Abstract
Adoptive transfer of autologous preinfection-collected peripheral blood mononuclear cells (PBMCs) or activated CD4+ T cells was performed in simian immunodeficiency virus (SIVmac239)–infected monkeys following short-term antiviral therapy with PMPA (9-R-[2-phosphonylmethoxypropyl] adenine). Short-term chemotherapy alone led to a transient decrease in plasma and cellular proviral DNA loads and transient rescue of gag/pol and env cytotoxic T-lymphocyte precursors (pCTLs). However, cessation of therapy allowed for SIV infection to resume its clinical course. PMPA chemotherapy coupled with infusions of either autologous pre-SIV infection–collected PBMCs or activated CD4+ T cells led to extended control of plasma and cellular proviral DNA loads after infusion, in spite of the fact that the transfused cells were not primed against SIV. However, qualitatively different antiviral defenses were induced by infusion of unfractionated and unmanipulated PBMCs versus purified and activated CD4+ T cells: PBMC infusions significantly favored development of SIVenv-specific pCTLs, neutralizing antibodies, and secretion of soluble noncytotoxic suppressor factors of SIV replication. In contrast, activated CD4+ T cells predominantly promoted CTL responses to SIVgag/pol and SIVenv. In addition, infusion of influenza-primed activated CD4+ T cells markedly enhanced influenza-specific pCTL responses, whereas infusion of similarly influenza-primed unfractionated PBMCs enhanced such pCTL responses only modestly, suggesting that the predominant immune defect after SIV infection lies in the T helper cell compartment rather than the effector cell compartment. Thus, adoptive immunotherapy with autologous “SIV naı̈ve” CD4+ lymphocytes was sufficient to rescue cell-mediated immune responses and induce long-term anti-SIV control and immune responses in the absence of continued antiviral chemotherapy.
Introduction
Although highly active antiretroviral therapy (HAART) has a major beneficial effect on HIV-1–infected individuals,1,2 it is clear that the next major therapeutic breakthrough requires a better definition of strategies for full immune reconstitution.3 One of the challenges in achieving this goal is our lack of understanding of the precise spectrum or kinetics of the development of immune dysfunction in individual HIV-infected patients and strategies best suited to reconstitute such immune defects. Although virus-specific cytotoxic T lymphocytes (CTLs) clearly play a major role in eliminating virus-infected cells,4-6 development and maintenance of such CTL pools require CD4+ T helper cell function and an appropriate balance of cytokines.3,7,8 It is also clear that innate immune mechanisms play a major role particularly during the initial stages of infection,9,10 influencing the viral load set point, and that virus-neutralizing antibodies contribute to the containment of cell-free virus infection of naive cells.11 12 Thus, a variety of immune reconstitution strategies need to be explored, some of which may be of benefit to those patients who were initiated on HAART during acute infection, whereas others may be more appropriate to patients with chronic infection. Since the primary target of HIV-1 infection is the CD4+ T cells and the depletion of those cells is one of the major consequences of infection, our laboratory has initially focused on seeking methodologies for the replenishment of this cell lineage.
Several studies aimed at immune reconstitution have previously been performed utilizing autologous unfractionated and in vitro expanded CD8+ T cells from HIV-1–infected patients.13-15 Transient decreases in viral load and increases in CD4+ T-cell counts have been achieved utilizing such immune reconstitution therapies. However, these studies used autologous cells collected after HIV infection. Thus, lack of a more profound effect could be due to either an abnormal microenvironment for the adoptively transferred cells to home, survive, and/or execute immune function, or an intrinsic defect in the transferred T cells, as a direct and/or indirect effect of the virus infection. Clearly, a number of defects ranging from loss of lymphocyte specificities and subsets to signaling defects of CD4+ T cells from HIV-1–infected patients have been documented.16-20 Yet definitive proof for such defects cannot be obtained from the study of humans infected with HIV-1, since it would involve the use of autologous cells obtained prior to infection. Hence, such mechanistic questions require the use of an animal model, which provides infection-induced immune dysfunction within an immune system comparable to humans. Simian immunodeficiency virus (SIV)–infected nonhuman primates provide such a model, in which we may attempt to distinguish among the above-mentioned 2 possibilities since the CD4+ T cells can be collected prior to infection, expanded with anti-CD3/CD28 immobilized antibodies and cryopreserved. In the present study, monkeys were first immunized with live attenuated influenza A/PR8 prior to collecting peripheral blood mononuclear cells (PBMCs), then infected with SIV and infused with autologous preinfection cell lineages and the immune reconstitution potential of the infused cells evaluated.
Materials and methods
Animals
A total of 12 adult healthy rhesus macaques weighing 5 kg to 12 kg comprised this study. The monkeys were housed at the Yerkes Regional Primate Research Center in accordance with the instructions of the Committee on the Care and Use of Laboratory Animals of the Institute of Laboratory Animal Resources, National Research Council and the U.S. Public Health Service Guidelines, Guide for the Care and Use of Laboratory Animals.
