Granulocyte colony–stimulating factor (G-CSF) may affect T-cell homeostasis by multiple mechanisms, inducing polarization of cytokine secretion, inhibition of T-cell proliferation, and enhancement of T-cell apoptosis. We analyzed the production of interleukin-10 (IL-10) and transforming growth factor-β1 (TGF-β1) by T cells from healthy volunteer donors treated with recombinant human G-CSF. Highly purified CD4+ T cells obtained before and after G-CSF administration (pre-G and post-G, respectively) were activated using the allogeneic mixed leukocyte reaction. Post-G CD4+T cells produced high levels of IL-10 but undetectable levels of IL-2 and IL-4, whereas the level of TGF-β1 release was comparable to that of pre-G CD4+ T cells. Notably, post-G CD4+ T cells proliferated poorly in response to alloantigens and to recall antigens and suppressed the proliferation of autologous CD4+ T cells in a cell contact–independent and an antigen-nonspecific manner. TGF-β1 and IL-10 were not dispensable for post-G CD4+ T cells to mediate suppression, as shown by neutralization studies. Compared with pre-G CD4+ T cells, alloantigen-activated post-G CD4+ T cells preferentially expressed markers associated with memory T cells, in conjunction with reduced levels of CD28 and CD62L. Collectively, these data demonstrate that CD4+ T cells exposed to G-CSF in vivo acquire the properties of T regulatory (Tr) cells once triggered in vitro through the T-cell receptor, including a peculiar cytokine production profile (IL-10++TGF-β1+IL-2low/−IL-4low/−), an intrinsic low proliferative capacity, and a contact-independent suppression of antigen-driven proliferation. Tr cells generated ex vivo after exposure to G-CSF might be clinically relevant for transplantation medicine and for the treatment of human immune-mediated diseases.
Introduction
Hematopoietic stem cells (HSCs) circulate in the peripheral blood, and clinical provision of cytokines such as granulocyte-colony–stimulating factor (G-CSF) alone or along with cytoreductive chemotherapy has the ability to increase dramatically HSC frequency.1 HSC transplantation (HSCT) has become a powerful strategy for the treatment of leukemia, aplastic anemia, congenital immunodeficiencies, hemoglobin disorders, and autoimmune and degenerative diseases.2 In particular, allogeneic HSCs may be useful for cancer treatment and in a nonmalignant clinical setting and might lead to donor-specific chimerism for inducing lifelong tolerance to tissue or organ transplantation.2
To date, results of allogeneic peripheral blood HSCT for hematologic malignancies suggest that this technique has potential advantages over conventional bone marrow transplantation1 given that hematopoietic engraftment might be more prompt because of the infusion of so-called facilitator T cells, and the antileukemic effect of T cells contained within the graft may be enhanced. Although T-cell dose in peripheral blood HSC allografts is markedly higher than in bone marrow allografts, the level of acute graft-versus-host disease (GVHD) has been tolerable.1 Several explanations for this phenomenon have been proposed, including functional alteration of T cells in G-CSF–mobilized allografts. Support for this hypothesis stems from recent studies in mice and in humans. New properties of G-CSF as a modulator of the immune response have been postulated, for example, in indirect actions on T-cell function through bystander cells, endogenous mediators, or effects on bone marrow lymphoid precursors.3-6
The impact of G-CSF on cytokine secretion by human T cells remains controversial. Some studies describe the polarization of T-cell responses toward a helper T cell type 2 (TH2) functional profile, and others document the inhibition of helper T cell type 1 (TH1) and TH2 cytokine production.7,8 Previously, we demonstrated that G-CSF can inhibit T-cell proliferation in response to polyclonal mitogens by modulating the expression of key components of the cell cycle machinery at the G1-S transition9,10; furthermore, soluble inhibitory factors elicited by G-CSF can favor the execution of T-cell apoptosis through increased bax expression, collapse of mitochondrial transmembrane potential, caspase-3 cleavage, and DNA fragmentation.11
