Trioma cell vaccination is a potent new immunologic approach for the therapy of malignant B-cell lymphoma. It is based on targeting tumor antigens to internalizing receptors on antigen-presenting cells (APCs). Tumor cells are fused to an APC-specific hybridoma, where they are converted to trioma cells that include potentially all lymphoma-derived antigens and that express the APC-binding arm. In this study, the mechanisms of trioma-mediated tumor immunity in immunocompetent mice were dissected, and it was shown in this model system that humoral anti-idiotypic immunity is indeed detectable after idiotype-specific immunization but that it does not reflect the degree of tumor protection obtained in vivo. Immunization against the idiotype alone was not sufficient for efficient tumor rejection in vivo. Targeting tumor antigens to APCs is only successful in terms of inducing tumor protection when designed as a polyvalent vaccination protocol.
Introduction
It is commonly accepted that immune responses are initiated by the uptake of antigens by specialized antigen-presenting cells (APCs) that activate antigen-specific T cells. The engulfment of antigens can occur through phagocytosis, macropinocytosis, or, most efficiently, by adsorptive endocytosis. It has been shown in vitro1-8 and in vivo9,10 that antibody-mediated targeting of antigens toward the endocytosing Fc receptors FcγRI and FcγRΙΙ that are expressed on APCs causes the antigen to be processed and presented to T lymphocytes. The induction of humoral responses in vivo was even possible against weak immunogens such as the immunoglobulin (Ig) idiotype (Id) of B-cell lymphomas,10which is an attractive target antigen for tumor immunotherapy because it is absolutely tumor specific. However, the impact of such anti-Id responses on tumor protection in vivo was not addressed in the latter study.
Triomas are B-lymphoma cells that have been modified to express an FcγR binding specificity.11 Originally, we set out to specifically assemble the lymphoma Id with an APC-binding arm. To this end, murine lymphoma cells were fused to a xenogeneic (rat) hybridoma expressing an FcγR-specific antibody (Ab). Because of preferential pairing between heavy and light chains of corresponding specificities observed when the parental Abs are of different species origin,12 the resultant trioma cells expressed a bispecific Ab including the lymphoma Id and the rat anti-APC–binding arm at high yield.11 Vaccination of mice with trioma cells induced a specific and long-lasting immunity against the wild-type tumor that was strictly dependent on CD4+ and CD8+ T cells.11 Even the eradication of established A20 lymphomas at day 6 was possible.13 This model allows us to define the significance of a humoral and a cellular anti-Id response for in vivo tumor protection. We show that, despite the ability to induce a humoral Id-specific response by targeting the Id to APCs,10 this reaction alone is not sufficient for efficient tumor protection in vivo. Other tumor-derived antigens included in the trioma cell seem to be primarily responsible for tumor rejection. The trioma approach, which is the most potent immunization protocol described to date in the A20 model, is obviously only successful because of its polyvalence.
Materials and methods
Cell culture and characterization of trioma cells
All cells were cultured in RPMI 1640 medium supplemented with 5% or 10% fetal calf serum, 2 mM glutamine, and 50 μM 2-mercaptoethanol at 37°C in a humidified 5% CO2atmosphere. A20 and MPC11 are B-cell lymphomas of BALB/c origin, 2.4G2 and NLDC-145 are rat hybridomas expressing an anti-FcR and an anti–DEC-205 monoclonal antibody (mAb), respectively, and 26II6 is a rat hybridoma with specificity against human CD3. S49 and P388D1 are cell lines expressing FcR and the DEC-205 antigen, respectively. Cell fusion was performed as described earlier.11 The variants BiVneg, BiVIdneg, and A20Idneg were generated by subcloning. Immunoglobulin quantitation in supernatants was conducted using enzyme-linked immunosorbent assay (ELISA) and fluorescence-activated cell sorter (FACS) analysis. In the ELISA, immunoglobulin proteins were captured by rat antimouse IgG2a mAb or goat antirat IgG and were detected with rat antimouse IgG or goat antirat IgG, respectively. Hybrid molecules were detected by capturing the mouse IgG2a Fc region with protein A and subsequent detection of the rat moiety using mouse (Fab)2 antirat IgG; the presence of the murine light chain in the hybrid molecule was verified by using rat antimouse kappa. Monoclonal and polyclonal antibodies were purchased from PharMingen (San Diego, CA) or Dianova (Hamburg, Germany). Binding of mAbs and of hybrid molecules to FcR or DEC-205 was tested by FACS analyses. Immunoglobulin was coated on S49 or P388D1 cells and was detected with fluorescein isothiocyanate-labeled goat antirat IgG or rat antimouse IgG. BiV- and A20-derived immunoglobulin and 2.4G2 mAb were purified from culture supernatants by protein A chromatography.11
Animal studies
In preimmunization experiments, groups of 6 female BALB/c mice (Bommice, Ry, Denmark) were injected intraperitoneally with 105 vaccine cells or 50 μg protein in phosphate-buffered saline. A boost was given after 3 weeks, and, after another 7 days, mice received an intraperitoneal tumor challenge with 105to 5 × 105 A20 cells. Therapy of established tumors was performed as previously described.13 Wild-type A20, when used as a vaccine, was irradiated at a dose of 15 Gy from a cesium 137 source. For blocking FcR in vivo, mice were injected intraperitoneally with 1 mg 2.4G2 mAb twice during vaccination. By this treatment, FcR was completely saturated. All experiments were performed at least in duplicate.
