Notch-mediated cellular interactions are known to regulate cell fate decisions in various developmental systems. A previous report indicated that monocytes express relatively high amounts of Notch-1 and Notch-2 and that the immobilized extracellular domain of the Notch ligand, Delta-1 (Deltaext-myc), induces apoptosis in peripheral blood monocytes cultured with macrophage colony-stimulating factor (M-CSF), but not granulocyte-macrophage CSF (GM-CSF). The present study determined the effect of Notch signaling on monocyte differentiation into macrophages and dendritic cells. Results showed that immobilized Deltaext-myc inhibited differentiation of monocytes into mature macrophages (CD1a+/−CD14+/− CD64+) with GM-CSF. However, Deltaext-myc permitted differentiation into immature dendritic cells (CD1a+CD14−CD64−) with GM-CSF and interleukin 4 (IL-4), and further differentiation into mature dendritic cells (CD1a+CD83+) with GM-CSF, IL-4, and tumor necrosis factor-α (TNF-α). Notch signaling affected the differentiation of CD1a−CD14+macrophage/dendritic cell precursors derived in vitro from CD34+ cells. With GM-CSF and TNF-α, exposure to Deltaext-myc increased the proportion of precursors that differentiated into CD1a+CD14− dendritic cells (51% in the presence of Deltaext-myc versus 10% in control cultures), whereas a decreased proportion differentiated into CD1a−CD14+ macrophages (6% versus 65%). These data indicate a role for Notch signaling in regulating cell fate decisions by bipotent macrophage/dendritic precursors.
Introduction
Notch-mediated cellular interactions have been shown to play a central role in regulating cell fate decisions of bipotent precursors in numerous developmental systems.1 As demonstrated in neural cell development from neural/epidermal precursors in Drosophila or vulval cell specification inCaenorhabditis elegans,2,3 Notch receptors expressed by bipotential progenitors are activated by neighboring progenitors bearing Notch ligands, leading to inhibition of differentiation of the Notch-expressing cells along a fate-specific pathway. These cells remain undifferentiated or differentiate along an alternate pathway in the presence of appropriate stimuli (lateral inhibition).1
Notch receptors are evolutionarily conserved transmembrane receptors, which are made up of an extracellular ligand-binding domain with epidermal growth factor (EGF)–like repeats and a cytoplasmic domain required for signal transduction.4 Four vertebrate forms, Notch-1, -2, -3, and -4,5-9 have currently been identified. Vertebrate Notch ligands, identified as Jagged-1 and -2 and Delta-1 , -2, -3, and -410-15 are transmembrane proteins whose extracellular domains contain multiple EGF-like repeats and a DSL domain (Delta, Serrate, LAG-2), all of which are required for binding and activating the Notch receptor.4 Notch receptors, on interaction with Notch ligand, undergo at least 2 steps of proteolytic cleavage, release the intracellular receptor domain (Notch-IC), and subsequently translocate to the nucleus where they often associate with the DNA-binding transcription factor, CSL (CBF-1, suppressor of hairless, Lag-1: or RBP-Jκ).16,17 This complex of the Notch-IC and the CSL transcription factor has been shown to transactivate the basic helix-loop-helix transcription factorHes1 gene, a homologue of E(Spl), and then affect downstream genes.1,18 19
Several lines of evidence have suggested a role for Notch signaling in hematopoietic cell development.20 We previously found Notch-1 messenger RNA in bone marrow cells, including CD34+precursors.21 Furthermore, we and others detected Notch protein in hematopoietic progenitors and Notch ligand, Jagged-1, in stroma cells.22-25 In addition, we found that hematopoietic precursor cell populations increased after incubation with Notch ligands, Jagged-1,22 23 or Delta-1 (B.V.-F., manuscript in preparation, July 2001), suggesting that Notch signaling may play an important role in determining self-renewal and cell lineage decisions in hematopoiesis.
Recently, we found that peripheral blood monocytes express relatively high amounts of Notch-1 and Notch-2, and that an immobilized form of the extracellular domain of the Notch ligand, Delta-1 (Deltaext-myc), induces monocytes to undergo apoptosis with macrophage colony-stimulating factor (M-CSF).26 Apoptosis occurred only if Deltaext-myc was immobilized. However, apoptosis did not occur with immobilized Deltaext-myc and granulocyte-macrophage CSF (GM-CSF), suggesting a role for Notch signaling in the cytokine-specific regulation of monocyte survival and differentiation.26
Monocytes are known to differentiate into macrophages with GM-CSF or M-CSF, whereas with GM-CSF and interleukin 4 (IL-4) they differentiate into CD1a−CD14+ immature dendritic cells and, with the addition of tumor necrosis factor-α (TNF-α), they differentiate into CD83+ mature dendritic cells.27 Moreover, CD1a−CD14+cells that have been derived in vitro from CD34+ cells with GM-CSF and TNF-α have also been shown to be bipotent precursors of macrophages and dendritic cells.28 29 We therefore tested the effect of Notch signaling on the cell fate decision of each of these bipotent precursors.
