Primitive hematopoietic stem cells (HSCs) in the bone marrow are rare pluripotent cells with the capacity to give rise to all lineages of blood cells. During commitment, progenitor cells are composed mainly of cells with the potential for differentiation into 1 or 2 lineages. This commitment involves the acquisition of specific growth factor receptors and the loss of others. Viral and bacterial infections may lead to profound disturbance of hematopoiesis, which is possibly due to different susceptibility of HSCs to infectious agents. Here, we show that quiescent human HSCs are fully resistant to infection by the intracellular bacteria, Listeria monocytogenes andSalmonella enterica serovariationtyphimurium, and the extracellular pathogen Yersinia enterocolitica. During myeloid/monocytic differentiation induced by incubation with stem cell factor, thrombopoietin, and flt-3 ligand, partially differentiated HSCs emerge, which readily take up these pathogens and also latex beads by macropinocytosis. After further monocytic differentiation, bacterial uptake by macropinocytosis still occurs but internalization of the pathogens is now mainly achieved by receptor-mediated phagocytosis. These results suggest that in the case of HSCs uptake mechanisms for bacteria develop sequentially.
Introduction
Hematopoietic proliferation and differentiation is sustained by a pool of hematopoietic stem cells (HSCs). HSCs are generated in the bone marrow and are able to differentiate into erythrocytes, granulocytes, monocytes, megacaryocytes, and lymphocytes. Hematopoiesis is regulated by a network of growth factors and related cytokines.1 Hematopoietic growth factors act on committed progenitors to increase their survival and to amplify maturing populations by stimulating proliferation. Differentiation into these specialized blood cells can be induced in vitro by a cocktail containing specific cytokines and growth factors.2
Infection of adult HSCs by bacteria has not been studied yet. Facultative intracellular bacteria, such as Salmonella entericaserovariation typhimurium and Listeria monocytogenes, but also extracellular bacteria, such asYersinia enterocolitica, are taken up by members of the myeloid lineage, in particular monocytes, macrophages, and dendritic cells.3,4 These cells internalize bacteria by macropinocytosis and by receptor-mediated phagocytosis (Fc, complement, and β1-integrin receptors).5-7 In addition, intracellular bacteria can be internalized by nonphagocytic mammalian cells via triggered phagocytosis supported by special bacterial surface proteins.8-10 These bacterial surface proteins do not seem to play a major role for bacterial uptake in professional phagocytic cells such as monocytes, macrophages, and dendritic cells.6
After internalization, some of the bacteria are able to survive in the mammalian host cells. The intracellular bacteria S typhimuriumand L monocytogenes replicate extensively in modified phagosomes or the host cell cytosol, respectively.11-13Bacterial survival in the host cell might explain the rapid apoptosis of monocytes, macrophages, and dendritic cells after infection byS typhimurium,3,12 whereas cells infected withL monocytogenes survive for a longer time.4,14Pathogenic Yersinia species promote apoptosis of macrophages via secreted Yop proteins.15
The question whether adult HSCs can be infected by intracellular bacteria is important to answer because infected HSCs might be a source for generations of infected differentiated cells. In addition, infection of bone marrow progenitors may contribute to a hematologic manifestation of bacterial infection.
The aim of our study was to evaluate the susceptibility of quiescent HSCs and monocytic differentiated progenitor cells to bacterial infection.
Materials and methods
Isolation of human CD34+ progenitor cells derived from peripheral blood cells
After informed consent was obtained from patients, cells were collected by apheresis during hematopoietic recovery after chemotherapy and treatment with recombinant subcutaneous granulocyte colony-stimulating factor. A 4-mL cell suspension from the pilot aliquot was used for positive selection of CD34+cells.
Positive selection of CD34+ cells and isolation of the CD14+ fraction
The CD34+ selection kit from Miltenyi Biotec (Bergisch Gladbach, Germany) was used. After washing, the cell pellet was resuspended in 300 μL buffer (phosphate-buffered saline supplemented with 0.5% bovine serum albumin, and 2 mM EDTA [ethylenediaminetetraacetic acid]) per 5 × 108 cells. The cell suspension was incubated with Fc receptor–blocking reagent (human immunoglobulins) and subsequently with monoclonal hapten-conjugated anti-CD34 antibody (clone QBEND/10, mouse IgG1) for 15 minutes at 6°C. Following an additional washing step, the stained cell suspension was incubated with colloidal superparamagnetic magnetic-activated cell-sorter (MACS) microbeads conjugated to an antihapten antibody in a final volume of 500 μL/5 × 108 cells for 15 minutes at 6°C. For positive selection cells were again washed and resuspended in buffer (2 × 108 cells/mL). After passing through a filter to remove clumps, cells were applied to the selection column (Type VS+) and inserted into the magnetic field of the VarioMACS system (both from Miltenyi Biotech, Bergisch-Gladbach, Germany). Following 3 rinses, the VS+ column was removed from the magnetic field and the selected cells were eluted in buffer. To further enrich the CD34+ cells, eluted cells were applied to an additional positive selection column (RS+ column for 107 CD34+ cells) with an analogous procedure. The final CD34+ cell suspension was eluted in 1 mL buffer. The CD34+ cells were used for the experiments either directly or after storage in liquid nitrogen. The expression of surface molecules was evaluated by flow cytometry after direct staining with phycoerythrin (PE)–conjugated or fluorescein isothiocyanate (FITC)–conjugated anti-CD3, anti-CD13, anti-CD14, anti-CD16 (FcγRIII), anti-CD19, anti-CD29 (integrin β1 chain), anti-CD32 (FcγRII), anti-CD33, anti-CD34, anti-CD64 (FcγRI), and anti-CD206 (macrophage mannose receptor) antibodies (Pharmingen, Hamburg, Germany).