Protective immunity to foreign antigens and control of autoaggressive immune reactions are ensured by T regulatory (Tr) cells.12Tr cells have been described in a variety of experimental systems and have the ability to protect from autoimmune diseases,12inflammatory bowel disease,13 allograft rejection, and cyclosporin A–induced autologous GVHD.14 Specifically, Tr cells with high interleukin-10 (IL-10) or transforming growth factor-β1 (TGF-β1) and low or undetectable IL-2 or IL-4 release were designated Tr type 1 (Tr1) cells.13 TGF-β1 and IL-10 are known to regulate T-cell homeostasis; in particular, TGF-β1 protects T cells from apoptosis and is a general suppressor of cytokine production,15,16 whereas IL-10 promotes cell cycle arrest mainly by inhibiting IL-2 production and CD28 costimulation.17,18 Tr1 cells proliferate poorly, and their suppressive activities against bystander T cells—for example, the inhibition of antigen-specific and antigen-nonspecific proliferation—are partly dependent on the concerted action of TGF-β1 and IL-10.12 Notably, Tr cells can induce naive CD4+ T cells to differentiate into Tr cells, a phenomenon termed infectious tolerance.12 Alloantigen challenge of human CD4+ T cells in vitro in the presence of IL-10 also induces T-cell anergy, and, after repetitive stimulations, a population of Tr cells emerges that secretes high amounts of IL-10 and moderate amounts of TGF-β1.13 Importantly, CD4+ T cells with regulatory activity have been shown to suppress graft rejection in several transplantation models, and it has been demonstrated that CD4+ T cells anergized by combined treatment with IL-10 and TGF-β1 remain tolerant to alloantigens and prevent GVHD lethality after transfer to major histocompatibility complex (MHC) class 2 disparate recipients.19 20
Herein we report that highly purified CD4+ T cells from healthy HSC donors receiving G-CSF acquire the functional properties of Tr cells after activation with alloantigens and secrete high amounts of IL-10 and moderate amounts of TGF-β1 in the absence of significant IL-2 or IL-4 release. Furthermore, we have learned that these alloactivated CD4+ Tr cells have a peculiar cell-surface antigen profile, an intrinsically impaired proliferative capacity, and the ability to mediate active suppression of antigen-driven proliferation primarily by a cell-contact–independent mechanism.
Patients, materials, and methods
Characteristics of HSC donors
Six healthy donors (3 men, 3 women; median age, 36 years) received 16 μg/kg per day G-CSF (Granocyte; Aventis Pharma, Milan, Italy) subcutaneously for 5 days to mobilize HSCs into the peripheral blood for transplantation into HLA-matched allogeneic recipients. All donors gave their informed consent, and the investigations were approved by the Institutional Human Research Committee. Peripheral blood samples were obtained before G-CSF (pre-G) and on day 4 of cytokine administration (post-G), when donors underwent leukophoretic collection of circulating HSCs, as detailed elsewhere.9
T-cell isolation and stimulation
Peripheral blood mononuclear cells (PBMCs) were separated by the Ficoll-Hypaque density-gradient method, as reported.11Adherent cells were removed by incubation on tissue-culture–treated flasks for 1 hour at 37°C, and CD4+ T cells were purified by positive selection (CD4 MACS MultiSort beads; Miltenyi Biotec, Bergische Gladbach, Germany). After detachment, cells were washed with phosphate-buffered saline (PBS) supplemented with 1% human serum albumin; CD4+ T-cell purity as assessed by fluorescence-activated cell sorter (FACS) analysis ranged from 94% to 96%. CD4+ T cells were stimulated in an antigen-specific manner with the mixed-leukocyte reaction (MLR). Briefly, 5 × 104 pre-G or post-G CD4+ T cells (MLRCD4+ T cells) were seeded with irradiated (25 Gy) allogeneic T-cell–depleted (TCD) PBMCs (5 × 105) as accessory cells and were cultured for 7 days at a stimulator-responder ratio of 1:3. Because serum contains significant amounts of latent TGF-β, all experiments were performed under serum-free conditions (10% BIT HCC-9500 serum substitute; StemCell Technologies, Vancouver, BC, Canada). TGF-β1 (1 ng/mL), IL-12 (2 IU/mL), IL-2 (10 IU/mL), or IL-15 (20 ng/mL) (all purchased from R&D Systems, Oxon, Cambridge, United Kingdom) was added to the MLR, as indicated in the figure legends.