Experimental protocol
All macaques were immunized with 1024 HA (hemagglutination) units of live attenuated influenza virus A/PR8 intranasally and boosted with the same dose and route 6 weeks later. Starting one month later, the monkeys were bled every 2 weeks with rapid leukocyte collection and reinfusion of erythrocytes to maximize leukocyte collections until the desired number of lymphoid cells were obtained. PBMCs were then either cryopreserved or subjected to CD4+T-cell isolation and expansion as outlined below. During this period, one monkey was euthanized because of wasting. The remaining 11 monkeys were then infected with 200 tissue culture infection dose 50 (TCID50) of SIVmac239 intravenously and followed for levels of plasma viremia. Group 1 (n = 2) served as virus infection control group. At 13 weeks after infection, upon achievement of plasma viral load set point, 9 monkeys were treated daily with 30 mg/kg of PMPA (9-R-[2-phosphonylmethoxypropyl] adenine) subcutaneously for 28 days. The 9 monkeys were split into 3 groups of 3 animals each. Group 2 served as virus-infected PMPA controls. Group 3, starting 1 week prior to cessation of PMPA therapy, received 2.5 × 108autologous viable unfractionated (pre SIV) PBMCs intravenously weekly for 6 weeks (total 1.5 × 109). Group 4 received autologous anti-CD3/CD28 stimulated and expanded (pre SIV) CD4+ T cells (2.5 × 108/infusion) according to the same schedule as group 3. Lymph node biopsies were performed at 10 weeks after infection (before PMPA), 27 weeks after infection (following PMPA/transfusions) and 60 weeks after infection or at autopsy.
Preparation of cells for infusion
PBMCs were isolated by standard Ficoll-hypaque gradient centrifugation. For group 3 monkeys, a total of 2 × 109unfractionated PBMCs per monkey were cryopreserved. For group 4 monkeys, CD4+ T cells were first selected using anti-CD4–conjugated magnetic beads (Dynal, Lake Success, NY) and then rescued using the “Detachabead” reagent. The enriched CD4+ T cells (> 95% CD4+), were then cultured in vitro with tosyl-activated magnetic beads (Dynal) coated with equal amounts of anti-CD3 (clone FN18) and anti-CD28 monoclonal antibodies according to the manufacturer's instruction at a 3:1 bead-to-cell ratio. Cells were cultured/expanded for 3 to 4 weeks in RPMI 1640 with 10% fetal calf serum, adding more antibody-coated immunobeads as required. At the end of culture the beads were removed and the cells washed and cryopreserved. Aliquots of each batch were analyzed for purity by FACS (> 90% CD4+ and < 5% CD8+) and tested for endotoxin content and sterility. On the day of infusion, the required number of cryopreserved unfractionated PBMCs or anti-CD3/CD28 activated and expanded CD4+ T cells was thawed, washed twice in RPMI 1640 media, resuspended at 2.5 × 108 viable cells in 10 mL sterile phosphate-buffered saline (PBS), and infused intravenously into autologous monkeys. Each monkey received one infusion per week for 6 weeks.
Viral load determinations
Plasma viral loads were performed using a competitive reverse transcriptase–polymerase chain reaction (RT-PCR) assay as described previously.18 The sensitivity of the plasma viral RNA detection utilizing this technique was determined to be 500 copies/mL plasma.
Proviral DNA load determinations were performed on DNA samples from sequentially collected PBMCs or lymph node cells (LNCs). The technique to quantitate proviral DNA has been described previously.18 The sensitivity of the assay was previously determined to be one copy per 1 × 105 cells. Results are expressed as the number of DNA copies per 105cells.
SIV serology
Plasma samples were assayed for anti-SIV antibodies utilizing routine enzyme-linked immunosorbent assay (ELISA) techniques, whereas SIVmac239-specific neutralizing antibody titers were determined as described by Montefiori et al.21
Determination of SIV and influenza-specific CTL precursors
Sequential PBMC aliquots were assayed for the presence and frequencies of SIVgag/pol-, SIVenv-, and influenza matrix protein (Flu-MP)–specific CTL activity in a classic limiting dilution assay described previously.22,23 The frequencies of CTL precursors and confidence intervals were derived using the Jacknife program.48 Data presented represent net pCTL values, where the values for SIVgag/pol, SIVenv, or Flu-MP have been adjusted for the values obtained against targets pulsed with wild-type Vaccinia virus by the same responder population.
Evaluation of CD8-secreted antiviral mediators
Secretion of soluble antiviral activity was evaluated on sequential PBMC cultures from the animals using a double chamber assay.24 25 Briefly, PBMCs were stimulated with 2 μg/mL phytohemaglutinin (PHA; Difco Laboratories, Detroit, MI) for 3 days before being added to the top chamber of a Transwell culture system (Costar, Corning, NY) containing CD4+ PBMCs from a naı̈ve donor freshly infected with SIVmac239 (multiplicity of infection [MOI], 0.1) in vitro. All cultures were set up in duplicates as a single experiment to avoid interassay variability. Culture supernatants collected at day 5, day 10, day 15, day 20, and day 25 were analyzed for p27 content. Control cultures contained PHA-stimulated PBMCs from SIV-naı̈ve monkeys or no cells in the top chamber.
Results
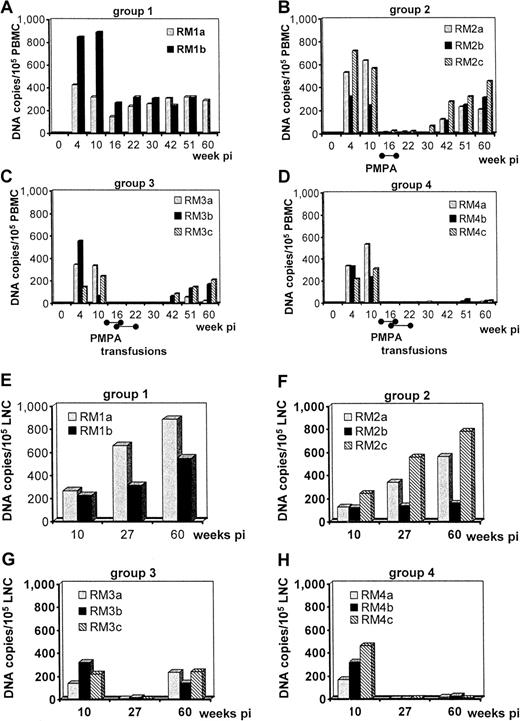
Effect of autologous cell transfusions on plasma viral load
In efforts to determine the potential therapeutic benefit of autologous lymphoid cell transfusion without the confounding effect of lentivirus infection–mediated immune defect in the transfused cells, the monkeys were infected and allowed to seroconvert and establish their respective viral load set point before initiating treatment. To prevent loss or impairment of infused naı̈ve cells as potential viral targets, viral loads were first reduced to a minimum using a short-term course of the antiviral drug PMPA.26Thereafter, cell transfusions were initiated 1 week prior to cessation of PMPA therapy and continued weekly for 6 weeks.