We found that immobilized Deltaext-myc inhibited the differentiation of monocytes into mature macrophages with GM-CSF, but permitted their differentiation into dendritic cells in the presence of GM-CSF and IL-4, with or without TNF-α. We also found that immobilized Deltaext-myc permitted CD34+cell-derived CD1a−CD14+ precursors cultured with GM-CSF and TNF-α to adopt a dendritic cell fate, but not a macrophage fate. These data reveal a potential role for the Notch pathway in regulating cell fate choices by bipotent macrophage/dendritic cell precursors.
Materials and methods
Separation of peripheral monocyte and CD34+cells
Peripheral blood monocytes were purified by negative selection as described previously.26 CD34+ cells were isolated from healthy adult bone marrow by using mouse anti-CD34 antibody, 12.8, followed by antimouse immunoglobulin M (IgM) Microbeads, and VS+ separation column (Miltenyi Biotec, Bergisch Gladbach, Germany) according to the manufacturer's instructions.
Antibodies and immunofluorescence studies
Immunofluorescence studies were performed as previously described26 using a FACScan (Becton Dickinson, Mountain View, CA), excluding dead cells stained with propidium iodide, and using fluorescein isothiocyanate (FITC)–labeled antibodies against CD14 (Leu-M3), HLA-DR (both from Becton Dickinson, Sunnyvale, CA), CD40, CD64 (Pharmingen, San Diego, CA), CD83 (Immunotech, Marseilles, France), or phycoerythrin (PE)-labeled IgG antibodies against CD80 (Becton Dickinson), CD86 (Pharmingen), CD1a, CD14 (My4), and CD54 (all from Immunotech). The antihuman myc antibody, 9E10 F(ab′)2, was prepared from the 9E10 hybridoma in our laboratory as reported previously.26
Immunohistochemistry
Cells were fixed with 2% paraformaldehyde dissolved in phosphate-buffered saline (PBS), permeabilized with a 0.1% solution of Triton X-100 (Sigma, St Louis, MO), and incubated overnight at 4°C with 2% goat serum (Santa Cruz Biotechnology, Santa Cruz, CA) in a humidified chamber. Cells were stained with a rabbit anti-RelB antibody at 1:1000 dilution for 4 hours at room temperature, followed by biotinylated goat antirabbit antibody (1:1000, both from Santa Cruz Biotechnology), and streptavidin-conjugated FITC (1:1000; Biosouce/Tago, Camarillo, CA). Nuclei were counterstained with DAPI. At least 200 DAPI-stained nuclei were counted in a blinded fashion, and then the percentage of DAPI-stained nuclei that also expressed RelB was quantitated. We performed 3 independent experiments and calculated the mean percentage of cells with RelB expression in nuclei. Microscope images were collected with Delta Vision (Applied Precision, Issaquah, WA).
Extracellular domain of Delta-1 generation
The extracellular domain of Delta-1 containing 6 myc-tags (Deltaext-myc) was prepared as reported previously.26 Briefly, the construct containing complementary DNA (cDNA) sequences of the extracellular domain of human Delta-1 and 6 consecutive myc epitopes was subcloned into the expression vector pcDNA3.1/amp (Invitrogen, San Diego, CA) that added 6 histidines to the sequence, and then electroporated into NSO myeloma cells. G418-resistant clones were screened for secretion of the fusion proteins using a quantitative enzyme-linked immunosorbent assay, and clones that generated the highest amounts of construct were expanded into roller bottles (Dulbecco modified Eagle medium with 1.0% Nutridoma NS [Boehringer Mannheim, Indianapolis, IN]) for mass production of proteins. Two liters of conditioned medium were generated.