Transwell experiments
Coculture experiments were performed with Transwell systems (MilliCell inserts, 0.4 μM; Millipore, Watford, United Kingdom) for the assessment of regulatory properties of post-GMLRCD4+ T cells against nonregulatory autologous pre-G MLRCD4+ T cells (indicator CD4+ T cells). Both chambers of each Transwell received irradiated allogeneic TCD PBMCs as stimulator cells. The proliferation of indicator CD4+ T cells plated in the lower chamber was monitored in the absence of direct contact with 5 × 105 post-G MLRCD4+T cells from the same HSC donor, placed in the upper compartment of the Transwell (primary cocultures). In selected coculture experiments, neutralizing anti–TGF-β1 (20 ng/mL) or anti–IL-10 antibodies (10 μg/mL; both from R&D Systems) were added as indicated in the figure legends. After 7 days, the basket was removed and proliferation of autologous indicator CD4+ T cells was measured, as will be detailed.
Antigen specificity of suppression mediated by post-GMLRCD4+ T cells was assessed in secondary cocultures. Briefly, pre-G CD4+ T cells were stimulated with allogeneic TCD PBMC from different donors (donor A or donor B). Seven days later, these donor A– or donor B–specific indicator CD4+ T cells were restimulated with allogeneic TCD PBMCs from donor A or donor B, separated through Transwell chambers by suppressor post-G CD4+ T cells. The proliferation of indicator CD4+ T cells was estimated, as will be described.
Immunologic markers
Expression of informative activation–differentiation antigens and that of receptors for representative CC and CXC subfamilies of chemokines was investigated by flow cytometry. Briefly, aliquots ofMLRCD4+ T cells were incubated for 20 minutes at 4°C with pretitrated amounts of the following fluorescein isothiocyanate (FITC)– or phycoerythrin (PE)-conjugated monoclonal antibodies (mAbs): CD45RA (L48 clone, immunoglobulin G1[IgG1]), CD45RO (UCHL-1 clone, IgG1), CD25 (2A3 clone, IgG1), CD40L (CD154; 89-76 clone, IgG1), CD44 (L178 clone, IgG1; Becton Dickinson, Mountain View, CA), CD122 (IL-2 receptor β-chain [IL-2R β-chain]; Mik–β3 clone, IgG1), CD132 (IL-2R γ-chain; AG184 clone, IgG1), CD45RB (MT4 clone, IgG1), CXCR3 (CD183; 1C6 clone, IgG1), CXCR4 (CD184; 12G5 clone, IgG2a), CCR5 (CD195; 2D7 clone, IgG2a), CCR6 (11A9 clone, IgG1), CCR7 (CDw197; 2H4 clone; IgM; PharMingen, San Diego, CA), CD28 (15E8 clone, IgG1), CD62L (DREG-56 clone, IgG1), CD95 (DX2 clone, IgG1), CD95L (CD178; ALF-2.1 clone, IgG2a), CD38 (HIT2 clone, IgG1; Caltag Laboratories, Burlingame, CA) or with the appropriate fluorochrome-conjugated, isotype-matched irrelevant mAbs to establish background fluorescence. Cells labeled with the primary unconjugated anti-CCR7 mAb were further incubated with FITC-conjugated goat–anti-mouse mAb (Caltag Laboratories) for 30 minutes at 4°C. After washings with PBS, cells were kept on ice until flow cytometric analysis.
Analysis of cytokine production
The frequency of cytokine-producing CD4+ T cells was evaluated as previously described.21 Briefly,MLRCD4+ T cells were exposed to a protein transport inhibitor (1 μg/mL Brefeldin A; Sigma Chemical, St Louis, MO) during the last 4 hours of culture. Cells were then fixed with 1% paraformaldehyde for 15 minutes at room temperature, and underwent permeabilization with 0.01% saponin and incubation with FITC- or PE-conjugated anti–interferon (IFN)-γ mAb (NIB42 clone, IgG1; Becton Dickinson), anti–IL-10 mAb (B-N10 clone, IgG2b; Valter Occhiena, Turin, Italy), or anti–IL-4 mAb (8D4-8 clone, IgG1; Becton Dickinson) or with unconjugated anti–TGF-β1 rabbit polyclonal antibodies (Santa Cruz Biotechnology, CA) for 30 minutes at 4°C. After washings with PBS, FITC-conjugated goat–anti-rabbit antibodies (Caltag Laboratories) were added to CD4+ T cells stained with the primary unconjugated anti–TGF-β1 antibody, and these CD4+ T cells were further incubated for 30 minutes at 4°C before flow cytometric analysis. Recombinant cytokines (all from R&D Systems) were always included to control for the specificity of mAb binding.