During the studies, one of the SIV-infected control monkeys (group 1) died of simian AIDS at week 51 after infection, and 2 of 3 virus-infected and PMPA-treated animals (group 2) died at week 62 after infection. In contrast, all monkeys that received autologous unfractionated PBMCs (group 3) or autologous anti-CD3/CD28-activated and -expanded CD4+ T cells (group 4) survived more than 64 weeks after infection. As seen in Figure1A-D, all 11 monkeys showed plasma viremia prior to initiation of PMPA therapy, although the levels did vary. One group 1 monkey, 1 monkey of 3 group 2 monkeys, and 2 monkeys of 3 monkeys in group 3 and group 4 had levels of plasma viremia significantly higher than the other animals within their respective groups. After reaching viral load set point by 6 weeks after infection, both animals in the virus control group maintained approximately the same level of viral load until weeks 22 to 24. After this point, the monkey RM1b continued to show increased viral load, developed AIDS, and was euthanized at week 51. All 3 group 2 animals reached viral plasma load set point by 6 to 8 weeks and following PMPA therapy showed undetectable levels (< 500 copies/mL) of viremia until approximately week 22. Thus, cessation of PMPA therapy provided approximately 7 to 10 weeks of viral replication control. In marked contrast, PMPA therapy followed by autologous unfractionated PBMCs or anti-CD3/CD28-activated autologous CD4+ T-cell infusions led to a marked decrease in plasma viral load in 2 of 3 group 3 animals and all 3 group 4 animals, respectively, for at least 64 weeks after infection, 48 weeks after PMPA therapy. However, the levels of control of viral replication were not uniform. Thus, soon after cessation of PMPA therapy, all group 3 and group 4 animals showed low levels of viral replication (2000 vRNA copies/mL at 18-20 weeks after infection). Following this period of moderate replication, one group 3 animal (RM3c) showed a full viral rebound, reflecting a potential for higher viral replication and susceptibility to disease progression, since this animal showed increasing viral loads prior to PMPA therapy (Figure 1C). In addition, within this group, monkey RM3b showed an initial increase in plasma viral load followed by 10 to 14 weeks of undetectable levels and renewed low but clearly positive viremia by weeks 42 to 60. In contrast, the virus in 2 of 3 monkeys from group 4 was undetectable for 5 months (RM4c) or more than 10 months (RM4b) from week 20 after infection (Figure 1D). The third monkey in this group behaved much like monkey RM3b in group 3, in which viral control was preceded by an initial increase in plasma viral loads up to 6 weeks after discontinuation of PMPA treatment. Two of 3 group 4 monkeys exhibited detectable low viral loads again at 42 weeks after infection, but in contrast to group 3 viremic monkeys, these loads showed a decreasing trend toward week 60 when the study was terminated.
Plasma viral load in rhesus macaques following SIVmac239 infection.
(A) Virus-only control group (monkeys RM1a and RM1b). (B) SIV infection and a 28-day course of PMPA chemotherapy (monkeys RM2a, RM2b, RM2c). (C) SIV infection, PMPA chemotherapy, and infusion with autologous unfractionated PBMCs (monkeys RM3a, RM3b, RM3c). (D) SIV infection, PMPA chemotherapy, and infusion with anti-CD3/CD28-activated autologous CD4+ T cells (monkeys RM4a, RM4b, RM4c).
Plasma viral load in rhesus macaques following SIVmac239 infection.
(A) Virus-only control group (monkeys RM1a and RM1b). (B) SIV infection and a 28-day course of PMPA chemotherapy (monkeys RM2a, RM2b, RM2c). (C) SIV infection, PMPA chemotherapy, and infusion with autologous unfractionated PBMCs (monkeys RM3a, RM3b, RM3c). (D) SIV infection, PMPA chemotherapy, and infusion with anti-CD3/CD28-activated autologous CD4+ T cells (monkeys RM4a, RM4b, RM4c).