Anti-idiotype enzyme-linked immunosorbent assay
The humoral anti-Id response was determined by enzyme-linked immunosorbent assay (ELISA). Serum was taken 7 days after boosting and was incubated in serial dilutions on ELISA plates coated with A20 immunoglobulin purified from culture supernatant. As a detection reagent, mAbs directed against mouse IgG1, IgG2b, and IgG3 were used. Reactivity of sera with constant domains has been excluded by using irrelevant IgG2a as the capturing Ab. Serum titers were calculated as those reciprocal serum dilutions that gave a twofold extinction in the ELISA compared with the background.
T-cell assays
Spleen and mesenterial and inguinal lymph nodes were isolated from naive, immune, or tumor-bearing animals. After lysis of erythrocytes, 4 × 106 cells were stimulated in the presence of 5 × 105 irradiated A20 tumor cells or of 5 μg/mL purified BiV- or A20-derived immunoglobulin and 30 U/mL IL-2 (Amersham-Pharmacia, Freiburg, Germany). In additional stimulation rounds that followed after 10-day intervals, 106 syngeneic spleen cells and 5 × 105 irradiated A20 cells or soluble immunoglobulin, respectively, were added to 106 responder cells. Cellular reactivity was assessed by determining granulocyte macrophage–colony-stimulating factor (GM-CSF) secretion of serially diluted responder cells in the presence of 5 × 104 A20, MPC11, or A20Idneg cells or only medium. GM-CSF was measured by ELISA.14 For adoptive transfer, 5 × 105 in vitro stimulated T-cells were injected intraperitoneally into mice, along with a lethal A20 challenge. Cell-mediated lysis was quantitated in a standard 4-hour chromium Cr 51 release assay. Target cells (A20 or YAC) were labeled with 51Cr and were incubated with stimulated effector cells at varying effector-target ratios. Spontaneous release was determined by incubating target cells alone in complete medium.
Results
Significance of the lymphoma idiotype and other determinants for tumor protection in vivo
The trioma cell line BiV was generated by fusing the murine A20 lymphoma with the rat hybridoma 2.4G2 that produces an antimouse FcγR Ab.11 To unravel the mechanisms involved in trioma-dependent tumor immunization, we created an A20 Id loss mutant (A20Idneg) and an Id-deficient BiV variant (BiVIdneg) by subcloning. A BiV variant lacking the APC-binding arm (BiVneg) was described earlier.11 As demonstrated by FACS analyses, these variants did not differ from parental A20 and BiV, respectively, regarding the expression of immunologically relevant surface molecules, such as major histocompatibility complex (MHC) class I, MHC class II, CD40, CD80, or CD86. The rat-derived anti-FcR binding arm was present on the cell surfaces of BiV and BiVIdneg (not shown). Cytogenetic analyses showed that in all trioma variants, the number of chromosomes equaled the sum of chromosomes derived from A20 and 2.4G2. Thus, gross deletions in the subcloned mutants were excluded. Immunizing agents used in this study are compiled in Table 1.