Positive selection of the CD14+ cell fraction was performed as described above with the use of monoclonal hapten-conjugated anti-CD14 antibody instead of anti-CD34 antibodies.
Differentiation of HSCs toward monocytes
Bacteria
Bacterial strains used in this study are L monocytogenes Sv 1/2a EGD, L monocytogenes Sv 1/2a EGD Psod gfp (resistance-marker tetracycline),17Y enterocolitica, S typhimurium14028S.18 The bacteria were grown in brain-heart infusion (BHI) medium at 30°C (Yersinia) or 37°C (Listeria, Salmonella) until they reached the mid-log phase of growth.
In vitro bacterial infection of HSCs
Cells (5 × 105 cells/mL) were infected with bacteria. Bacteria were added in the multiplicity of infection of 10. The cultures were incubated in RPMI 1640 medium supplemented with 10% pooled human AB serum at 37°C for 1 hour. For selective removal of extracellular bacteria, 100 μg/mL gentamicin (Gibco, Karlsruhe, Germany) was added.
For determination of colony-forming units the cells were washed 30 minutes after addition of gentamicin with phosphate-buffered saline, lysed by the addition of ice-cold distilled water, and incubated for 20 minutes on ice. Serial dilutions were plated out on BHI agar.
Determination of bacteria in HSCs by light microscopy after Giemsa staining
After 1 hour of infection, cells were centrifuged on coverslips, fixed with methanol for 5 minutes, stained with Giemsa 1:20 (Merck, Darmstadt, Germany) for 20 minutes, and then examined using a Leitz Dialux 20 microscope (Leica, Solms, Germany).
Fluorescence microscopy
Green fluorescent protein (GFP)–expressing L monocytogenes in CD14+ and CD34+ HSCs were visualized by using a fluorescence-equipped inverted phase-contrast microscope and photographed with a digital imaging system camera (Visitron, Puchheim, Germany). Images were generated with the help of MetaMorph Imaging software (Universal Imaging, West Chester, PA).
Transmission electron microscopy
At 1 hour after infection, cells were washed, fixed in 2.5% glutaraldehyde, postfixed in 2% osmium tetroxide, stained with 0.5% uranyl acetate, dehydrated in graded alcohols, and finally embedded in Lowicryl K4M.
Uptake studies with green fluorescent latex beads or lucifer yellow
To evaluate macropinocytosis HSCs were incubated with green fluorescent latex beads (polystyrene, amine-modified, diameter 1 μm; Sigma-Aldrich, Steinheim, Germany) or lucifer yellow (1 mg/mL; Sigma-Aldrich) for 60 minutes at 4°C and 37°C. The difference in the number of fluorescent cells between incubation at 37°C and 4°C corresponds to the uptake rate of latex beads/lucifer yellow. Uptake rate was determined by fluorescence microscopy and flow cytometry.
Uptake inhibition studies
Throughout the duration of inhibition studies, infection media contained either 5 mg/mL yeast mannan (Sigma-Aldrich), the competitor of mannose/fucose receptor, 100 μM of the macropinocytosis inhibitor 5-(N, N-dimethyl)–amiloride, or 50 μg/mL fibronectin from human plasma (Sigma-Aldrich), the inhibitor of β1-integrin receptor.7 19
Analysis of cell death process
The percentage of cell death after bacterial infection was analyzed after staining the cells with propidium iodide (1 μg/mL) by fluorescence microscopy. For visualizing the nuclear morphology, HSCs were incubated with bisbenzimide dye (Hoechst 33342, 5 μg/mL; Merck) at 37°C for 15 minutes.
Statistical analysis
The data are presented as mean values and SDs of a representative experiment. All experiments were performed at least 3 times with cells from different donors. The number of infected cells and the number of intracellular bacteria per 100 cells were counted in triplicate. For statistical comparison t test was performed; P < .05 was considered as statistically significant.