Deltaext-myc was purified from conditioned medium generated from Deltaext-myc-transfected NSO cells as reported previously.26 For a control for studies with Deltaext-myc, control conditioned medium generated by untransfected NSO cells was similarly prepared as reported previously.26 In brief, conditioned medium from either cells expressing Deltaext-myc or control untransfected cells was concentrated, dialyzed against PBS, and subsequently bound to a nickel column (Ni-NTA [Nitrilotriacetic acid] agarose; Qiagen, Chatsworth, CA) using the His-Bind buffer kit (Novagen, Madison, WI). Bound protein was washed extensively with wash buffer (His-Bind buffer supplemented with 1.0% Tween-20 and 20 mM β-mercaptoethanol) to remove nonspecific binding proteins. Proteins were then eluted with increasing concentrations of imidazole. Fractions containing Deltaext-myc were identified with Western blots and subsequently pooled, dialyzed against PBS, and concentrated about 8-fold. To assess purity, proteins were separated using 8% sodium dodecyl sulfate–polyacrylamide gel electrophoresis and Coomassie-stained. The purity of Deltaext-myc was 84%. Western blots were performed as previously described.23 We used Deltaext-myc at 1 μg/mL for experiments based on the data previously reported.26 The same fractions from the control elution were pooled, dialyzed, and concentrated into the same volume as the Deltaext-myc solution. We used control conditioned solution at a protein concentration of approximately 0.18 μg/mL, which is similar to that of nonspecific protein (0.16 μg/mL) included in the Deltaext-myc preparation. No effect was seen with control solution up to 5 μg/mL.
Cellcultures
Isolated monocytes (5000-20 000/well) were cultured in the 96-well plates with 10% fetal calf serum (FCS) Iscoves modified Dulbecco medium (IMDM) containing designated cytokines and either immobilized Deltaext-myc or control medium as described previously.26 Briefly, immobilized Deltaext-myc and control medium were prepared as follows. The 96-well plates were coated with a mouse anti-myc antibody, 9E10, in the form of an F(ab′)2 fragment at the concentration of 10 μg/mL for 30 minutes at 37°C. After washing, coated wells were blocked with IMDM containing 20% fetal bovine serum (FBS; Hyclone, Logan, UT) for 30 minutes at 37°C. After washing, 1 μg/mL Deltaext-myc or control medium was applied to the coated wells for 30 minutes. Cytokines were used at the following concentrations: 10 ng/mL M-CSF (Peprotech, Rocky Hill, NJ), 100 ng/mL GM-CSF (Amgen, Thousand Oaks, CA), 20 ng/mL TNF-α (Peprotech), and 10 ng/mL IL-4 (Sigma). Cultured cells were harvested after incubation with 200 μM EDTA PBS (Gibco, Grand Island, NY) for 15 minutes to enhance the detachment of adherent cells.
The CD34+ cells were first cultured in 6-well plates containing 10% FCS IMDM and c-kit ligand (100 ng/mL; Amgen), GM-CSF, and TNF-α (20 ng/mL) at 2 × 104/mL to 4 × 104/mL. After 5 days, cells were harvested, and CD1a−CD14+ cells were isolated by fluorescence-activated cell sorting and cultured in 24-well plates at 2 × 104 cells/well for 8 days with 10% FCS containing GM-CSF, TNF-α (20 ng/mL), and either immobilized Deltaext-myc or control medium.
Mixed leukocyte culture
Cultured cells were tested in mixed leukocyte culture (MLC) for stimulatory activity. Peripheral blood mononuclear cells (PBMCs) were obtained by centrifuging on Ficoll-Hypaque (density 1.077) and used as responder cells. Stimulator cells were incubated in RPMI-HEPES containing 15% human AB serum, 100 U/mL penicillin-streptomycin, 100 U/mL l-glutamine, and 1 mM sodium pyruvate. After irradiation at 3000 cGy, increasing numbers of stimulator cells were incubated with PBMC at 5 × 104/well in round-bottomed 96-well plates. Cultures were maintained in a humidified atmosphere at 37°C and 5% CO2. Cells were pulsed with 37 kBq/well 3H-thymidine for 18 hours before harvest on day 6 to measure proliferation.
Statisticalanalysis
A Student t test was used to determine statistical significance.
Results
Effect of immobilized Deltaext-myc on the differentiation of monocytes into macrophages and dendritic cells
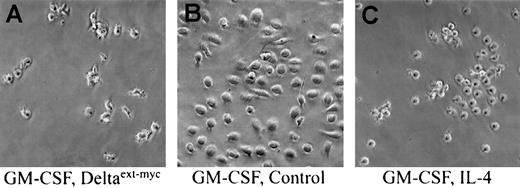
To determine the effect of immobilized Deltaext-myc on macrophage or dendritic cell differentiation, we cultured monocytes with GM-CSF or GM-CSF and IL-4, respectively. As expected, monocytes cultured for 6 days with GM-CSF and control medium were round, large macrophage-appearing cells and were firmly adherent to the plastic (Figure 1B). However, monocytes cultured for 6 days with GM-CSF and Deltaext-myc had an irregular surface with variable numbers of projections and were easily detached from the culture plate (Figure 1A). These characteristics were similar to immature dendritic cells derived from monocytes cultured with GM-CSF and IL-4 (Figure 1C). Mean numbers of cells derived from 10 000 monocytes cultured in quadruplicate in cultures containing GM-CSF and Deltaext-myc were not significantly different from those of cultures containing GM-CSF and control medium (5856 ± 1826 versus 5317 ± 2556; P > .05).