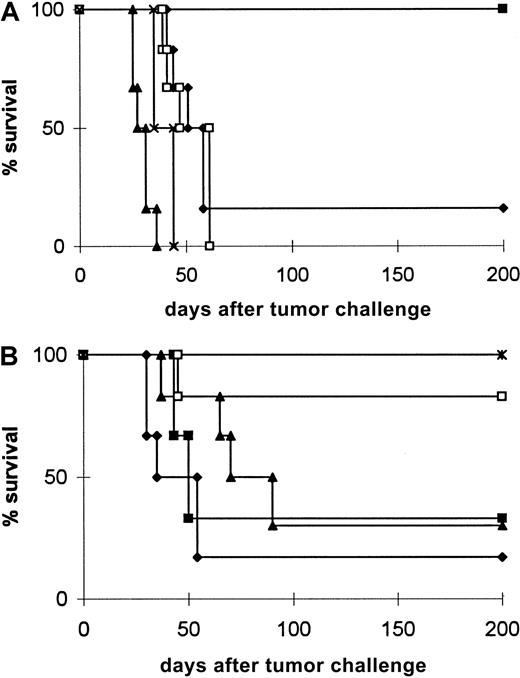
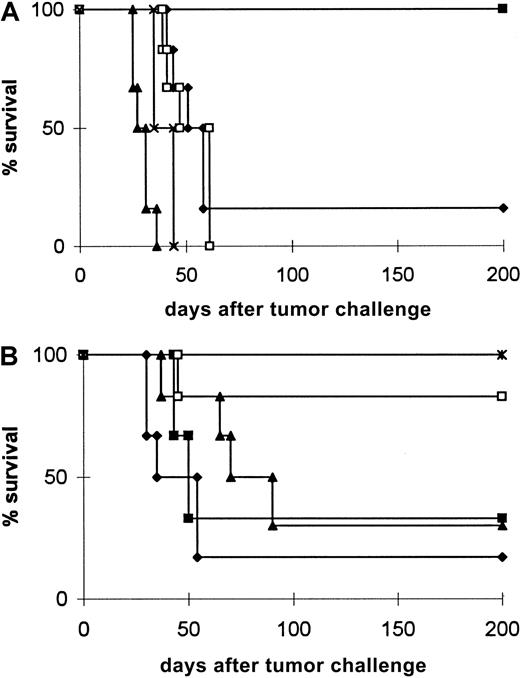
The most specific agent we generated for mounting an anti-Id response is the soluble bispecific Ab containing the Id and the APC-binding arm. Immunization with protein purified from BiV supernatant indeed gave rise to a considerable humoral anti-Id response (Table 2). However, when the protective effect of this Ab response was tested by challenging mice with a lethal tumor dose, only a modest survival benefit was observed (Figure1A, Table 1). This result was even obtained with the minimal tumorigenic dose of 105 cells. In contrast, a cellular BiV vaccine conferred 100% tumor protection (Figure 1A and 11), though the anti-Id titers induced were significantly lower than those obtained with protein vaccination (Table2). The difference between the BiV protein and BiV cells with regard to tumor protection may be related to the xenogenicity of the cellular vaccine that leads to its lysis with release and subsequent presentation of tumor-associated antigens other than the Id. While A20 wild-type cells also provide these antigens, they lack the xenogeneic moiety, as well as the ability to redirect antigens toward APCs; therefore, irradiated A20 cells were completely ineffective as immunogens. An alternative explanation for the superiority of the cellular vaccine could be priming against rat antigens leading to cross-recognition of A20 tumor antigens. To preclude this possibility, immunization was performed with rat hybridoma cells alone (not shown) or with a mixture of BiV protein and 26II6 hybridoma cells (Figure 1A, Table 1) that are also of rat origin but that differ from 2.4G2 by expression of a mAb that does not react with murine antigens.15 In both settings, no significant tumor protection was obtained. Thus, successful immunization seems to require xenogeneic cells that contain A20-derived antigens.
Protection of mice from A20 cells after vaccination with the indicated immunogens.