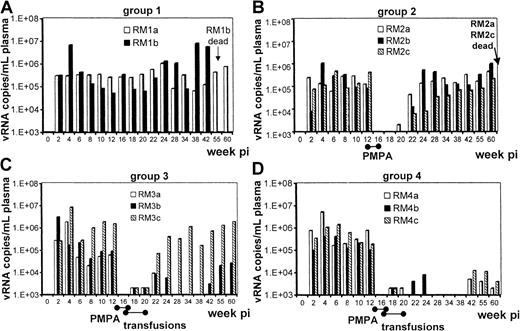
Effect of autologous cell transfusions on proviral DNA levels
PBMC and LNC samples from all 11 animals were subjected to proviral DNA load analysis and each showed a significant amount of PBMC-associated proviral DNA by 4 weeks after infection, ranging from 148 to 850 copies per 105 cells (Figure2A-D). In both virus control infection monkeys, the high initial frequency of proviral DNA-containing cells decreased to a steady state by 16 weeks after infection (Figure 2A). The virus-infected and PMPA-treated animals (groups 2, 3, and 4) all showed a rapid decrease of PBMC proviral DNA by week 16. However, whereas all 3 group 2 animals showed a rebound of PBMC proviral DNA by week 42 (Figure 2B), there was significantly less PBMC proviral DNA in the monkeys that received cell infusions (groups 3 and 4,P < .02). The proviral DNA decrease appeared better sustained in the monkeys that received autologous anti-CD3/CD28-activated and -expanded CD4+ T cells (Figure2D; < 24 copies per 105 PBMCs) than the monkeys that received unfractionated PBMCs (Figure 2C).
Cellular proviral load in PBMCs or LNCs of rhesus macaques following SIVmac239 infection.
(A,E) Virus-only control group. (B,F) SIV infection and a 28-day course of PMPA chemotherapy. (C,G) SIV infection, PMPA chemotherapy, and infusion with autologous unfractionated PBMCs. (D,H) SIV infection, PMPA chemotherapy, and infusion with anti-CD3/CD28-activated autologous CD4+ T cells. PBMCs, A-D; LNCs, E-H.
Cellular proviral load in PBMCs or LNCs of rhesus macaques following SIVmac239 infection.
(A,E) Virus-only control group. (B,F) SIV infection and a 28-day course of PMPA chemotherapy. (C,G) SIV infection, PMPA chemotherapy, and infusion with autologous unfractionated PBMCs. (D,H) SIV infection, PMPA chemotherapy, and infusion with anti-CD3/CD28-activated autologous CD4+ T cells. PBMCs, A-D; LNCs, E-H.
LNCs isolated from biopsies obtained at 10 weeks after infection also showed significant cellular proviral DNA loads following SIV infection and before PMPA therapy (Figure 2E-H). However, whereas LNC samples from control group 1 and group 2 monkeys showed high cellular proviral DNA loads at week 27 after infection (401 ± 187 viral copies/105 cells), LNCs from the monkeys that received cell infusions following PMPA therapy (groups 3 and 4) showed a marked decrease in cellular proviral DNA loads (range, 0 to 16 viral copies/105 cells). Moreover, at later stages (51-62 weeks after infection), whereas LNCs from group 1 and group 2 animals all continued to show high cellular proviral DNA loads and LNCs from the group 3 animals appeared to show initial evidence of viral rebound (Figure 2G; 144, 234, and 238 viral copies/105 cells), LNCs from the 3 group 4 animals still maintained low cellular proviral DNA loads (Figure 2H; 8, 16, and 24 viral copies/105 LNCs), suggesting a more sustained antiviral control in group 4 monkeys. Thus, infusion of SIV antigen-naı̈ve PBMCs, and particularly activated CD4+ T cells, can induce a sustained inhibition of viral replication.
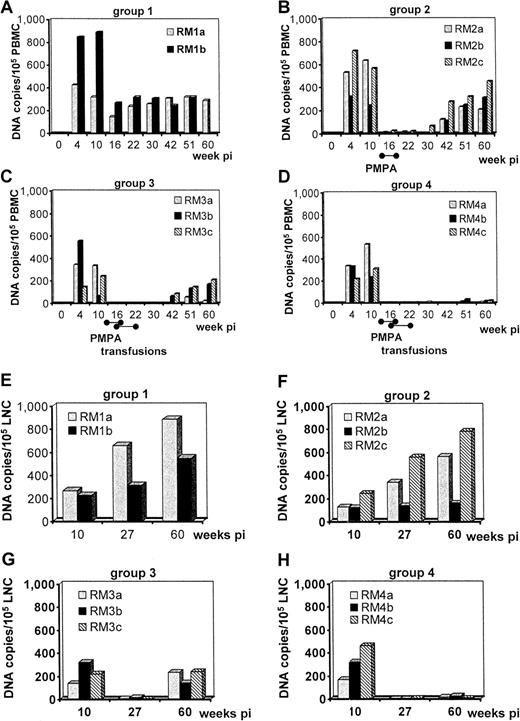
Effect of autologous cell transfusions on CD4+ and CD8+ T cells
As seen in Figure 3A,C,E,G, the frequency of CD4+ T cells in most of the 11 monkeys following SIV infection decreased by 8 weeks after infection. Subsequently, there was a gradual continuing decline in the frequency of CD4+ T cells in group 1 and group 2 monkeys. In group 3 animals, 2 of 3 showed an increase in the frequency of CD4+and CD8+ T cells coinciding with PMPA therapy and transfusion with the unfractionated PBMCs. The animals in group 4 maintained a relatively stable CD4+ and CD8+T-cell frequency. Absolute values and frequencies of CD4 and CD8 cells expressing CD25 and CD69 did not appear to be informative (data not shown). In general, monkeys that received autologous cell infusions maintained higher frequencies of CD4+ T cells, however, lack of CD4+ T-cell loss is not a reliable marker for absence of disease progression in rhesus macaques infected with SIVmac isolates.27 28
Kinetics of the frequencies of CD4+ and CD8+T-cell subsets in the PBMCs of rhesus macaques following SIVmac239 infection.
SIV infection alone (A,B); SIV infection and a 28-day course of PMPA chemotherapy (C,D); SIV infection, PMPA chemotherapy, and infusions with autologous unfractionated PBMCs (E,F); SIV infection, PMPA chemotherapy, and infusions with anti-CD3/CD28-activated autologous CD4+ T cells (G,H). CD4+, A,C,E,G; CD8+, B,D,F,H.