Results
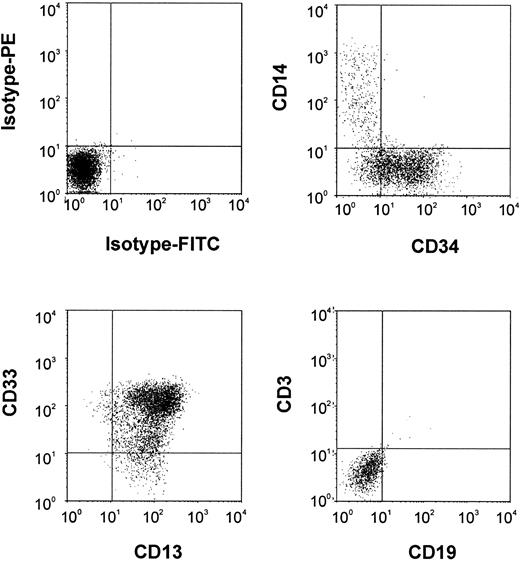
To study susceptibility of quiescent HSCs to bacterial infection, we isolated a purified fraction of human CD34+ HSCs from human peripheral blood cells. The obtained cell population consisted of more than 95% CD34+ cells and less than 2% cells expressing CD3, CD19, or CD14, specific markers for T cells, B cells, and monocytes, respectively (Figure1).
Surface marker analysis of purified human CD34+ HSCs.
FACS analysis was done after staining cells with FITC-labeled (x-axis) and PE-labeled (y-axis) monoclonal antibodies.
Surface marker analysis of purified human CD34+ HSCs.
FACS analysis was done after staining cells with FITC-labeled (x-axis) and PE-labeled (y-axis) monoclonal antibodies.
The CD34+ HSCs were incubated with L monocytogenes, Y enterocolitica, and S entericaserovariation typhimurium and the uptake of bacteria into HSCs was determined by light microscopy after Giemsa staining, transmission electron microscopy, or by green fluorescent bacteria, and by the determination of intracellular viable bacterial cell counts.
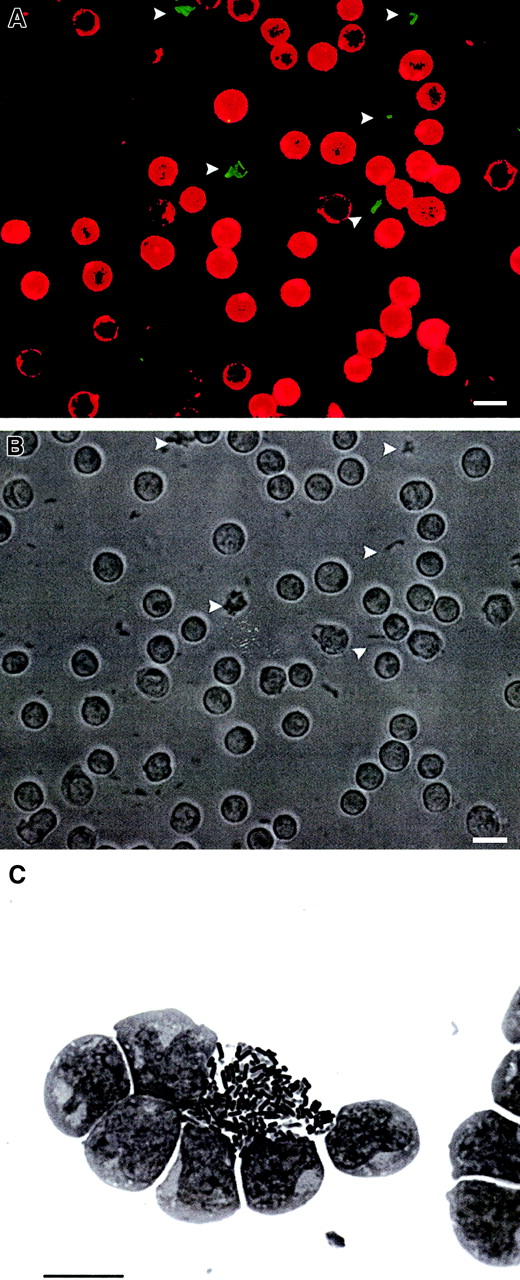
No bacteria were detected inside HSCs after a 1-hour or after an extended 24-hour incubation period with L monocytogenes,S typhimurium, or Y enterocolitica(Figure 2). These results clearly indicate that quiescent HSCs are resistant to infection by these pathogens.
Quiescent HSCs are resistant to infection by bacteria.