Mice received 2 immunizations, as described in “Materials and methods,” followed by challenge with 5 × 105 viable A20 (A, B) or A20Idneg cells (B). Representative results from 2 to 3 independent experiments are shown. The growth kinetics of A20Idneg in untreated mice is identical to that of wild-type A20. (A) ♦, BiV protein; ▪, BiV cells; ▴, irradiated A20 cells; ■, 26II6 cells + BiV protein; ×, tumor control. (B) ♦, BiVneg cells; ▪, BiV cells + 2.4G2 mAb; ▴, BiVneg cells + BiV protein; ■, BiVIdneg cells; ∗, BiV cells–A20Idneg challenge.
Protection of mice from A20 cells after vaccination with the indicated immunogens.
Mice received 2 immunizations, as described in “Materials and methods,” followed by challenge with 5 × 105 viable A20 (A, B) or A20Idneg cells (B). Representative results from 2 to 3 independent experiments are shown. The growth kinetics of A20Idneg in untreated mice is identical to that of wild-type A20. (A) ♦, BiV protein; ▪, BiV cells; ▴, irradiated A20 cells; ■, 26II6 cells + BiV protein; ×, tumor control. (B) ♦, BiVneg cells; ▪, BiV cells + 2.4G2 mAb; ▴, BiVneg cells + BiV protein; ■, BiVIdneg cells; ∗, BiV cells–A20Idneg challenge.
The requirement for targeting APCs was proven directly by using for immunization the BiVneg variant that had lost the anti-APC binding arm. This vaccine did not elicit a significant humoral anti-Id response (Table 2), nor did it confer efficient tumor rejection (Figure 1B, Table 1). Because wild-type A20 exerted no effect, the modest effect of BiVneg with 20% long-term survivors might have been attributed solely to the xenogeneic nature of this vaccine, which results in enhanced antigen presentation. Essentially the same result was observed when FcR was blocked with 2.4G2 mAb during vaccination with intact BiV cells (Figure 1B). If the sole mechanisms of trioma immunization are Id retargeting to APCs and enhanced antigen presentation after lysis of the xenogenized vaccine cells, the 100% protection provided by intact BiV cells should be reconstituted by mixing the purified BiV protein with BiVneg cells. This was, however, not possible: simultaneous vaccination with BiVneg cells and BiV protein yielded only 42% long-term survivors (Figure 1B, Table 1). Thus, the effect of intact BiV cells seems to be dependent on a third mechanism. Because the APC binding arm could be detected on the surface of all highly immunogenic trioma cells, we assume that a direct physical interaction between the trioma cell and the APC may be mandatory for optimal in vivo effects. If this holds true, it could be predicted that retargeting of the intact xenogenized vaccine cells to APCs by the APC binding arm would be sufficient for tumor protection, irrespective of the Id. To test this possibility, mice were vaccinated with the BiVIdneg variant that expresses the anti-FcR specificity but not the A20 Id. Approximately 70% of the animals rejected the tumor after immunization (Figure 1B, Table 1). These data indicate that the Id indeed does not play a pivotal role in BiV-mediated tumor protection. This hypothesis was confirmed in an experiment in which animals were vaccinated with intact BiV cells and were challenged with an A20 mutant that had lost the Id. Like the wild-type tumor, this variant was rejected in all animals (Figure 1B).