Effect of immobilized Deltaext-myc on differentiation of monocytes cultured with GM-CSF.
Phase contrast microscopy of cells derived from monocytes cultured for 6 days with GM-CSF and 1 μg/mL Deltaext-myc (A), GM-CSF and control medium (B), or GM-CSF and IL-4 (C). Tissue culture wells were coated with anti-myc antibody, 9E10 F(ab′)2, to attach myc-containing Deltaext-myc to the plastic surface (original magnification × 200).
Effect of immobilized Deltaext-myc on differentiation of monocytes cultured with GM-CSF.
Phase contrast microscopy of cells derived from monocytes cultured for 6 days with GM-CSF and 1 μg/mL Deltaext-myc (A), GM-CSF and control medium (B), or GM-CSF and IL-4 (C). Tissue culture wells were coated with anti-myc antibody, 9E10 F(ab′)2, to attach myc-containing Deltaext-myc to the plastic surface (original magnification × 200).
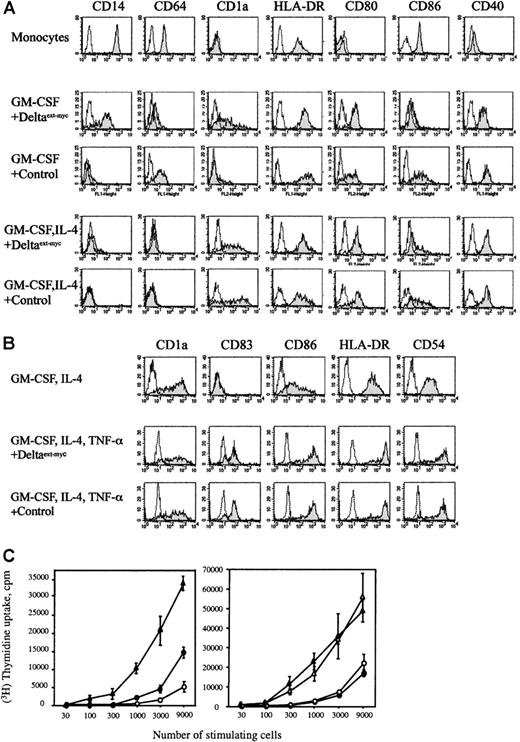
In immunofluorescence studies, cells from cultures containing GM-CSF and control medium expressed low levels of CD1a, diminished levels of CD14 (Leu-M3), and high amounts of CD64, a high-affinity receptor for IgG (FcγR1) (Figure 2A), consistent with the phenotype of macrophages. Conversely, cells cultured with GM-CSF and immobilized Deltaext-myc continued to express CD14 and expressed diminished levels of CD86. However, these cells expressed high levels of CD1a and diminished levels of CD64. We observed that when monocytes were cultured with GM-CSF and IL-4, CD14 expression was detected until day 2, but was no longer detected after that, whereas CD1a was expressed on day 2 (data not shown). These data suggest that the phenotype of cells cultured for 6 days with GM-CSF and immobilized Deltaext-myc is consistent with the early stage of dendritic cells undergoing differentiation from monocytes into immature dendritic cells (Figure 2A).
Effect of immobilized Deltaext-myc on differentiation of monocytes cultured with either GM-CSF or GM-CSF and IL-4 with or without TNF-α.