(A) Fluorescence microscopic image. Detection of CD34+ HSCs (stained with anti–CD34-PE antibodies) and extracellular, green fluorescent L monocytogenes(arrowheads) carrying the gfp gene under control of the constitutively active sod promotor (1 hour after infection; bar, 10 μm). (B) Light microscopic image of the identical field (1 hour after infection; bar, 10 μm); bacteria are marked with arrowheads. (C) No uptake of Y enterocolitica in quiescent HSCs (Giemsa staining at 24 hours after infection; bar, 10 μm).
Quiescent HSCs are resistant to infection by bacteria.
(A) Fluorescence microscopic image. Detection of CD34+ HSCs (stained with anti–CD34-PE antibodies) and extracellular, green fluorescent L monocytogenes(arrowheads) carrying the gfp gene under control of the constitutively active sod promotor (1 hour after infection; bar, 10 μm). (B) Light microscopic image of the identical field (1 hour after infection; bar, 10 μm); bacteria are marked with arrowheads. (C) No uptake of Y enterocolitica in quiescent HSCs (Giemsa staining at 24 hours after infection; bar, 10 μm).
Next, HSCs were differentiated toward monocytes.2 16Incubation of HSCs in differentiation medium (see “Materials and methods”) led to the up-regulation of the myeloid markers CD13 and CD33 and monocytic antigens such as CD14. No surface expression of CD3 and CD19, markers characteristic for T and B cells, were detected (Figure 3).
Surface marker analysis of partially differentiated 5d-HSCs.
FACS analysis was done after cells were stained with FITC-labeled (x-axis) and PE-labeled (y-axis) monoclonal antibodies.
Surface marker analysis of partially differentiated 5d-HSCs.
FACS analysis was done after cells were stained with FITC-labeled (x-axis) and PE-labeled (y-axis) monoclonal antibodies.
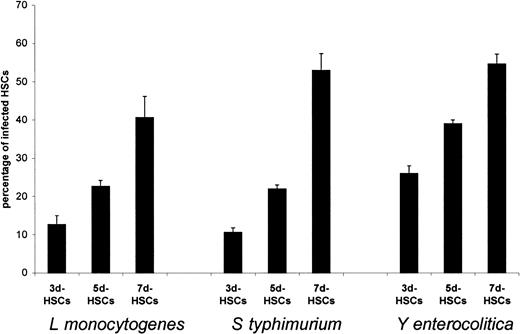
The capability of bacterial uptake by partially differentiated HSCs was measured at several stages of cell development. We studied infection of HSCs that were incubated for 3, 5, and 7 days in the described cell culture medium (termed in the following as 3d-, 5d-, and 7d-HSCs).
As shown in Figure 4, we found a correlation between the stage of cell development mediated by incubation in the growth factor combination and the efficiency of bacterial uptake. Depending on the HSC donor, the numbers of internalized bacteria showed some variation. However, for all donors tested the portion of infected HSCs was significantly higher for 5d-HSCs than for 3d-HSCs.
Comparison of bacterial uptake into 3d-, 5d-, and 7d-HSCs.
Determination of internalized bacteria in human partially differentiated HSCs by light microscopy after Giemsa staining (1 hour after the addition of bacteria). The results from a representative experiment are presented as mean values and SDs (error bars); determination was done in triplicate.
Comparison of bacterial uptake into 3d-, 5d-, and 7d-HSCs.
Determination of internalized bacteria in human partially differentiated HSCs by light microscopy after Giemsa staining (1 hour after the addition of bacteria). The results from a representative experiment are presented as mean values and SDs (error bars); determination was done in triplicate.
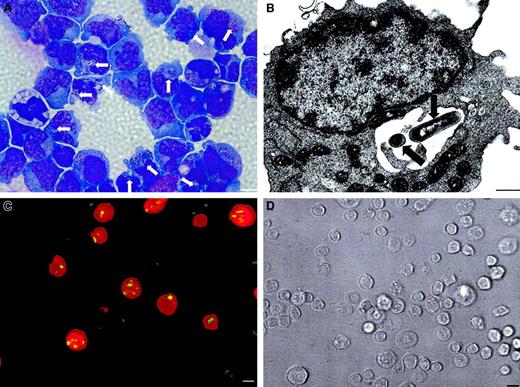
The 5d-HSCs internalized L monocytogenes (Figure 5A,B), S typhimurium, andY enterocolitica quite efficiently. Most infected 5d-HSCs expressed the CD14 surface marker, whereas noninfected HSCs were CD14− (Figure 5C,D). For reinforcement of these findings, CD14+ 5d-HSCs were isolated by cell sorting and infected with the 3 bacterial strains. This purified CD14+5d-HSC population showed an increased susceptibility to infection with infection rates of 53%, 42%, and 70% for L monocytogenes,S typhimurium, and Y enterocolitica, respectively. These results suggest a correlation between the susceptibility of HSCs to bacterial infection and the appearance of the monocytic maturation marker CD14.
Partially differentiated 5d-HSCs internalize bacteria.