Cellular response induced by trioma immunization
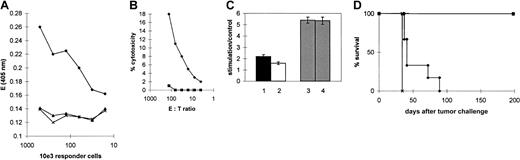
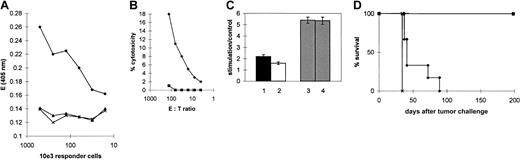
Having demonstrated that anti-Id serum Ab titers were not predictive for lymphoma protection in vivo and that antigens other than the Id are likely to be the major targets of tumor rejection in the trioma model, we analyzed the role of cellular effectors and their Id specificity. Spleen and lymph node cells were isolated from immune mice and were stimulated in vitro with irradiated A20 cells, as outlined in “Materials and methods.” Cell activation was measured by determining GM-CSF secretion in the presence of A20, A20Idneg, or the irrelevant syngeneic MPC11 tumor. As shown in Figure2A, specific reactivity against A20 cells was detected after 2 rounds of stimulation in vitro. CD4+and CD8+ T cells were identified in a ratio of 80: 20. In a51Cr release assay, CTLs specifically activated in vitro against A20 were capable of lysing A20 cells (Figure 2B). By using trioma cells as stimulators in similar in vitro systems, we could confirm the dependence of trioma immunization on APCs because the antibody-mediated depletion of CD14+ cells completely abrogated T-cell activation (unpublished observations, 1999/2000). To assess the role of targeting to the APC surface molecule in vitro, we stimulated responder cells with the purified bispecific BiV protein or the unmodified A20 Ig, respectively, in the presence of syngeneic spleen cells. As expected, the stimulatory effect was more pronounced when BiV protein was used than when unmodified Id was used (Figure 2C). When whole lymphoma cells were used as stimulators, however, the Id-specific response seemed to be inferior to the response directed against unspecified A20 antigens, since after vaccination of mice with intact BiV cells and subsequent in vitro stimulation, reactivity against the mutant A20Idneg cells was not reduced compared with wild-type A20 (Figure 2C). Hence, as found in the in vivo tumor protection experiments, the in vitro assays also indicated an inferior role of Id immunity in tumor protection. On adoptive transfer, T cells conferred 100% tumor protection provided they were generated from BiV cell-vaccinated animals and were restimulated in vitro with A20 cells. Intermittent stimulation with BiV protein resulted in prolonged survival but not in long-lasting tumor protection (Figure 2D).
Characterization of A20-specific effector cells.
(A) A20-specific reactivity of cells recovered from 2 BiV cell-vaccinated mice and restimulated twice in vitro with A20 (♦), MPC11 (▴), or medium (×). As a readout for cellular activation, the extinction obtained in the GM-CSF ELISA is shown. (B) Cytotoxicity against A20 (♦) or YAC cells (▪) exerted by effector cells that were isolated from BiV-vaccinated mice and that showed A20-specific activation after in vitro restimulation. (C) Activation of effector cells against A20 (columns 1-3) and A20Idneg cells (column 4) after stimulation with BiV protein (black column), A20 protein (white column), or A20 cells (shaded columns). Activation was measured in the GM-CSF ELISA as outlined in “Materials and methods.” The y-axis shows the ratio of the extinctions obtained with specific and control stimulation at a responder cell number of 1.25 × 105. (D) Adoptive transfer of in vitro-stimulated T cells. Spleen cells of BiV-immunized mice were stimulated only with irradiated A20 cells (▪) or with A20 cells first and BiV protein in the following stimulation rounds (♦). 5 × 105 effector cells were transferred together with a lethal A20 tumor challenge. Both CD4+ and CD8+ T cells were present in the transferred cell population. ×, tumor control.
Characterization of A20-specific effector cells.
(A) A20-specific reactivity of cells recovered from 2 BiV cell-vaccinated mice and restimulated twice in vitro with A20 (♦), MPC11 (▴), or medium (×). As a readout for cellular activation, the extinction obtained in the GM-CSF ELISA is shown. (B) Cytotoxicity against A20 (♦) or YAC cells (▪) exerted by effector cells that were isolated from BiV-vaccinated mice and that showed A20-specific activation after in vitro restimulation. (C) Activation of effector cells against A20 (columns 1-3) and A20Idneg cells (column 4) after stimulation with BiV protein (black column), A20 protein (white column), or A20 cells (shaded columns). Activation was measured in the GM-CSF ELISA as outlined in “Materials and methods.” The y-axis shows the ratio of the extinctions obtained with specific and control stimulation at a responder cell number of 1.25 × 105. (D) Adoptive transfer of in vitro-stimulated T cells. Spleen cells of BiV-immunized mice were stimulated only with irradiated A20 cells (▪) or with A20 cells first and BiV protein in the following stimulation rounds (♦). 5 × 105 effector cells were transferred together with a lethal A20 tumor challenge. Both CD4+ and CD8+ T cells were present in the transferred cell population. ×, tumor control.