Cytokine synthesis was evaluated by the analysis of supernatants 7 days after alloantigen stimulation. IL-2, IL-4, IL-10, and TGF-β1 levels were quantified by ELISA (R&D Systems) and were further validated using the Bio-Plex Protein Array System (Bio-Rad Laboratories, Hercules, CA).22 To activate latent TGF-β1 to the immunoreactive form, 500 μL cell-free supernatants were preincubated with 1 N HCl, followed by neutralization with 1.2 N NaOH in 0.5 M HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid) buffer. Limits of detection were as follows: 0.5 pg/mL IL-10 (Ultra Quantikine HS; R&D Systems); 7 pg/mL TGF-β1; and 10 pg/mL IL-2 and IL-4. Calculations of cytokine levels in a typical multiplex experiment were performed with the Bio-Plex Manager 2.0 software (Biorad Laboratories, Milan, Italy) using a 5-PL regression equation.
Generation of dendritic cells for autologous MLR
PBMCs were seeded at 0.5 × 107/mL into 6-well culture plates containing AIM-V (Invitrogen, Carlsbad, CA) supplemented with 0.5% human serum albumin. After 2 hours at 37°C, nonadherent cells were removed, and adherent cells were cultured at 37°C in a humidified 6% CO2–95% air incubator in the presence of recombinant human granulocyte macrophage (GM)–CSF (800 IU/mL) and IL-4 (500 IU/mL; both from R&D Systems). After 7 days of culture, tumor necrosis factor-α (TNF-α) (R&D Systems) was added at 1000 IU/mL to induce dendritic cell (DC) maturation.23Pre-G indicator CD4+ T cells were cultured with irradiated (25 Gy) DCs at a 1:3 stimulator-responder ratio in the lower chamber of a Transwell system, separated by post-G CD4+ T cells in the upper compartment of the Transwell. To test for antigen-specific T-cell responses, cultures were performed in the presence of a recall antigen (purified protein derivative of Mycobacterium tuberculosis[PPD]; 20 μg/mL final concentration; Staten Serum Institute, Copenhagen, Denmark). During the last 24 hours of culture, pre-G indicator CD4+ T cells were pulsed with bromodeoxyuridine (BrdUrd), and proliferation was evaluated as detailed below. Cocultures of indicator CD4+ T cells and DCs not pulsed with PPD were always included to control for the antigen dependency of the response.
Proliferation assays and cell cycle analysis
During the last 24 hours of the MLR, cells were pulsed with 25 μM BrdUrd (Sigma Chemical); cultures were stopped, and cells were fixed with ice-cold 70% ethanol.10 After partial DNA denaturation with 3 N HCl containing 0.5% Tween-20, cells were incubated for 30 minutes at 4°C with FITC-conjugated anti-BrdUrd mAb (BR-3 clone, IgG1; Caltag Laboratories) or with isotype-matched irrelevant mAbs to establish background fluorescence; cells not exposed to BrdUrd were used to evaluate the specificity of the anti-BrdUrd staining. Cellular DNA content was measured by resuspending the BrdUrd-labeled cells in DNA staining buffer (5 μg/mL propidium iodide, 2 mg/mL RNase; Sigma Chemical) before flow cytometric analysis.
Messenger RNA detection
RNA was isolated with the RNeasy minikit (Qiagen, Hilden, Germany) and was reverse-transcribed with 25 U Moloney murine leukemia virus reverse transcriptase (RT; Perkin Elmer Cetus, San Diego, CA) at 42°C for 30 minutes in the presence of random hexamers. Two microliters cDNA product was amplified with 1 U Amplitaq Gold (Perkin Elmer) in the presence of primers specific for the gene of interest, together with primers specific for the housekeeping gene aldolase-A. The ratio between the sample RNA to be determined and aldolase-A was calculated to normalize for initial variations in sample concentration and as a control for reaction efficiency, as reported.24 Reverse transcription–polymerase chain reaction (RT-PCR) was performed using the following oligonucleotides: GATA-3 forward, TAAACGAGCTGTTCTTGGGG; GATA-3 reverse, GTCCTGTGCGAACTGTCAGA; aldolase-A forward, CGCAGAAGGGGTCCTGGTGA; aldolase-A reverse, CAGCTCCTTCTTCTGCTCCGGGGT (Pharmacia Biotech, Uppsala, Sweden). Band intensity was quantified with Photoretix 1D (Photoretix International, Newcastle-upon-Tyne, United Kingdom) and was expressed as relative absorbance units.24
Flow cytometry and immunofluorescence analysis
Samples were run through a FACScan flow cytometer (Becton Dickinson) equipped with an argon laser emitting at 488 nm. The fluorescence of FITC was recorded in FL1 (525 nm), and the fluorescence of PE and propidium iodide was recorded in FL2 (575 nm), after suitable electronic compensation. A minimum of 10 000 events was acquired in list mode using CellQuest software. Details on instrument settings and requirements are published elsewhere.11 25
Statistical analysis
The approximation of population distribution to normality was tested using statistics for kurtosis and symmetry. Results were asymmetrically distributed and, consequently, were presented as median values and ranges. All comparisons were performed with the Wilcoxon W test for paired determinations or the Mann-Whitney U test for unpaired data, as appropriate. The criterion for statistical significance was defined as P ≤ .05.