(A) Phagocytosed L monocytogenes in 5d-HSCs (arrows; Giemsa staining at 1 hour after infection; bar, 10 μm). (B) Transmission electron microscopy reveals phagosomal bacteria (arrows) at 1 hour after infection (bar, 0.6 μm). (C) Fluorescence microscopic image. Detection of CD14+ partially differentiated HSCs (stained with anti–CD14-PE antibodies) and superimposed, intracellular green fluorescent L monocytogenes (yellow) carrying thegfp gene under control of the constitutively activesod promotor (1 hour after infection; bar, 10 μm). (D) Light microscopic image of the identical field (bar, 10 μm).
Partially differentiated 5d-HSCs internalize bacteria.
(A) Phagocytosed L monocytogenes in 5d-HSCs (arrows; Giemsa staining at 1 hour after infection; bar, 10 μm). (B) Transmission electron microscopy reveals phagosomal bacteria (arrows) at 1 hour after infection (bar, 0.6 μm). (C) Fluorescence microscopic image. Detection of CD14+ partially differentiated HSCs (stained with anti–CD14-PE antibodies) and superimposed, intracellular green fluorescent L monocytogenes (yellow) carrying thegfp gene under control of the constitutively activesod promotor (1 hour after infection; bar, 10 μm). (D) Light microscopic image of the identical field (bar, 10 μm).
To analyze the uptake mechanisms at the different stages of stem cell development experiments were carried out in 3d-, 5d- and 7d-HSCs with the inhibitor of macropinocytosis amiloride. Amiloride (100 μM) reduced the internalization process of L monocytogenes, S typhimurium, or Y enterocoliticaby 3d-HSCs and 5d-HSCs (Figure 6). In contrast, amiloride did not impair the uptake of L monocytogenes by 7d-HSCs. The uptake of S typhimuriumand Y enterocolitica was still impaired, but the extent of uptake inhibition was lower in comparison to the effect of amiloride on 3d-HSCs and 5d-HSCs (Figure 6).
Inhibition of the uptake of bacteria and latex beads with an inhibitor of macropinocytosis.
Comparison of bacterial uptake and the uptake of latex beads into 3d-, 5d-, and 7d-HSCs in the absence and presence of amiloride, an inhibitor of macropinocytosis (*P < .05, **P < .001, t test). The results from a representative experiment are presented as mean values and SDs (error bars); determination was done in triplicate.
Inhibition of the uptake of bacteria and latex beads with an inhibitor of macropinocytosis.
Comparison of bacterial uptake and the uptake of latex beads into 3d-, 5d-, and 7d-HSCs in the absence and presence of amiloride, an inhibitor of macropinocytosis (*P < .05, **P < .001, t test). The results from a representative experiment are presented as mean values and SDs (error bars); determination was done in triplicate.
To exclude a support of special surface proteins for the uptake of the bacteria into HSCs, we also determined the uptake of fluorescent latex beads. Uptake of latex beads (1 μm diameter) by 3d-, 5d-, and 7d-HSCs could be demonstrated (Figure 6). As expected, the uptake of latex beads by 3d-, 5d-, and 7d-HSCs was significantly reduced by 100 μM amiloride (Figure 6).
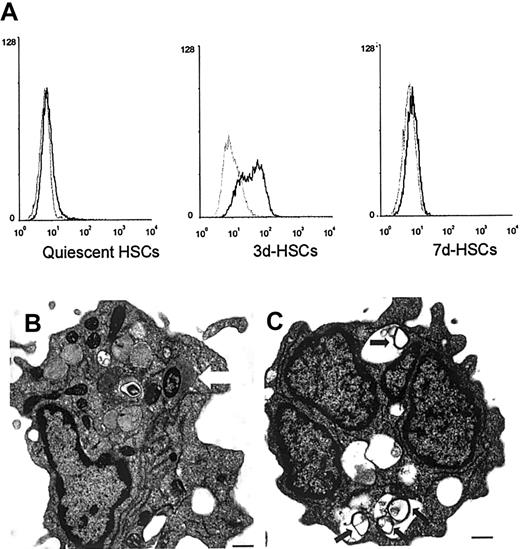
Direct evidence for macropinosome formation was demonstrated by the ingestion of lucifer yellow. In contrast to quiescent HSCs, 3d-HSCs were able to ingest lucifer yellow. Further differentiation of HSCs reduced lucifer yellow accumulation (7d-HSCs; Figure7A).
Uptake of lucifer yellow, and live or heat-killed
L monocytogenes by HSCs. (A) Uptake of lucifer yellow by HSCs. Histograms: fluorescence intensity in a logarithmic scale (x-axis) was plotted against cell numbers (y-axis). Black histograms show the fluorescence of HSCs incubated with lucifer yellow at 37°C, and gray histograms show the fluorescence of HSCs incubated with lucifer yellow at 4°C (negative control). (B) Transmission electron microscopy reveals live cytosolic L monocytogenes beginning actin polymerization at 2 hours after infection (arrow; bar, 0.6 μm). (C) The 5d-HSCs were able to internalize heat-killed L monocytogenes, which were degraded in the lysosomal compartments (arrows; transmission electron microscopy; bar, 0.6 μm).