Kinetics of the frequencies of CD4+ and CD8+T-cell subsets in the PBMCs of rhesus macaques following SIVmac239 infection.
SIV infection alone (A,B); SIV infection and a 28-day course of PMPA chemotherapy (C,D); SIV infection, PMPA chemotherapy, and infusions with autologous unfractionated PBMCs (E,F); SIV infection, PMPA chemotherapy, and infusions with anti-CD3/CD28-activated autologous CD4+ T cells (G,H). CD4+, A,C,E,G; CD8+, B,D,F,H.
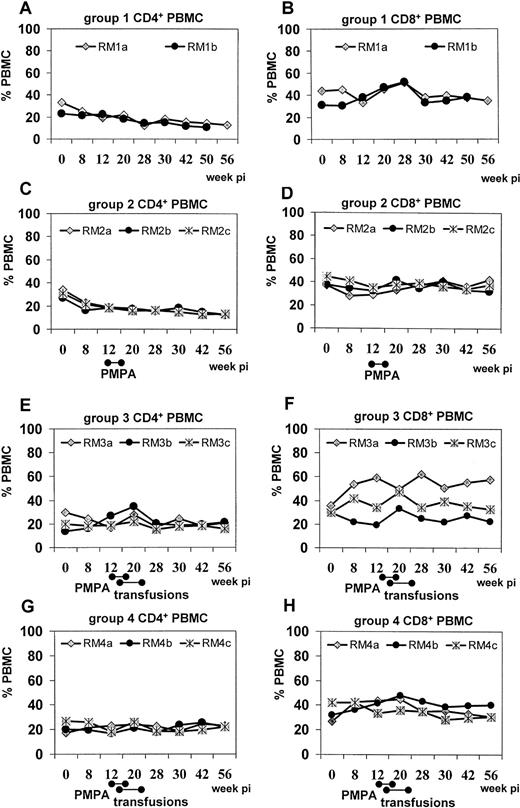
Effect of autologous cell transfusions on SIV-specific pCTLs
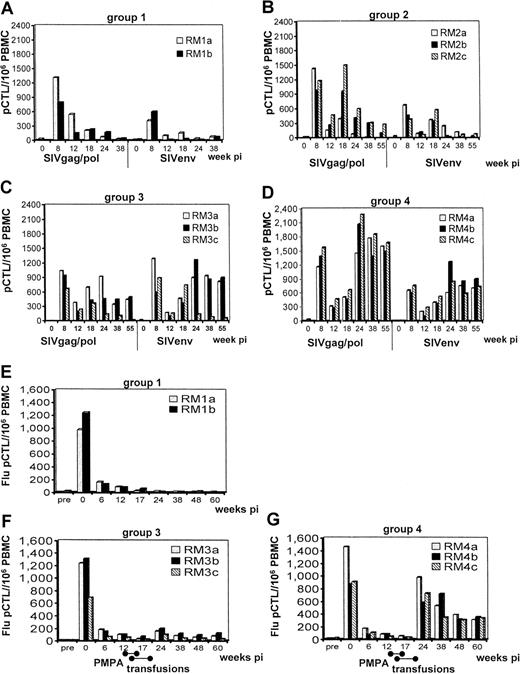
SIVgag/pol- and SIVenv-specific pCTL frequencies were determined from all monkeys (1) prior to SIV infection, (2) at the viral load set point but prior to PMPA therapy (weeks 8 and 12), (3) following PMPA therapy/before completion of cell infusions (week 18), and (4) following cell infusions (weeks 24, 38, and 55) (Figure4). CTL precursors against SIVgag/pol and SIVenv were initially noted in all monkeys at viral load set point (week 8), as were decreases of such values by week 12, just prior to PMPA therapy. The pCTL trends then diverged: in group 1 untreated control monkeys, pCTLs remained low or decreased to undetectable levels (Figure 4A). In contrast, in group 2 animals, PMPA (weeks 13-17 after infection) induced marked rescue of pCTLs at 18 weeks after infection for SIVgag/pol and SIVenv, suggesting that the antiviral chemotherapy itself does benefit cell-mediated responses (Figure 4B). However, these enhanced responses were transient since pCTL frequencies decreased to pre-PMPA levels at 24 weeks after infection and even further thereafter. Group 3 was heterogeneous: PBMCs from RM3c showed pCTL frequencies indistinguishable from group 2 animals at week 18 (Figure4C), but thereafter, this animal (unlike his group mates) showed a gradual decrease of SIVgag/pol and SIVenv pCTL values, which correlated with the high plasma viral load rebound in this animal. The other 2 monkeys (RM3a and RM3b) not only showed “rescue” of pCTLs following PMPA treatment and PBMC transfusion, but these frequencies were maintained over time, correlating with significant containment of virus replication. Enhancement of pCTL frequencies was more marked against SIVenv than SIVgag/pol determinants in this group. In contrast, group 4 animals showed enhancement and maintenance of not only SIVenv-specific pCTL frequencies, but in addition, a striking enhancement and maintenance of SIVgag/pol pCTLs (Figure 4D). These data suggest that infusions with autologous activated CD4+ T cells (2.5 × 108/infusion ×6) provide a qualitatively different immune reconstituting/augmenting effect than similar numbers of autologous unfractionated and unmanipulated PBMCs. These data also suggest that providing new T helper cells was sufficient to markedly rescue and enhance CD8+ effector functions following SIV infection even though these infused helper cells were not SIV specific.