Results
Cytokine production by MLRCD4+T cells
To provide a quantitative measure of the cytokine-producing ability of T cells after their exposure to G-CSF, pre-G and post-G CD4+ T cells from the same HSC donor were challenged with irradiated TCD PBMCs from an unrelated healthy volunteer. Alloantigen-activated post-G MLRCD4+T cells showed a general suppression of cytokine production; the frequency of cells expressing intracellular IL-2 and IL-4 was significantly lower than that of pre-GMLRCD4+ T cells (Table1). Similarly, IFN-γ production by post-G MLRCD4+ T cells was decreased (data not shown). When the percentage of CD4+ T cells releasing IL-10 and TGF-β1 was evaluated, a significant increase in the frequency of post-GMLRCD4+ T cells expressing intracellular IL-10 was found; conversely, the frequency of post-GMLRCD4+ T cells reactive with the anti–TGF-β1 mAb was unchanged compared with pre-GMLRCD4+ T cells (Table 1). Thus, only a small proportion of post-G MLRCD4+T cells had a Tr1-like cytokine production profile (IL-10++TGF-β1+IL-2low/−IL-4low/−) as judged by the flow cytometric analysis at the single-cell level.
Cytokine production byMLRCD4+ T cells
| Stimuli . | Cells . | IL-2 . | IL-4 . | IL-10 . | TGF-β1 . |
|---|---|---|---|---|---|
| Allogeneic TCD PBMCs | Pre-G CD4+ | 30 (22-38)* | < 10* | 80 (40-190)* | 3800 (3430-4500)* |
| 6% (3%-7%)† | 2% (1%-2.5%)† | 2% (1.5%-3.5%)† | 6% (4%-7%)† | ||
| Allogeneic TCD PBMCs | Post-G CD4+ | < 10*,‡ | < 10* | 178 (90-250)*,‡ | 3040 (2200-4075)* |
| < 1%†,‡ | < 1%†,‡ | 12% (8%-18%)†,‡ | 5% (4%-8%)† |
| Stimuli . | Cells . | IL-2 . | IL-4 . | IL-10 . | TGF-β1 . |
|---|---|---|---|---|---|
| Allogeneic TCD PBMCs | Pre-G CD4+ | 30 (22-38)* | < 10* | 80 (40-190)* | 3800 (3430-4500)* |
| 6% (3%-7%)† | 2% (1%-2.5%)† | 2% (1.5%-3.5%)† | 6% (4%-7%)† | ||
| Allogeneic TCD PBMCs | Post-G CD4+ | < 10*,‡ | < 10* | 178 (90-250)*,‡ | 3040 (2200-4075)* |
| < 1%†,‡ | < 1%†,‡ | 12% (8%-18%)†,‡ | 5% (4%-8%)† |
Ranges appear in parentheses.
Pre-G and post-G CD4+ T cells from the same donor were activated with allogeneic TCD PBMCs for 7 days in MLR at a 1:3 stimulator-responder ratio. After culture, IL-2, IL-4, IL-10, and TGF-β1 levels were measured by ELISA in culture supernatants, whereas the frequency of cytokine-producing CD4+ T cells was determined by flow cytometry after short-term exposure to a protein transport inhibitor (see “Patients, materials, and methods”). Binding specificities of the anticytokine mAb were established by adding recombinant cytokines before mAb staining (data not shown). All determinations were performed in triplicate. Data were reported as median values and ranges and are representative of 6 independent experiments.
pg/mL.
Percentage positive cells.
P < .05 compared with pre-GMLRCD4+ T cells.