Uptake of lucifer yellow, and live or heat-killed
L monocytogenes by HSCs. (A) Uptake of lucifer yellow by HSCs. Histograms: fluorescence intensity in a logarithmic scale (x-axis) was plotted against cell numbers (y-axis). Black histograms show the fluorescence of HSCs incubated with lucifer yellow at 37°C, and gray histograms show the fluorescence of HSCs incubated with lucifer yellow at 4°C (negative control). (B) Transmission electron microscopy reveals live cytosolic L monocytogenes beginning actin polymerization at 2 hours after infection (arrow; bar, 0.6 μm). (C) The 5d-HSCs were able to internalize heat-killed L monocytogenes, which were degraded in the lysosomal compartments (arrows; transmission electron microscopy; bar, 0.6 μm).
We also measured the uptake of heat-killed bacteria by 5d-HSCs. In comparison to viable L monocytogenes, which escape into the cytosol of the host cell and start polymerization of F-actin (Figure7B), internalized heat-killed bacteria were always located in membrane-surrounded vacuoles and were rapidly degraded (Figure 7C). Hence, we suggest that fusion with late endosomes (lysosomes) takes place at this state of HSC differentiation.
Human serum, but not fetal calf serum, significantly stimulated the uptake of L monocytogenes by 7d-HSCs (Table1), whereas uptake in 3d-HSCs and 5d-HSCs was less inducible by human serum.
Percentage of L monocytogenes- and Y enterocolitica-infected 3d-, 5d-, and 7d-HSCs treated with different infection media
| . | No additive . | + 10% fetal calf serum . | + 10% human serum . | + 10% human serum + mannan (5 mg/mL) . |
|---|---|---|---|---|
| L monocytogenes | ||||
| 3d-HSCs | 7.3%* (SD 1.2) | 8.4% (SD 0.6) | 12.0% (SD 1.0) | 12.7% (SD 2.3) |
| 5d-HSCs | 8.3%† (SD 0.6) | 13.7%† (SD 0.6) | 22.0% (SD 1.0) | 20.0% (SD 1.7) |
| 7d-HSCs | 1.6%† (SD 1.1) | 4.0%† (SD 2.5) | 26.0% (SD 2.6) | 27.0% (SD 2.0) |
| Y enterocolitica | ||||
| 3d-HSCs | 12.3% (SD 2.1) | 10.7% (SD 2.5) | 13.7% (SD 1.5) | 9.4%* (SD 2.1) |
| 5d-HSCs | 15.0%* (SD 1.0) | 15.7%* (SD 3.2) | 22.4% (SD 2.1) | 15.3%* (SD 0.6) |
| 7d-HSCs | 10.4%† (SD 1.5) | 14.3%† (SD 4.0) | 36.0% (SD 2.1) | 22.0%† (SD 2.9) |
| . | No additive . | + 10% fetal calf serum . | + 10% human serum . | + 10% human serum + mannan (5 mg/mL) . |
|---|---|---|---|---|
| L monocytogenes | ||||
| 3d-HSCs | 7.3%* (SD 1.2) | 8.4% (SD 0.6) | 12.0% (SD 1.0) | 12.7% (SD 2.3) |
| 5d-HSCs | 8.3%† (SD 0.6) | 13.7%† (SD 0.6) | 22.0% (SD 1.0) | 20.0% (SD 1.7) |
| 7d-HSCs | 1.6%† (SD 1.1) | 4.0%† (SD 2.5) | 26.0% (SD 2.6) | 27.0% (SD 2.0) |
| Y enterocolitica | ||||
| 3d-HSCs | 12.3% (SD 2.1) | 10.7% (SD 2.5) | 13.7% (SD 1.5) | 9.4%* (SD 2.1) |
| 5d-HSCs | 15.0%* (SD 1.0) | 15.7%* (SD 3.2) | 22.4% (SD 2.1) | 15.3%* (SD 0.6) |
| 7d-HSCs | 10.4%† (SD 1.5) | 14.3%† (SD 4.0) | 36.0% (SD 2.1) | 22.0%† (SD 2.9) |
The results from a representative experiment are presented as mean values and SDs of triplicate determination.
P < .05 and †P < .001 byt test.
Because the effect of human serum points to a role of immunoglobulins and the Fc receptor in the uptake of bacteria, we measured the expression of Fcγ receptors (CD16, CD32, and CD64) on human HSCs.
