The core-binding factor (CBF) complex is a heterodimeric transcription factor composed of 2 subunits, CBFα and CBFβ, that play a major role in hematopoiesis. Both members of the CBF complex are frequently altered in acute myeloid leukemia (AML) by translocation, most commonly t(8;21), t(12;21), and t(3;21) for CBFα, located in 21q22, and inv16(p13;q22) for CBFβ, located on 16q22. Recently, a new mechanism of alteration of CBFα, by point mutation, has been reported in myeloid malignancies, particularly in M0 AML. In the present study, we found no point mutation of theCBFβ gene in 30 myelodysplastic syndromes and 100 AMLs, suggesting a limited role, if any, of CBFβ point mutations in those disorders.
Introduction
The core-binding factor (CBF) complex is a heterodimeric transcription factor composed of 2 subunits, α and β. CBFα is encoded by a family of genes with homology to theDrosophila runt gene, which contains an evolutionarily conserved protein motif of 128 amino acids1 that is responsible for DNA binding, transactivation, and heterodimerization with the subunit β.2 Unlike CBFα, the CBFβ subunit does not bind DNA but enhances, by a factor of 10 to 20, the DNA binding of CBFα.3 The CBF complex plays a major role in hematopoiesis4 through regulation of the expression of various genes, including granulocyte–colony-stimulating factor (G-CSF) receptor, macrophage–colony-stimulating factor (M-CSF) receptor, myeloperoxidase, interleukin-3, and T-cell–receptor β gene.4-6 CBFα (AML1), located on 21q22, and CBFβ, located on 16q22, are the 2 genes most frequently deregulated in leukemia, generally through translocations that produce chimeric RNA and protein.7 For the AML1 gene, the major chimeric proteins are AML1-ETO in the t(8;21)(q22;q22) translocation,8 AML1-ETV6 in the t(12;21)(p13;q22) translocations, and, less often, AML1-EVI1, AML1-MDS1, and AML1-EAP in the t(3;21)(q26;q22) translocations.9-11 For theCBFβ gene, only one chimeric protein has been described—CBFβ-MYH11 in inv16(p13;q22) or t(16;16)(p13;q22)—present in almost all patients with the M4 E0 subtype of AML.12 In most of these cases, fusion proteins act to repress transcription of the CBF target genes, which have a promoter consensus sequence for AML1.11,12 In addition, homozygous knockout mice for AML1 or CBFβ have the same phenotype (absence of fetal hematopoiesis).5,6,13 Recently, point mutations of CBFα (AML1) have been reported in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).14-16 In this work, we looked for point mutations of the CBFβ gene that could also potentially inactivate it in AML and MDS.
Study design
Analysis of point mutations of the CBFβ gene was made in 25 healthy subjects (bone marrow donors) and 130 leukemia patients—100 patients with AML (40 patients with M0 AML, 17 patients with M1 AML, 22 patients with M2 AML, 2 patients with M3 AML, 10 patients with M4 AML including 2 patients with M4 E0, and 9 patients with M5 AML according to the French-American-British [FAB] classification17) and 30 patients with MDS (5 refractory anemia, 6 refractory anemia with ring sideroblasts, 7 refractory anemia with excess of blasts, 6 refractory anemia with excess of blasts in transformation, and 6 chronic myelomonocytic leukemia according to FAB classification). A large number of patients with M0 AML were included in this study because a high frequency of AML1 mutations is observed in this type of AML.16 All patients had given informed consent.
Detection of CBFβ gene mutations was made on DNA extracted from bone marrow cells, by single-stranded conformation polymorphism (SSCP) analysis of the 6 exons corresponding to the entire coding region of the CBFβ gene. Primers for polymerase chain reaction (PCR) were chosen upstream and downstream of each exon to include the detection of mutations in acceptor and donor splicing sites. PCR was performed in a total reaction volume of 50 μL containing 50 ng DNA, 0.3 μM each primer (primer names and sequences are given in Table 1), 1 to 3.5 mM MgCl2 (Table1), 10 mM Tris HCl, 50 mM KCl, 200 μM each dNTP (Pharmacia, Stockholm, Sweden), 2.5 U Taq DNA polymerase (Quiagen, Courtaboeuf, France), and 0.037 MBq 32P-labeled deoxycytidine triphosphate. Samples were heated for 5 minutes at 94°C and then underwent 34 cycles for 1 minute at 94°C, 1 minute at 55 to 57°C (Table 1), and 1 minute at 72°C, followed by a final elongation of 7 minutes at 72°C. After amplification, PCR products were loaded on a 2% agarose gel stained with ethidium bromide. The size of the PCR products was 163 to 276 bp (Table 1). For SSCP analysis, 4 μL PCR product was diluted in 16 μL solution containing 0.1% sodium dodecyl sulfate and 20 mM EDTA; 3 μL this mixture was mixed with 3 μL solution of 95% formamide, 20 mM EDTA, 0.05% bromophenol blue, and 0.05% xylene cyanol and then was heated at 95°C for 2 minutes and cooled in ice. Finally, 3 μL was loaded on an MDE gel (Tebu, Le Perray en Yvelines, France). Our preliminary experiments showed the best SCCP profiles were observed with a gel containing 5% glycerol, 1× TBE, and electrophoresis run for 12 hours at room temperature.