SIVenv- and SIVgag/pol-specific CD8+ pCTL frequencies in PBMC samples from rhesus macaques following SIVmac239 infection.
SIV infection alone (A); SIV infection and a 28-day course of PMPA chemotherapy (B); SIV infection, PMPA chemotherapy, and infusions with autologous unfractionated PBMCs (C); SIV infection, PMPA chemotherapy, and infusions with anti-CD3/CD28-stimulated and -expanded autologous CD4+ T cells (D). Sequential Flu-MP–specific CD8+ pCTL frequencies in PBMC samples following SIVmac239 infection alone (E); SIV infection, PMPA chemotherapy, and infusions with autologous unfractionated PBMCs (F); SIV infection, PMPA chemotherapy, and infusions with anti-CD3/CD28-stimulated and -expanded autologous CD4+ T cells (G).
SIVenv- and SIVgag/pol-specific CD8+ pCTL frequencies in PBMC samples from rhesus macaques following SIVmac239 infection.
SIV infection alone (A); SIV infection and a 28-day course of PMPA chemotherapy (B); SIV infection, PMPA chemotherapy, and infusions with autologous unfractionated PBMCs (C); SIV infection, PMPA chemotherapy, and infusions with anti-CD3/CD28-stimulated and -expanded autologous CD4+ T cells (D). Sequential Flu-MP–specific CD8+ pCTL frequencies in PBMC samples following SIVmac239 infection alone (E); SIV infection, PMPA chemotherapy, and infusions with autologous unfractionated PBMCs (F); SIV infection, PMPA chemotherapy, and infusions with anti-CD3/CD28-stimulated and -expanded autologous CD4+ T cells (G).
Effect of autologous cell transfusions on Flu virus–specific pCTLs
Our laboratory has previously shown that Flu virus–primed monkeys rapidly lose Flu-MP CTL activity after SIV infection.29Since the infused PBMCs and activated CD4+ T cells were collected following Flu immunization and thus included Flu primed cells, it was reasoned that adoptive transfer of such Flu-specific memory T cells was likely to restore Flu-specific responses in vivo. As seen in Figure 4E-G, each of the monkeys showed significant Flu-MP–specific pCTL responses prior to SIV infection, which were markedly decreased upon SIV infection. However, whereas infusions of the group 3 monkeys with autologous unfractionated Flu-primed PBMCs led to only a modest but significant increase (3- to 4-fold increase in Flu-MP–specific pCTL/106 PBMCs; Figure 4F;P < .02), infusions with autologous activated CD4+ T cells in the group 4 monkeys led to a robust enhancement of Flu-MP–specific pCTL frequencies (Figure 4G,P < .01). However, the CTL activity was mediated by CD8+ T cells and major histocompatibility complex (MHC) class I restricted as determined by CD8 depletion or addition of anti-MHC class I antisera (data not shown). In addition, the differences in the Flu-MP–specific pCTL values seen in the PBMCs of group 3 and group 4 monkeys were highly significant from week 24 after infection until the end of the study (P < .02). Since the presence of influenza antigen at the time of cell transfusion was highly unlikely, it is assumed that such SIV-infected animals retained Flu-specific memory CD8+ T cells in vivo which were reactivated via infusions with Flu-MP memory-containing activated CD4+ T cells better than with unfractionated PBMCs, suggesting again that the predominant immune impairment at this stage of infection resides in the CD4+ T-cell compartment.
Effect of autologous cell transfusions on secretion of soluble inhibitors of SIV
Analyses of sequential PBMC samples for production and release of soluble inhibitor activity were performed against a single batch of SIVmac239-infected rhesus target cells using Transwell cultures to separate effectors and targets. Listed in Table1 are mean p27 values (and percent inhibition) obtained from duplicate cultures at day 10 for an effector-to-target ratio of 1:1. Effector cells collected from all monkeys prior to SIV infection showed 8.5% to 19.4% inhibition of viral replication most likely secondary to antigen nonspecific production of β-chemokines.30 Shortly after SIV infection however, marked levels of inhibition of SIV replication ranging between 65% to 76% were observed in all animals. Similar to previously published data,30 the production of such soluble antiviral mediators was gradually lost in untreated macaques (group 1) during the course of infection. In contrast, group 4 animals showed long-term maintenance of soluble inhibitor production (P < .005 at week 22 and 42 weeks after infection) at levels similar to those observed early after infection. In further contrast, group 3 animals not only maintained soluble inhibitor production, but this mechanism appeared markedly enhanced when compared with untreated controls (P < .04 at week 22) or even to group 4 animals (P = .06). These enhanced levels of soluble inhibitors were especially evident in monkeys RM3a and RM3b, which exerted marked control of viremia (Figure 1C), whereas in RM3c, soluble inhibitor production decreased over time, concurrent with the observed increases in viral loads. These data clearly suggest that administration of autologous unfractionated SIV-naı̈ve PBMCs is sufficient to induce production of soluble inhibitors and boost this antiviral pathway. Conversely, purified and activated CD4+T cells, while sustaining (or protecting) this effect, do not appear to significantly enhance the production of soluble inhibitors.