(A) Fluorescence histograms of peripheral monocytes and cells cultured with GM-CSF or GM-CSF and IL-4 in the presence of 1 μg/mL Deltaext-myc or control medium. Tissue culture wells were coated with anti-myc antibody, 9E10 F(ab′)2, to attach myc-containing Deltaext-myc to the plastic surface. The x-axis represents log fluorescence intensity and the y-axis represents cell number. The shaded histograms represent staining with antibodies against CD14 (Leu-M3), CD64, CD1a, HLA-DR, CD80, CD86, and CD40, and open histograms represent staining with an isotype-matched control antibody of irrelevant specificity. Data are representative of 5 experiments. (B) Effect of Deltaext-myc on TNF-α–induced maturation of immature dendritic cells. Immature dendritic cells derived from monocytes cultured for 5 days with GM-CSF and IL-4 (top panel). Cells were then incubated with GM-CSF, IL-4, TNF-α, and either 1 μg/mL Deltaext-myc or control medium for 2 days (bottom 2 panels). Tissue culture wells were coated with anti-myc antibody, 9E10 F(ab′)2. The shaded histograms represent staining with designated antibodies and open histograms represent staining with an isotype-matched control antibody. One representative experiment of 3 is shown. (C) MLR-stimulatory capacity of cultured cells. In left panel, stimulator cells were prepared from monocytes cultured for 6 days with GM-CSF and 1 μg/mL Deltaext-myc(●), GM-CSF and control medium (○), or GM-CSF and IL-4 (▴). In the right panel, stimulator cells were prepared from monocytes cultured for 7 days with GM-CSF and IL-4 in the presence of 1 μg/mL Deltaext-myc (●) or control medium (○), or from monocyte-derived immature dendritic cells cultured for 2 days with GM-CSF, IL-4, and TNF-α in the presence of 1 μg/mL Deltaext-myc (▴) or control medium (▵). All wells were coated with anti-myc antibody, 9E10 F(ab′)2. After irradiation, increasing numbers of stimulator cells were cocultured with PBMC (5 × 104) for 5 days, and3H-thymidine uptake was assessed. Values are the mean ± SD obtained from triplicate cultures. Data are representative of 3 experiments.
Effect of immobilized Deltaext-myc on differentiation of monocytes cultured with either GM-CSF or GM-CSF and IL-4 with or without TNF-α.
(A) Fluorescence histograms of peripheral monocytes and cells cultured with GM-CSF or GM-CSF and IL-4 in the presence of 1 μg/mL Deltaext-myc or control medium. Tissue culture wells were coated with anti-myc antibody, 9E10 F(ab′)2, to attach myc-containing Deltaext-myc to the plastic surface. The x-axis represents log fluorescence intensity and the y-axis represents cell number. The shaded histograms represent staining with antibodies against CD14 (Leu-M3), CD64, CD1a, HLA-DR, CD80, CD86, and CD40, and open histograms represent staining with an isotype-matched control antibody of irrelevant specificity. Data are representative of 5 experiments. (B) Effect of Deltaext-myc on TNF-α–induced maturation of immature dendritic cells. Immature dendritic cells derived from monocytes cultured for 5 days with GM-CSF and IL-4 (top panel). Cells were then incubated with GM-CSF, IL-4, TNF-α, and either 1 μg/mL Deltaext-myc or control medium for 2 days (bottom 2 panels). Tissue culture wells were coated with anti-myc antibody, 9E10 F(ab′)2. The shaded histograms represent staining with designated antibodies and open histograms represent staining with an isotype-matched control antibody. One representative experiment of 3 is shown. (C) MLR-stimulatory capacity of cultured cells. In left panel, stimulator cells were prepared from monocytes cultured for 6 days with GM-CSF and 1 μg/mL Deltaext-myc(●), GM-CSF and control medium (○), or GM-CSF and IL-4 (▴). In the right panel, stimulator cells were prepared from monocytes cultured for 7 days with GM-CSF and IL-4 in the presence of 1 μg/mL Deltaext-myc (●) or control medium (○), or from monocyte-derived immature dendritic cells cultured for 2 days with GM-CSF, IL-4, and TNF-α in the presence of 1 μg/mL Deltaext-myc (▴) or control medium (▵). All wells were coated with anti-myc antibody, 9E10 F(ab′)2. After irradiation, increasing numbers of stimulator cells were cocultured with PBMC (5 × 104) for 5 days, and3H-thymidine uptake was assessed. Values are the mean ± SD obtained from triplicate cultures. Data are representative of 3 experiments.
To determine if cells possessed antigen-presenting capability of dendritic cells, we evaluated their function in stimulating mixed leukocyte reactions (MLR). We found that cells cultured with GM-CSF and Deltaext-myc were significantly more potent in stimulating MLR than cells cultured with GM-CSF and control medium, although this stimulatory capacity was lower than that of immature dendritic cells generated from GM-CSF and IL-4 (Figure 2C). Nonetheless, these data suggest that cells incubated with GM-CSF and Deltaext-mycgained antigen-presenting function. Overall, these results indicate that Notch signaling induced by Deltaext-myc inhibits GM-CSF–induced differentiation of monocytes into mature macrophages, but permits differentiation into cells with characteristics of an early stage of dendritic cell differentiation.
To determine the effect of Notch signaling on dendritic cell differentiation, we cultured 5000 monocytes with GM-CSF and IL-4. There was no significant difference in the cell number (3250 ± 470 versus 3757 ± 948; P > .05) and in the appearance of cells derived from cultures incubated for 7 days with GM-CSF and IL-4 and either Deltaext-myc or control medium. In both cultures, cells had variable numbers of cytoplasmic projections and a veiled appearance (data not shown). Similarly, monocytes in both cultures gave rise to cells that expressed relatively high amounts of CD1a and HLA-DR, intermediate levels of CD80, CD40, and CD86, and little to no CD14 (Figure 2A) and CD83 (data not shown). In MLR assays, we found that cells from cultures containing Deltaext-myc possessed similar MLR-stimulating capacity as cells from control cultures (Figure2C). These data suggest that Deltaext-myc has no effect on the differentiation of monocytes into immature dendritic cells.