We could demonstrate pronounced up-regulation of CD32 on HSCs over the time course (Figure 8; 81% of 5d-HSCs were CD32+), whereas CD16 and CD64 up-regulation was less pronounced.
Flow cytometry of surface marker expression of FcγII receptor (CD32) on differentiating HSCs.
Black histograms represent expression of FcγII receptor (CD32). The x-axis of each histogram shows the log fluorescence intensity; the y-axis shows the relative cell number. Gray histograms represent staining with isotype-matched antibodies.
Flow cytometry of surface marker expression of FcγII receptor (CD32) on differentiating HSCs.
Black histograms represent expression of FcγII receptor (CD32). The x-axis of each histogram shows the log fluorescence intensity; the y-axis shows the relative cell number. Gray histograms represent staining with isotype-matched antibodies.
In comparison to L monocytogenes, internalization of Y enterocolitica by 7d-HSCs was influenced to a lesser degree by human serum (Table 1). The uptake of Y enterocolitica but not L monocytogenes is inhibited by yeast mannan, a competitive inhibitor of the mannose/fucose receptor. These results were corroborated by flow cytometry analysis of the surface expression of macrophage mannose receptor (CD206) on HSCs, which showed that differentiation toward monocytes led to up-regulation of the macrophage mannose receptor (Figure 9). Up to 10% of 7d-HSCs carried the receptor.
Expression of the macrophage mannose receptor CD206 on human HSCs.
The x-axis of dot plot shows the fluorescence intensity in a logarithmic scale. Forward scatter is on the y-axis.
Expression of the macrophage mannose receptor CD206 on human HSCs.
The x-axis of dot plot shows the fluorescence intensity in a logarithmic scale. Forward scatter is on the y-axis.
In addition, uptake of Y enterocolitica into HSCs could be inhibited by the addition of human serum fibronectin, which blocks the β1-integrin receptor (Figure10A). The β1-integrin receptors are present on quiescent and differentiated HSCs and do not parallel the switch from macropinocytosis to phagocytosis (Figure 10B).
Influence of β1-integrin receptor expression for the uptake of
Y enterocolitica by HSCs. (A) Comparison of the uptake of Y enterocolitica into 3d-, 5d-, and 7d-HSCs in the absence and presence of human fibronectin (*P < .05, t test). The results from a representative experiment are presented as mean values and SDs (error bars). (B) Flow cytometry of surface marker expression of β1-integrin CD29 on quiescent and 7d-HSCs (black histograms). The x-axis of each histogram shows the log fluorescence intensity; the y-axis shows the relative cell number. Gray histograms represent staining with isotype-matched antibodies.
Influence of β1-integrin receptor expression for the uptake of
Y enterocolitica by HSCs. (A) Comparison of the uptake of Y enterocolitica into 3d-, 5d-, and 7d-HSCs in the absence and presence of human fibronectin (*P < .05, t test). The results from a representative experiment are presented as mean values and SDs (error bars). (B) Flow cytometry of surface marker expression of β1-integrin CD29 on quiescent and 7d-HSCs (black histograms). The x-axis of each histogram shows the log fluorescence intensity; the y-axis shows the relative cell number. Gray histograms represent staining with isotype-matched antibodies.
The 5d- and 7d-HSCs did not show enhanced cell death after infection with L monocytogenes (propidium iodide staining revealed 5% to 6% dead cells either in uninfected 7d-HSCs or 6 hours after infection with L monocytogenes). In contrast, infection of 7d-HSCs with S typhimurium or Y enterocoliticaled to a significantly increased cell mortality 6 hours after infection (S typhimurium, 12% cell death; Y enterocolitica, 15% cell death), which is mainly caused by necrosis. Apoptotic cells, detected by chromatin condensation and cell blebbing after staining with Hoechst 33342, were rarely observed.
Discussion
The present study shows that quiescent CD34+ HSCs are completely resistant to infection with the tested bacteria. Our results are in accordance to the clinical observation that none of these pathogens leads to major alterations of hematopoiesis in patients.
L monocytogenes has been shown to invade a wide spectrum of differentiated phagocytic and nonphagocytic mammalian cells.4,20,21 In the latter, phagocytosis is supported by special bacterial surface proteins.8 It was recently shown that infection with S typhimurium and Y enterocolitica leads to efficient uptake of bacteria by myeloid cells, especially monocytes, macrophages, and dendritic cells.3,6 Phagocytes exhibit 3 types of endocytosis: macropinocytosis, phagocytosis, and clathrin-mediated endocytosis.5,6 They express several receptors that are involved in the internalization of bacteria including Fcγ/Fcε, macrophage mannose receptor, β1-integrin receptors, and complement receptors.6,7 22
In contrast to phagocytes, human quiescent HSCs are unable to perform macropinocytosis or receptor-mediated phagocytosis. In addition, bacterial uptake into HSCs could not be triggered by specific invasions of bacteria.8-10 Therefore, we conclude that in primitive HSCs essential receptors and internalization mechanisms are not developed yet. This is corroborated by the observation that the Fc-receptors CD16, CD32, and CD64 are expressed only discretely on quiescent HSCs.