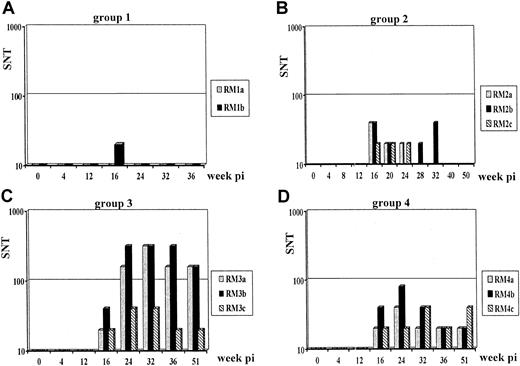
SIV-neutralization antibody titers
Sequential plasma aliquots were analyzed for SIVmac239-neutralizing antibodies, and there were generally undetectable titers in group 1 control monkeys (Figure5A). In contrast, group 2, group 3, and group 4 monkeys all showed detectable titers of neutralizing antibodies after PMPA but before transfusion. Although these titers became undetectable over time in all nontransfused group 2 monkeys (Figure5B), they were marginally enhanced and sustained in group 4 animals (Figure 5C). In marked contrast, group 3 monkeys showed marked enhancement of these titers (Figure 5B,C) suggesting again profound qualitative differences in the immune restoration induced by autologous PBMC transfusion and activated CD4+ T cells. Monkey RM3c again showed relatively lower titers than the other 2 animals in its group, correlating with its increasing viral loads. Since B cells cryopreserve very poorly, the PBMC infusions were not expected to significantly enrich this pool. Thus, it is assumed that the effect noted in Figure 5C,D was most likely secondary to transfusion of T cells, providing improved help to B cells.
Sequential anti-SIVmac239–neutralization antibody titers in rhesus macaques.
Animals were infected with SIV only (A); with SIV followed by a 28-day course of PMPA chemotherapy (B); with SIV, PMPA chemotherapy, and infusions with autologous unfractionated PBMCs (C); with SIV, PMPA chemotherapy, and infusions with anti-CD3/CD28-stimulated and -expanded autologous CD4+ T cells (D).
Sequential anti-SIVmac239–neutralization antibody titers in rhesus macaques.
Animals were infected with SIV only (A); with SIV followed by a 28-day course of PMPA chemotherapy (B); with SIV, PMPA chemotherapy, and infusions with autologous unfractionated PBMCs (C); with SIV, PMPA chemotherapy, and infusions with anti-CD3/CD28-stimulated and -expanded autologous CD4+ T cells (D).
Discussion
Although HAART is extremely effective in decreasing viral loads, immunologic recovery is slow31 and is by itself not sufficient to eradicate the virus or to facilitate immune reconstitution to a level at which chemotherapy is no longer required.3,32,33 Thus, the need for adjunct immunotherapy is clearly warranted. A variety of strategies for such immunotherapy have been attempted, including bone marrow transplantations among human leukocyte antigen (HLA)–matched siblings,34,35cytokine-based immunotherapies, and lymphoid cell infusions,13-15,36-38 all of which have had limited success.3 The cell infusion studies have included use of previously cryopreserved autologous unmanipulated PBMCs13and LNCs,38 in vitro expanded virus-specific autologous CD8+ CTLs,39 in vitro anti-CD3/CD28-activated and -expanded autologous CD4+ T cells,40 and CD4 zeta chain gene-modified autologous CD4+ and CD8+ T cells.41 The in vivo survival and trafficking of the infused cells have also been subjects of intense study.42
The reasons for the modest success of these strategies to date are not clear, but may be due to (1) intrinsic defects in the cells collected after infection, (2) absence of T cells with essential T-cell repertoire specificities, (3) stages of disease in which such therapy has been attempted, or (4) the fact that such patients continue to receive chemotherapy which may prevent the optimal function of the transfused cells and allow for insufficient exposure to antigenic stimuli.
To distinguish among some of these possibilities and in efforts to provide proof of principle whether such transfusion therapy has the potential for sustained clinical benefit, infusions of preinfection-collected autologous lymphoid cells were performed in SIV-infected macaques following short-term antiviral chemotherapy. Our results are the first to establish that despite their “SIV naı̈ve” status, the transfused preinfection lymphocytes were highly effective at promoting/maintaining robust antiviral responses associated with marked containment of viral replication. Surprisingly, reinfusion of autologous influenza-specific memory-containing activated CD4+ T cells appeared far more potent at restoring/enhancing influenza-specific pCTL responses than unmanipulated PBMCs containing both CD4+ and CD8+ T cells specific for influenza. These data clearly underscore the fact that it is the CD4+ T helper cell pool that is impaired at the clinically asymptomatic stage of infection. Thus, providing intact and/or unimpaired “SIV naive” CD4+ T cells to chronically infected monkeys in the presence of low levels of virus/antigen was clearly sufficient to induce or restore antigen-specific cellular effector mechanisms. In addition, providing antigen-specific activated CD4+ T cells was sufficient to not only restore but also enhance such effector mechanisms even in the absence of antigen (Flu).
A number of issues, however, remain to be addressed. These include, but are not limited to (1) whether such a result is unique to the SIV isolate utilized, (2) the precise mechanism that is involved in containing such viral load, (3) the underlying mechanisms by which infusions of autologous unfractionated cells were different from the mechanisms by which infusions with autologous activated CD4+ T cells mediated viral containment, and (4) whether HAART interruption was critical. Finally, further studies will be required to determine whether the stage of disease and timing of the infusions prior to cessation of antiviral drug therapy was critical in obtaining such results. Of importance also is to determine whether such cellular therapies can be conducted on cells collected after SIV infection, which would be of direct relevance to human HIV infection.