We further investigated the effect of immobilized Deltaext-myc on TNF-α–induced maturation and activation of immature dendritic cells. Immature dendritic cells, generated from monocytes cultured with GM-CSF and IL-4 for 5 days, were harvested and replated in cultures containing GM-CSF, IL-4, and TNF-α and either Deltaext-myc or control medium for another 2 days. We found that cells in both cultures appeared to be mature dendritic cells with numerous projections by phase contrast microscopy (data not shown), and that a substantial portion of cells in both Deltaext-mycand control-containing cultures expressed CD83, indicative of mature dendritic cells, as well as enhanced levels of CD86, CD54, and HLA-DR (Figure 2B). Cells in both cultures possessed equally enhanced levels of MLR-stimulating capacity (Figure 2C). These data suggest that Deltaext-myc does not affect TNF-α–induced maturation and activation of immature dendritic cells. Taken together, these data suggest that Deltaext-myc impairs the differentiation of monocytes into macrophages, but permits differentiation into immature dendritic cells and subsequent maturation into mature dendritic cells.
Deltaext-myc affects cell fate decisions of CD34+ cell-derived CD1a−CD14+macrophage/dendritic precursors
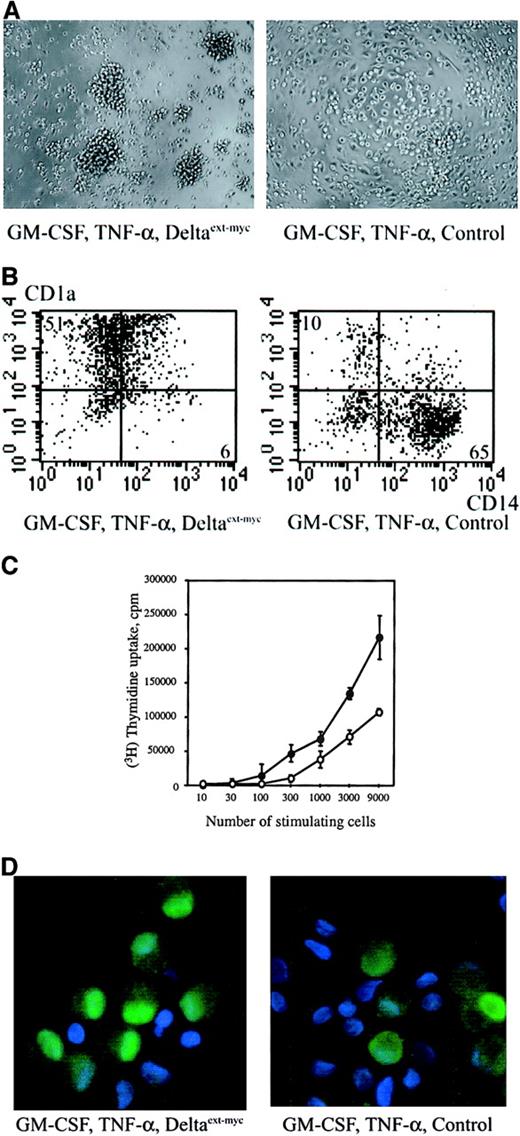
The CD34+ cell-derived CD1a−CD14+ cells are also macrophage/dendritic cell precursors. However, it has been shown that these cells require GM-CSF and TNF-α rather than GM-CSF and IL-4 for differentiation into dendritic cells.27 We therefore determined the effect of Deltaext-myc on the differentiation of these bipotent precursors. We obtained CD1a−CD14+macrophage/dendritic cell precursors by culturing CD34+cells with c-kit ligand, GM-CSF, and TNF-α as described.28 29 After 5 days, cells were harvested; CD1a−CD14+ cells were isolated by flow microfluorometry and then recultured at 2 × 104/well for another 8 days with GM-CSF, TNF-α, and either immobilized Deltaext-myc or control medium.