Targeting antigens to DEC-205 is less effective
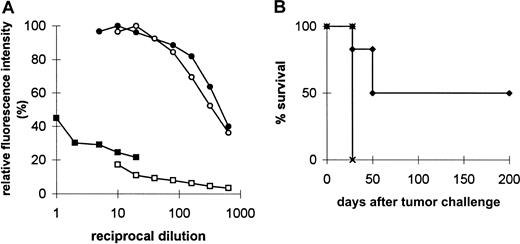
NLDC-145 is a rat hybridoma16 that secretes an mAb against DEC-205 described as an endocytosing receptor on dendritic cells with homology to a mannose receptor.17 To compare antigen presentation initiated by this receptor and by FcR, the 4D7 trioma cell line was created by fusing A20 to NLDC-145. A20 Id and DEC-205 specificity were expressed on the surface of 4D7 cells and were secreted into the supernatant, as shown by ELISA and FACS analyses (not shown). The expression level of the A20 Id and of the rat-binding arm was comparable in 4D7 and BiV cells. Rat–mouse hybrid molecules detected in a double-isotype ELISA were present in similar amounts in 4D7 and BiV supernatants, respectively. Binding of the rat moiety of 4D7 to the target antigen on P388D1 cells, however, was reduced more than 50-fold when compared to binding of BiV to FcR-expressing S49 cells. The same result was obtained when binding activity of the unmodified NLDC-145 rat mAb was measured in comparison with 2.4G2 from which BiV was derived (Figure 3A). Obviously, the antigen density on the target cells or the affinity of binding to the respective antigen is lower in NLDC-145 and 4D7. To test the in vivo consequences of this finding, mice were immunized with 4D7 and were challenged with A20 wild-type tumor. As shown in Figure 3B, only 50% of the animals successfully rejected the tumor. The same result was obtained in a therapeutic situation, when mice first received tumor challenge and subsequently received an injection of trioma cells. Thus, antigen targeting to FcR seems to be more efficient than antigen targeting to DEC-205 in terms of inducing a protective antitumor response.
Characterization and in vivo effects of 4D7 trioma cells.
(A) Binding of immunoglobulin from trioma (▪, 4D7; ●, BiV) and the corresponding parental hybridoma supernatants (■, NLDC-145, ○, 2.4G2) to P388D1 or S49 cells. Binding occurs by way of the rat moiety. Bound immunoglobulin is detected with fluorescein isothiocyanate-conjugated goat antirat IgG (parental hybridomas) or rat antimouse IgG (triomas). Maximum fluorescence is expressed as 100%. (B) Tumor protection conferred by 4D7 trioma cells. Animals were preimmunized and challenged as described in Figure 1. ▴, 4D7 vaccination; ×, tumor control.
Characterization and in vivo effects of 4D7 trioma cells.
(A) Binding of immunoglobulin from trioma (▪, 4D7; ●, BiV) and the corresponding parental hybridoma supernatants (■, NLDC-145, ○, 2.4G2) to P388D1 or S49 cells. Binding occurs by way of the rat moiety. Bound immunoglobulin is detected with fluorescein isothiocyanate-conjugated goat antirat IgG (parental hybridomas) or rat antimouse IgG (triomas). Maximum fluorescence is expressed as 100%. (B) Tumor protection conferred by 4D7 trioma cells. Animals were preimmunized and challenged as described in Figure 1. ▴, 4D7 vaccination; ×, tumor control.
Discussion
It was demonstrated earlier that antigen targeting to internalizing receptors on APCs is an efficient tool for immunization.1-10 An Ab response could be induced even against the weakly immunogenic Id of B-cell lymphomas by targeting to FcR.10 This was originally the rationale of the trioma cell approach that was developed to redirect a lymphoma Id to APCs by converting the Id to a bispecific Ab containing an FcR-binding arm.11 Using this model, we verified here the induction of a humoral anti-Id response by vaccination with trioma-derived immunoglobulin. The most rigorous test of tumor immunity, however, is the tumor challenge. Therefore, we examined tumor rejection in vivo after vaccination with FcR-targeting reagents and noted that the humoral response did not reflect the efficiency of tumor protection. Purified trioma protein induced considerably higher anti-Id titers than the cellular trioma vaccine, whereas an inverse hierarchy became apparent with regard to lymphoma rejection. Whereas BiV cells conferred 100% protection, immunization with the purified BiV protein mediated only a marginal survival benefit with 18% long-term survivors. Thus, in our model it was not sufficient to measure the humoral anti-Id response to predict tumor rejection.