With regard to the first issue, SIVmac239 is a predominantly T-cell–tropic molecularly cloned virus which replicates poorly in macrophages. Thus, this type of antiviral containment could be restricted to predominantly lymphotropic viruses and it remains to be established whether this approach is effective for monocytotropic/dual tropic isolates. SIVmac239, while pathogenic, is also relatively less virulent in vivo than its parent biologic clone SIVmac251.43 Thus, relative virulence could also affect the outcome of such cell-based therapies, as suggested by the differing therapeutic outcomes in group 3 monkeys. Based on the increased viral loads prior to PMPA treatment in monkey RM3c, it is possible that this animal showed a higher susceptibility to SIV replication and disease induction, potentially resulting in treatment failure. Although the modest group size precludes conclusions, all group 4 animals infused with activated CD4+ T cells exhibited potent antiviral control, suggesting that the virulence issue may be overcome with optimal reconstitution. Finally, it will be interesting to investigate whether the replicating viral isolates detected late in the infused monkeys represent immune escape mutants; this is the subject of ongoing studies.
As far as potential mechanisms of the induced antiviral containment, one has to bear in mind that the infused cells did not contain any virus-specific memory T cells and thus most likely provided either nonspecific helper T cell responses and/or fresh T-cell clones able to more efficiently recognize potential viral immune escape mutants. Ongoing studies are aimed at determining the respective breadth of SIVgag and SIVenv peptide-specific responses. Our findings regarding the influenza-specific responses provide additional mechanistic insights. Thus, although the adoptive transfer of unfractionated PBMCs containing both antigen-specific CD4+ and CD8+T cells appeared to restore modest levels of cell-mediated responses to this pre-SIV–encountered immunogen, there was a marked enhancement of such responses in the animals that were administered autologous Flu-primed activated CD4+ T cells. In this instance, the antigen is no longer present and thus it is unlikely that new T-cell clones are being activated. Therefore, we interpret this data as enhancement and/or mobilization of CD8+ effectors via the supply of highly effective and activated CD4+ T helper cells. However, it remains to be seen whether the immune restoration noted after adoptive transfer of Flu memory-containing T cells relies on the same mechanisms as the restoration of SIV-specific responses following transfer of SIV-naı̈ve T cells. In addition to these studies, the evolution of TCR Vβ spectratypes was followed in the CD4 and CD8 compartment of these animals. Although skewing of the CD4 compartment was noted in control animals (group 1) the data for the other monkeys showed marked individual variations and overall this analysis appeared inconclusive (data not shown).
We tested 2 forms of adoptive immunotherapy in these studies. Interestingly, while infusions of either unfractionated PBMCs or activated and expanded CD4+ T cells both induced potent antiviral containment in vivo, the effects of these 2 forms of immunotherapy differed: while the PBMC-infused monkeys appeared to generate potent SIVenv pCTLs, soluble antiviral activity, and neutralizing antibody titers, these responses appeared relatively less potent at containing proviral and plasma viral loads over time, not to mention that 1 of 3 monkeys from this group failed to maintain antiviral containment shortly after therapy (correlating with a decrease of antiviral responses). In contrast, the group 4 monkeys transfused with their activated/expanded pre-SIV CD4+ cells exhibited markedly enhanced pCTLs to SIVgag/pol in addition to SIVenv-directed responses; this phenotype is reminiscent of the immune status described in long-term nonprogressor patients with HIV infection.4 Anti-CD3/CD28 immunobead-activated and -expanded CD4+ T cells synthesize substantial amounts of β chemokines MIP-1α, β and RANTES,44 which is tightly regulated by the synthesis of tumor necrosis factor α (TNF-α).45 These cells also demonstrate down-regulation of CCR5 and resistance to infection by SIV and monocytotropic HIV. Even though this resistance to infection is reversible in vitro following removal of the immunobeads,46 these cells may engraft more efficiently,41 maintain the CCR5 virus-resistant phenotype, and/or differentiate into qualitatively different T helper cells in vivo. It is also clear that the multiple cell lineages present in PBMCs are not required since infusions of activated CD4+T cells alone were sufficient to lead to effective viral load containment. These results confirm the critical role of CD4+ T-cell help in recent studies using structured treatment interruptions in subjects identified during acute HIV-1 infection.47 One interpretation of these findings is that the infused activated CD4+ T cells may provide licensing of the appropriate antigen-presenting cells via CD40/CD40L interaction, leading to the restoration of virus-specific CD8+ CTL responses. Our results further suggest that a central CD4+T-cell defect is the primary lesion in this model of SIV infection and most likely in HIV infection. Thus, replenishment of the host's pool of “functionally intact” CD4+ T cells appears sufficient to induce antiviral disease protective immune responses. This model provides a much needed tool to identify such a central CD4+ T-cell defect and its in vitro immune correlates, not only in SIV-infected monkeys but also in HIV-1–infected patients. The next step will be to test strategies to overcome this defect in CD4+ T cells collected at various stages after infection, which will be critical for the implementation as well as the identification of limitations of such immunotherapy in human patients.
The authors are deeply grateful to the staff of the Yerkes Regional Primate Research Center for their handling of the animals; to Dr Riley and Dr Levine for providing the protocol for the expansion of immunobead-activated CD4+ T cells; to Dr Bischofberger of Gilead Sciences for the generous supply of PMPA; to Dr Robinson and Dr Currier for their support in Vβ analyses; and to the National Institutes of Health reagent repository for the supply of some of the reagents utilized in these studies.
Supported by grants from American Foundation for AIDS Research 97-102009, National Institutes of Health 1RO1-27057, and AIDS research grants from the Health Science Foundation in Japan, Ministry of Health.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
François Villinger, Winship Cancer Institute, 1365B Clifton Rd, Emory University, Atlanta, GA 30322; e-mail: fvillin@emory.edu.