Results and discussion
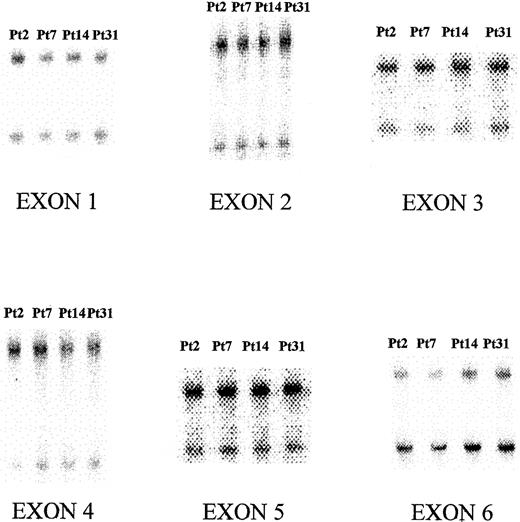
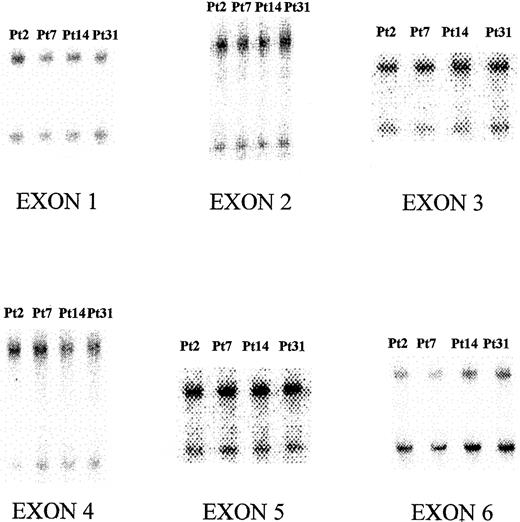
No abnormal SSCP profile for exons 1 to 6 of the CBFβgene was observed in healthy subjects and in 130 patients with MDS and AML studied (Figure 1). These results appear to differ from results observed with the AML1 gene. Indeed, others and we14-16 reported a new mechanism of inactivation of AML1 in hematologic malignancies, through point mutations of the gene in AML and, less frequently, in MDS and myeloproliferative disorders. All mutations of AML1 were located in the runt domain, and most of them were observed in M0 AML or in hematologic malignancies with acquired trisomy 21. In M0 AML, most of the patients had bi-allelic alteration of the AML1 gene either by mutation of the 2 alleles or duplication of the mutated allele with deletion of the wild-type allele or by loss of heterozygosity for AML1. In all patients, point mutations of AML1 gene were acquired, and functional analysis of these abnormal proteins showed that transactivation properties of AML1 on the promoter of the MCSF-receptor gene were abolished. Inactivation of those properties seemed to result from absent binding of the mutated protein on the DNA consensus site of AML1 target genes. In addition, the missense mutations appeared to act in a dominant manner by higher affinity binding of CBF. Therefore, we looked for point mutations of the second partner of the CBF complex, CBFβ, in MDS and AML.
SSCP profile of exons 1 to 6 of the CBFβgene.
Patient 2 was a healthy subject used as negative control. Patients 7, 14, and 31 had, respectively, M0 AML, M1 AML, and RAEB.
SSCP profile of exons 1 to 6 of the CBFβgene.
Patient 2 was a healthy subject used as negative control. Patients 7, 14, and 31 had, respectively, M0 AML, M1 AML, and RAEB.
Our negative results suggest that, unlike AML1, CBFβ is probably not inactivated by point mutations in AML and MDS. Because, except in M0 AML, the number of patients with each FAB subtype was low, we cannot completely exclude a low incidence of mutations in some specific FAB subtypes of AML or MDS. In addition, despite using optimal conditions for SSCP, including small PCR products, we could not exclude the presence of some mutations undetectable by the SSCP technique, which generally is 50% to 100% accurate. The apparent absence of CBFβ mutations in AML and MDS could be linked with the function of the CBFβ protein. Indeed, CBFβ acts as a cofactor, and only bi-allelic mutations or mono-allelic mutations with dominant-negative effects could inactivate the CBF complex, inducing the loss of transactivation of HIS target genes. This kind of alteration of CBFβ could have drastic effects and induce cell death. In that context, mutations with a dominant-negative effect could lead to a phenotype closed to that of CBFβ KO−/− mice with an absence of fetal hematopoiesis. On the other hand, mutations inducing lack of the transcription of only 1 of 2 alleles could lead to a phenotype close to that of KO+/− CBFβ heterozygous mice, which have few abnormalities. In conclusion, unlike AML1 mutations, CBFβ mutations are probably not an important event in the pathogenesis of AML or MDS.
We thank P. Liu for giving us the intronic sequence of theCBFβ gene, and we thank B. Vaast, M. Crepin, C. Denis, and the Institut Fédératif de recherché no. 22 for their excellent technical assistance and support in molecular biology.
Supported by the Centre Hospitalier Universitaire of Lille (PHRC 1997), the Ligue Nationale contre le cancer (Comité du Nord et de l'Aisne), and the Fondation de France (Comité Leucémie).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Claude Preudhomme, Unité 524 INSERM, Institut de Recherche sur le Cancer de Lille, 1 place de Verdun, 59045 Lille Cedex, France; e-mail:cpreudhomme@chru-lille.fr.