Subsequent differentiation of HSCs into CD14+ monocytelike progenitor cells enables them to internalize bacteria and also heat-killed bacteria and latex beads efficiently, indicating that these cells have acquired a general uptake apparatus that is apparently not present in quiescent HSCs. The uptake of bacteria and latex beads into 3d- and 5d-HSCs was significantly reduced by inhibitors of macropinocytosis. This is paralleled by an increased uptake of lucifer yellow in developing HSCs. Therefore, we suggest that macropinocytosis is an important uptake mechanism in 3d- and 5d-HSCs.
Human serum, but not fetal calf serum, significantly stimulated the efficiency of listerial uptake by 7d-HSCs. These results suggest that uptake mechanisms for bacteria develop stepwise. First, macropinocytosis becomes active as demonstrated by lucifer yellow accumulation and by inhibition of the uptake of latex beads, L monocytogenes, S typhimurium, and Y enterocolitica by inhibitors of macropinocytosis. At a later stage of differentiation (> 5d-HSCs) opsonophagocytosis is induced and bacteria are internalized by phagocytosis mediated by Fc receptor or complement receptor, mannose/fucose receptor, and β1-integrin receptor. In previous studies,6 we have shown that uptake of L monocytogenes by human monocyte-derived dendritic cells is enhanced by human serum, apparently caused by antibodies against listerial p60 antigen present in most human sera. Opsonization of Listeria organisms by these antibodies then leads to Fc receptor–mediated uptake. It is likely that a similar mechanism may also be responsible for serum-stimulated L monocytogenesinternalization by 7d-HSCs. This assumption is consistent with the observed up-regulation of Fc receptors (CD32) in developing HSCs. The internalization of Y enterocolitica by developing HSCs is inhibited by yeast mannan, a competitive inhibitor of the mannose/fucose receptor, demonstrating a role of this receptor for the cellular uptake of these bacteria. Mannose is a major component of the O-antigen of Y enterocolitica,23 which may be responsible for the interaction of Y enterocolitica with the mannose receptor. This is consistent with the observed expression of macrophage mannose receptor on monocyte precursors.
In addition, Yersinia promote bacterial penetration into mammalian cells by binding to several β1-chain integrins via an invasin protein.7 Fibronectin binds to β1-integrins at the same overlapping sites. Blocking of β1-intergrin receptors with human fibronectin reduced the uptake of Y enterocolitica into differentiating HSCs. This is why we suppose that Yersinia invasin protein binds to β1-intergrin and that this interaction contributes to bacterial entry into differentiating HSCs. Interestingly, we could show expression of the β1-integrin already on quiescent HSCs. Nevertheless this receptor could not be used by quiescent HSCs, because we did not observe bacterial uptake in this stage. One may speculate that aside from the receptor the general uptake apparatus is missing in quiescent HSCs.
According to our data, we believe that in other tissue-specific adult stem cells uptake mechanisms for bacteria may also develop gradually during differentiation, suggesting a similar resistance of these stem cells to infection with pathogenic bacteria.
Another interesting aspect of this investigation is the high viability of 5d-HSCs after internalization of bacterial pathogens, which is in contrast to the rapid apoptosis or necrosis of completely differentiated monocytes and macrophages observed especially after the infection with S typhimurium or Y enterocolitica.3,14,15 This remarkable survival rate together with the high bacterial uptake by 5d-HSCs assigns this cell population to be better applicable for the introduction of plasmid DNA via virulence-attenuated L monocytogenes24,25 or S typhimurium26 strains in comparison to completely differentiated cells presently used for this purpose. This possibility is currently being investigated in our laboratory.
The authors thank R. Ottohal for excellent technical assistance. We are grateful to Prof J. Heesemann for donating the Yersinia enterocolitica strain. We thank Prof G. Krohne and C. Gehrig for helping with electron microscopy. We are indebted to Drs M. Mäurer and B. Joseph for critical reading of the manuscript.
Prepublished online as Blood First Edition Paper, July 18, 2002; DOI 10.1182/blood-2002-03-0898.
Supported by a fellowship from the Bayerischen Staatsministerium für Wissenschaft, Forschung und Kunst to A.K.-M. and by grants from the Deutsche Forschungsgemeinschaft (SFB 479) and the Fonds der Chemischen Industrie.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Annette Kolb-Mäurer, Department of Dermatology, Josef-Schneider-Str 2, D-97080 Würzburg, Germany; e-mail: ankolb@biozentrum.uni-wuerzburg.de.






This feature is available to Subscribers Only
Sign In or Create an Account Close Modal