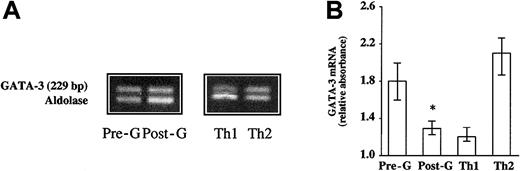
Cytokine release in culture supernatants was next evaluated using sensitive and specific enzyme-linked immunosorbent assay (ELISA). As shown in Table 1, post-G MLRCD4+ T cells produced higher amounts of IL-10 than did pre-GMLRCD4+ T cells; furthermore, significant levels of TGF-β1 were detected. Marginal synthesis of IL-2 and IL-4 could be measured in post-GMLRCD4+ T-cell cultures. Tested cytokines were unlikely to arise from exogenous sources because all experiments were performed under serum-free conditions; rather, cytokines were derived from T cells themselves. In addition, no cytokine production could be detected in control cultures containing irradiated stimulator TCD PBMCs only (data not shown). The combined analysis of cytokine levels in bulk cultures and the frequency of cytokine-producing CD4+ T cells suggested that alloantigen-activated post-G MLRCD4+T cells were neither genuine TH1 nor TH2 cells but, rather, acquired a cytokine production profile that was reminiscent of the Tr1 cells described in animal models and in humans.26 This finding was backed by molecular analyses showing that mRNA signals for the TH2-inducing transcription factor GATA-3 were down-regulated in post-GMLRCD4+ T cells compared with the reciprocal pre-G MLRCD4+ T-cell population but that they were similar to those of TH1 clones differentiated in the presence of IL-12 and neutralizing anti–IL-4 antibodies (Figure 1). In contrast, TH2 clones generated in the presence of IL-4 and neutralizing mAb directed against IL-12 expressed remarkable amounts of GATA-3 mRNA (Figure 1).
Measurement of mRNA signals for GATA-3 by RT-PCR.
Pre-G or post-G CD4+ T cells from the same donor were activated with allogeneic TCD PBMCs for 7 days in MLR at a 1:3 stimulator-responder ratio. (A) A representative experiment is shown. TH1 and TH2 clones were established after phytohemagglutinin activation of normal peripheral blood T cells in the presence of IL-12 (5 ng/mL) plus anti–IL-4 antibodies (200 ng/mL; TH1-promoting condition) or IL-4 (200 IU/mL) plus anti–IL-12 antibodies (10 μg/mL; TH2-promoting condition). (B) Error bars represent median values and ranges recorded in 6 independent experiments; band intensity was expressed as absorbance units relative to the housekeeping gene aldolase. *P < .05 compared with pre-GMLRCD4+ T cells.
Measurement of mRNA signals for GATA-3 by RT-PCR.
Pre-G or post-G CD4+ T cells from the same donor were activated with allogeneic TCD PBMCs for 7 days in MLR at a 1:3 stimulator-responder ratio. (A) A representative experiment is shown. TH1 and TH2 clones were established after phytohemagglutinin activation of normal peripheral blood T cells in the presence of IL-12 (5 ng/mL) plus anti–IL-4 antibodies (200 ng/mL; TH1-promoting condition) or IL-4 (200 IU/mL) plus anti–IL-12 antibodies (10 μg/mL; TH2-promoting condition). (B) Error bars represent median values and ranges recorded in 6 independent experiments; band intensity was expressed as absorbance units relative to the housekeeping gene aldolase. *P < .05 compared with pre-GMLRCD4+ T cells.