Phase contrast microscopy revealed that cells from cultures containing Deltaext-myc mainly appeared as dendritic cells with variable numbers of cytoplasmic projections, whereas control cultures contained mainly large-sized, round cells, consistent with the appearance of macrophages, with a small population of dendritic cells (Figure 3A). In the presence of Deltaext-myc, we observed an increase in the population of cells with a CD1a+CD14− dendritic cell phenotype (51% versus 10%), but a decrease in the CD1a−CD14+ macrophage population (6% versus 65%), when compared with control cultures (Figure 3B). Mean numbers of cells in quadruplicate in cultures with GM-CSF, TNF-α, and Deltaext-myc were not significantly different from those of cultures with GM-CSF, TNF-α, and control medium (16 620 ± 7180 versus 16 270 ± 5640; P > .05). Assessment of MLR-stimulating capacity revealed that cells from cultures containing Deltaext-myc had higher MLR-stimulating potential than cells from control cultures (Figure 3C). These data suggest that CD1a−CD14+ macrophage/dendritic cell precursors, on exposure to immobilized Deltaext-myc, adopt a dendritic cell fate rather than a macrophage fate.
Effect of immobilized Deltaext-myc on differentiation of CD34+ cell-derived macrophage/dendritic precursors.
Cells were generated from CD34+ cell-derived CD1a−CD14+ cells cultured for 8 days with GM-CSF, TNF-α, and either 1 μg/mL Deltaext-myc or control medium. All tissue culture wells were coated with anti-myc antibody, 9E10 F(ab′)2, to attach myc-containing Deltaext-myc to the plastic surface. (A) Phase contrast microscopy of cultured cells (original magnification × 100). (B) CD14 and CD1a expression profile of cultured cells. The x-axis represents log fluorescence intensity for CD14 (My4) and the y-axis represents log fluorescence intensity for CD1a. One representative experiment of 4 is shown. (C) MLR-stimulatory capacity of cells from cultures containing 1 μg/mL Deltaext-myc (●) or control medium (○). Values are the mean ± SD obtained from triplicate cultures. One representative experiment of 3 is shown. (D) Cells were stained with anti-RelB antibody (see “Materials and methods”) and nuclei were counterstained with DAPI (original magnification × 40).
Effect of immobilized Deltaext-myc on differentiation of CD34+ cell-derived macrophage/dendritic precursors.
Cells were generated from CD34+ cell-derived CD1a−CD14+ cells cultured for 8 days with GM-CSF, TNF-α, and either 1 μg/mL Deltaext-myc or control medium. All tissue culture wells were coated with anti-myc antibody, 9E10 F(ab′)2, to attach myc-containing Deltaext-myc to the plastic surface. (A) Phase contrast microscopy of cultured cells (original magnification × 100). (B) CD14 and CD1a expression profile of cultured cells. The x-axis represents log fluorescence intensity for CD14 (My4) and the y-axis represents log fluorescence intensity for CD1a. One representative experiment of 4 is shown. (C) MLR-stimulatory capacity of cells from cultures containing 1 μg/mL Deltaext-myc (●) or control medium (○). Values are the mean ± SD obtained from triplicate cultures. One representative experiment of 3 is shown. (D) Cells were stained with anti-RelB antibody (see “Materials and methods”) and nuclei were counterstained with DAPI (original magnification × 40).
To further document dendritic cell differentiation, we examined the expression and location of RelB protein. The nuclear factor κB (NF-κB) family of transcription factors, including RelB and NF-κB1 are activated during dendritic cell differentiation. After activation, these transcription factors translocate from the cytoplasm to the nucleus, bind to target DNA, and then activate a variety of genes.31-33 A significantly higher number of cells from cultures containing Deltaext-myc showed strong nuclear immunostaining for RelB as compared with control cultures (30.3% ± 6.0% versus 6.4% ± 4.7%, mean percentage of 3 different experiments ± SD; Figure 3D). These data further indicate that a higher proportion of CD1a−CD14+ precursors differentiate into mature dendritic cells in the presence of Deltaext-myc, GM-CSF, and TNF-α.
Discussion
We determined the effect of Notch signaling on the cell fate decisions of monocytes, bipotent precursors of macrophages, and dendritic cells. Although it has been possible to define cytokines that enable expression of dendritic cell or macrophage differentiation, cytokines are not thought to instruct assumption of one fate over another.34 We examined the effect of Notch because we had previously found that monocytes express relatively high amounts of Notch-1 and -2 and that activation of Notch signaling by immobilized Deltaext-myc induces apoptosis in monocytes cultured with M-CSF, presumably due to inhibition of macrophage differentiation.26 We also found that immobilized Deltaext-myc induced apoptosis in monocytes cultured with M-CSF, but not with GM-CSF.26 Based on those observations, we therefore determined if, analogous to its role in other bipotent precursors, Notch signaling is inhibitory to macrophage differentiation, but permits or promotes assumption of an alternative cell fate.