Because immunization with the cellular trioma vaccine was successful despite minimal anti-Id serum Ab titers, we examined to what extent the lymphoma Id contributed to the efficacy of the cellular trioma approach. The Id was shown to play a minor role for tumor protection. Even trioma Id loss mutants were able to convey tumor rejection, albeit at a somewhat lower efficiency than intact trioma cells (Figure 1). Also, in a therapeutic experimental setting, these mutants were able to protect mice, all of which also rejected an A20 rechallenge given after approximately 100 days (not shown). These results were confirmed by immunization with intact BiV, followed by challenge with an A20 Id loss mutant, that provided 100% protection. From the current data, we cannot conclude, of course, that the protective effect of the Id is weak compared with other single tumor antigens. There is no doubt, though, that for efficient tumor protection, the whole panel of antigens provided by the tumor cell is superior to the Id alone. This has also been observed in other vaccination models.14Using the cellular vaccine is not only the prerequisite for efficacy in vivo, it also circumvents cumbersome protein purification steps required for isolation of Id proteins or the necessity of isolating Id genes from the lymphoma.
In summary, one determinant for the potency of trioma immunization is the polyvalent immunization achieved by trioma cells because they include not only the Id but also other antigens derived from the parental lymphoma cell. This is an advantage for clinical application given that the in vivo selection of escape mutants is obviated. As was revealed by a series of vaccinations using mutant cells and by reconstitution experiments, the trioma approach seems to depend on 2 other essential features. First, immunization against tumor antigens is enhanced because of the xenogeneic nature of trioma cells, which may give rise to cell lysis and antigen release. Finally, the most important determinant for tumor protection involves the redirection of tumor antigens (including the Id) to FcR-bearing APCs. Hence, physical contact of vaccine cells expressing anti-FcR specificity on their surfaces and FcR-positive APCs may be required.
Our findings pave the way for the clinical application of the trioma strategy. Human B-cell lymphomas can be treated even after loss of the Id. To avoid injection of xenogeneic cells, the approach can be modified to an allogeneic setting. The immune response against xenogeneic or allogeneic determinants after multiple injections should not pose serious problems because rapid elimination of the vaccine cells is desired for the release and presentation of tumor antigens (see above). Given that polyvalent immunization against multiple antigens provided by intact trioma cells may raise the risk of autoimmunity, we subjected mice to extensive histologic examination after vaccination. As found using immunization protocols based on autologous tumor cells modified to express T-cell–activating cytokines or costimulatory surface molecules,18 signs of auto-aggressive disease were not observed (data not shown). Apparently, it is not possible to break tolerance against normally expressed self-antigens.19
Furthermore, our results show that tumor-specific T cells may be instrumental for mediating tumor immunity. In previous studies, we demonstrated that the antitumor effect in vivo was abrogated by the depletion of CD4+ or CD8+ T lymphocytes.11 Here we show that A20-specific effector cells can be generated from spleens of immunized mice after stimulation in vitro. These studies revealed that the Id is not the dominant antigen responsible for tumor recognition in vitro. Moreover, adoptive transfer of T cells that were stimulated with Id-derived protein was not successful in contrast to the transfer of effector cells stimulated with whole tumor cells. Nevertheless, it is conceivable that Id-reactive T cells20 are present among the polyclonal tumor-specific cell population. The questions as to how frequently such cells develop after trioma vaccination and whether they are functional in vivo have to be addressed in ongoing studies.
We thank Dr H. Hameister (Ulm) for karyotyping mouse cell lines and Dr R. Schuh (Fresenius AG) for providing the 26II6 hybridoma. We also thank Drs D. J. Schendel and B. Frankenberger for critically reading the manuscript. In addition, we thank H. Jennen, J. Jasny, and B. Konkol for their excellent technical assistance. This article is dedicated to H. Jennen, who died on November 1, 2000.
Supported in part by the HGF-Strategiefonds “Infektionsabwehr und Krebsprävention.”
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Ralph Mocikat, GSF-Institut für Molekulare Immunologie, Marchioninistr 25, D-81377 Munich, Germany; e-mail:mocikat@gsf.de.