a lack of synergism. This cytokine may contribute to tissue eosinophilia through a mechanism different from that of IL-5. Thus, IL-4 is less significant than IL-5 or IL-9 in the development of eosinophilia in the thioglycolate model, but its supportive role in the enhanced changes in TG5 mice cannot be excluded.
The ability to mount an eosinophilic inflammation may not depend only on local factors but also on the capacity of bone marrow to undergo lineage skewing.4 We have recently shown that IL-9 is able to up-regulate IL-5Rα expression on a human cell line,21suggesting that IL-9 may increase IL-5 responsiveness of precursor cells. To study the role of IL-9 on eos maturation we investigated the in vitro effects of IL-9 and IL-5 on cell populations recovered from bone marrow and peritoneal lavage. Although IL-9 had no direct effect on bone marrow cell proliferation,33 in combination with IL-5 it significantly increased the number of eos in cell cultures. Eos precursors have been shown to be increased in the blood of atopic patients after allergen challenge indicating that these cells may also mature at the site of inflammation during an inflammatory response.4 To study whether IL-9 plays a role in local maturation of bone marrow precursors in the peritoneum we repeated the in vitro experiments using cells lavaged from the peritoneal cavity of thioglycolate-injected mice. As assessed by thymidine incorporation, the proportion of proliferating bone marrow precursors in the peritoneal cavity appeared to be the highest 48 hours after injection. Because the susceptibility of this population of peritoneal cells to the in vitro effects of IL-9 and IL-5 was also apparently the highest in comparison with cells harvested at other time points, we selected these cells to study for eosinophilopoiesis. Similarly to the bone marrow cell cultures, in peritoneal lavage cells we found a synergistic effect of IL-5 and IL-9 in inducing eosinophilia. Interestingly, IL-5 alone strikingly increased the number of eos from peritoneal cells of TG5 mice. Eos numbers increased more than 50% by the end of the cell culture period in these mice suggesting that in addition to augmented survival, eosinophilopoiesis may have significant contribution to the observed eosinophilia. Thus, our in vivo and in vitro data strongly suggest the possibility that local expression of IL-9 primes tissues to give an exaggerated eosinophilic response to any stimulus that induces the production of IL-5 or other eos activators.
Ablating IL-9 in transgenic mice is difficult mostly because of the high concentrations of IL-9 (≥ 1 μg/mL) found in the serum of these mice.9 In addition, mice deficient in IL-9 are currently not available. Thus, to prove that IL-9 is responsible for inducing eosinophilia in vivo, we performed adoptive transfer experiments using splenic lymphocytes from TG5 and control (FVB) mice. TG5 spleen cells elicited significant IL-9 levels as well as marked peripheral eosinophilia in wild-type recipients. Because this peripheral blood eosinophilia was completely abolished following neutralizing anti-IL-9 antibody treatment, we conclude that adoptive transfer of IL-9 transgenic spleen cells induced eosinophilia through an IL-9–dependent mechanism. This confirms a previous study in which mice producing blocking anti-IL-9 antibodies failed to develop eosinophilia in response to intestinal parasite infections.34
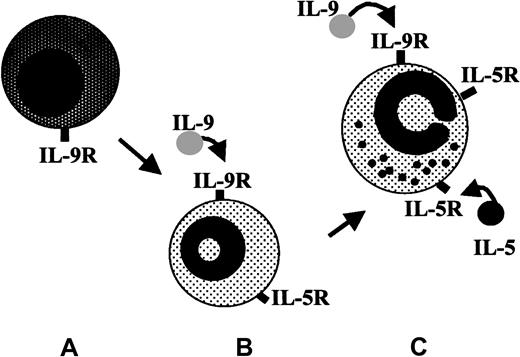
In conclusion, TG5 mice had a markedly enhanced and sustained local eosinophilic response to thioglycolate injection associated with increased eotaxin mRNA production IL-4 and IL-5 release. For the first time we demonstrated a synergistic effect of IL-9 and IL-5 on eos maturation in a primary cell culture, indicating that IL-9 may induce eosinophilia through IL-5–dependent pathways. We propose here a novel mechanism in which IL-9 has a major role in bone marrow lineage skewing that results in development and maintenance of tissue eosinophilic inflammation (Figure 8).
A model for the modulatory effects of IL-9 on eosinophilopoiesis.
IL-9 may increase susceptibility of noncommitted bone marrow precursor cells (A) to IL-5, thereby enhancing maturation of committed eos precursors (B) and facilitating IL-5–dependent eos functions (C).
A model for the modulatory effects of IL-9 on eosinophilopoiesis.
IL-9 may increase susceptibility of noncommitted bone marrow precursor cells (A) to IL-5, thereby enhancing maturation of committed eos precursors (B) and facilitating IL-5–dependent eos functions (C).
Acknowledgments
The authors are deeply indebted to Dr Hirohito Kita (Mayo Clinic, Rochester, MN) and to Dr Michael F. Beers (University of Pennsylvania Medical School, Philadelphia, PA) for their constructive advice and helpful comments.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Roy C. Levitt, Magainin Pharmaceuticals, 5110 Campus Dr, Plymouth Meeting, PA 19462; e-mail:rlevitt@magainin.com.