To induce Notch signaling, we used immobilized Deltaext-mycbecause we observed that immobilized Deltaext-myc induces apoptosis in monocytes cultured with M-CSF, but not GM-CSF.26 In separate studies, we have also found that Deltaext-myc bound to C2 myoblasts in a Ca++-dependent manner,30 consistent with previous studies showing that Notch and Notch ligand binding is Ca++- dependent.35 In those studies, we further found that Deltaext-myc inhibited C2 myoblast differentiation, indicative of Notch activation.30Conversely, we previously found that Deltaext-myc in solution does not induce apoptosis in monocytes cultured with M-CSF.26 In the present study, we again found no effect of Deltaext-myc in solution on the differentiation of monocytes into macrophages cultured with GM-CSF, even if the concentration was increased up to 10 μg/mL (data not shown). These data are consistent with our previous finding that Deltaext-myc inhibits C2 myoblast differentiation only if immobilized to the plastic via plastic-bound anti-myc antibody.30 However, contradictory studies from other laboratories showed that soluble forms of the extracellular domain of Notch ligands induced normal Notch activation.25 36-39Further studies are required to determine whether the differences result from different cell systems or that small amounts of ligands in solution became immobilized on the unblocked plastic wells in vitro or cell matrix in vivo.
In the present study, we demonstrate that immobilized Deltaext-myc inhibited GM-CSF–induced differentiation of monocytes into macrophages, supporting our previous hypothesis that Notch signaling is inhibitory to macrophage differentiation. In contrast, monocytes cultured with GM-CSF and Deltaext-mycdifferentiated into the early stage of dendritic cells with antigen-presenting properties. Furthermore, Deltaext-myc-exposed monocytes differentiated into CD1a+CD14− immature dendritic cells in the presence of GM-CSF and IL-4, and with addition of TNF-α, further differentiated into mature dendritic cells, characterized by enhanced antigen-presenting capacity and acquisition of CD83. We also found that CD34+ cell-derived CD1a−CD14+macrophage/dendritic cell precursors, on exposure to Deltaext-myc, preferentially differentiate into dendritic cells, rather than macrophages, with GM-CSF and TNF-α. The dendritic cell nature of the cells generated in the presence of Deltaext-myc was further confirmed by the observed increased nuclear translocation of RelB that is known to occur on dendritic cell differentiation. Therefore, these data clearly demonstrate a potential role of Notch signaling for determining cell fate decisions of bipotent macrophage/dendritic cell precursors as observed in other developmental systems.
These studies do not resolve whether Deltaext-myc solely inhibits the differentiation of monocytes to macrophages or whether it also promotes dendritic cell differentiation. In recent studies of neural crest stem cells, Notch signaling irreversibly inhibited neural crest cell differentiation into neural cells and further suggested that Notch signaling promoted their differentiation into glial cells.40 However, an effect of other factors combined with the permissive effects of Notch signaling on glial differentiation could not be ruled out. In our cultures, it is possible that several factors included in serum promote dendritic cell differentiation, while Deltaext-myc selectively inhibits monocyte differentiation into macrophages. Furthermore, we observed that cells from cultures containing GM-CSF and IL-4 in the presence of Deltaext-mycor control medium show the same amounts of MLR-stimulating capacity. These data suggest that Deltaext-myc does not promote the differentiation of monocytes into mature dendritic cells, but rather indicates a permissive effect of Deltaext-myc on dendritic cell differentiation. Consistent with this notion is a lack of effects of Notch-1 deficiency on intrathymic dendritic cell development, despite a profound effect on T-cell development.41
The present studies disclosed a potential role for Notch signaling in regulating cell fate decisions of macrophage/dendritic precursors. Notch signaling has been shown to regulate T-cell versus B-cell lineage decisions.42,43 Moreover, it has recently been reported that some fractions of dendritic cells express another Notch ligand, Jagged-1, and that dendritic cells transfected with Jagged-1 regulate the cell fate choice of CD4+ T cells between regulatory T cell versus helper T cell.44 45 These data further indicate that Notch-mediated cellular interactions may play an important role in regulating immune responses.
The authors thank Jennifer Blasi, Carolyn Brashem-Stein, Steven Staats, David Flowers, and Monica Yu for excellent technical assistance, and Lynn Planet for preparation of the manuscript.
Supported by a National Institutes of Health grant, P50 HL54881. K.O. is a Fellow of the Leukemia Lymphoma Society of America. I.D.B. is supported by the American Cancer Society-F.M. Kirby Clinical Research Professorship.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Irwin D. Bernstein, Fred Hutchinson Cancer Research Center, 1100 Fairview Ave N, D2-373, Seattle, WA 98109; e-mail: ibernste@fhcrc.org.