Cell surface phenotype of MLRCD4+T cells
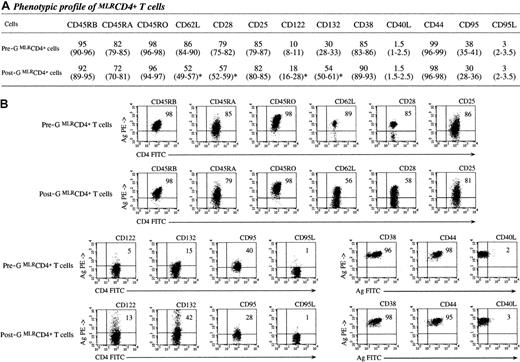
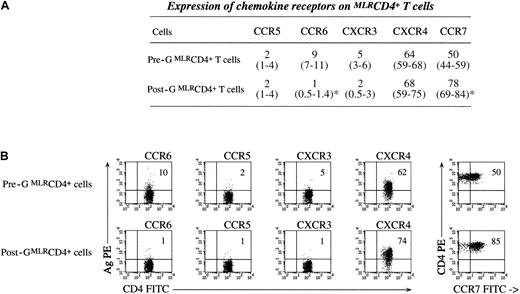
Next, post-G MLRCD4+ T cells were analyzed for the expression of informative activation–differentiation antigens; levels of surface antigen expression were compared with those of pre-GMLRCD4+ T cells. No differences were found between freshly isolated pre-G and post-G CD4+ T cells for the expression pattern of the cell-surface antigens detailed in “Patients, materials, and methods” (data not shown), thus confirming results of previous studies.9 In particular, the percentage of CD4+ T cells constitutively expressing CD25 was not significantly different between peripheral blood pre-G and post-G cells (12% [range, 7%-15%] vs 11% [range, 8%-12%], respectively). Conversely, alloantigen-activated post-G CD4+ T cells showed unique phenotypic features. The activation–costimulatory molecules CD62L and CD28 were detected on lower percentages of post-G than of pre-GMLRCD4+ T cells (Figure2). Post-GMLRCD4+ T cells expressed the highest frequency and intensity of the IL-2R β-chain (CD122) and γ-chain (CD132); in contrast, the inducible expression of the IL-2R α-chain (CD25) was comparable on pre-G and post-GMLRCD4+ T cells (Figure 2). CD45RA and CD45RO antigens, considered as markers of naive and memory cells, respectively, were found at comparable levels in pre-G and post-GMLRCD4+ T cells, as were CD45RB expression pattern and CD95, CD95L, and CD40L levels (Figure 2). Finally, post-G MLRCD4+ T cells expressed high levels of CCR7 and CXCR4 chemokine receptors (Figure3). Whereas CXCR3 and CCR5 receptors were detected on marginal proportions of pre-G and post-GMLRCD4+ T cells, a distinct subset ofMLRCD4+ T cells staining positively with the anti-CCR6 mAb could be resolved only in pre-GMLRCD4+ T-cell cultures. Collectively, these experiments showed that post-GMLRCD4+ T cells preferentially expressed markers characteristic of activated–memory T cells, in conjunction with reduced levels of the costimulatory molecule CD28.
Phenotypic profile ofMLRCD4+ T cells.
Pre-G or post-G CD4+ T cells from the same donor were activated with allogeneic TCD PBMCs for 7 days in MLR at a 1:3 stimulator-responder ratio. The expression of informative activation–differentiation antigens was then evaluated with multicolor flow cytometry. (A) Median values and ranges recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells. (B) A representative set of experiments is depicted. Markers were set according to the proper isotypic control, and the percentage of CD4+ T cells expressing a given antigen is indicated in the upper right quadrant of each bidimensional cytogram.
Phenotypic profile ofMLRCD4+ T cells.
Pre-G or post-G CD4+ T cells from the same donor were activated with allogeneic TCD PBMCs for 7 days in MLR at a 1:3 stimulator-responder ratio. The expression of informative activation–differentiation antigens was then evaluated with multicolor flow cytometry. (A) Median values and ranges recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells. (B) A representative set of experiments is depicted. Markers were set according to the proper isotypic control, and the percentage of CD4+ T cells expressing a given antigen is indicated in the upper right quadrant of each bidimensional cytogram.
Expression of chemokine receptors onMLRCD4+ T cells.
Pre-G or post-G CD4+ T cells from the same donor were activated with allogeneic TCD PBMCs for 7 days in MLR at a 1:3 stimulator-responder ratio. The expression of informative chemokine receptors was then evaluated with multicolor flow cytometry. (A) Median values and ranges recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells. (B) A representative set of experiments is depicted. Markers were set according to the proper isotypic control, and the percentage of CD4+ T cells expressing a given antigen is indicated in the upper right quadrant of each bidimensional cytogram.
Expression of chemokine receptors onMLRCD4+ T cells.
Pre-G or post-G CD4+ T cells from the same donor were activated with allogeneic TCD PBMCs for 7 days in MLR at a 1:3 stimulator-responder ratio. The expression of informative chemokine receptors was then evaluated with multicolor flow cytometry. (A) Median values and ranges recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells. (B) A representative set of experiments is depicted. Markers were set according to the proper isotypic control, and the percentage of CD4+ T cells expressing a given antigen is indicated in the upper right quadrant of each bidimensional cytogram.
Proliferation of MLRCD4+ T cells
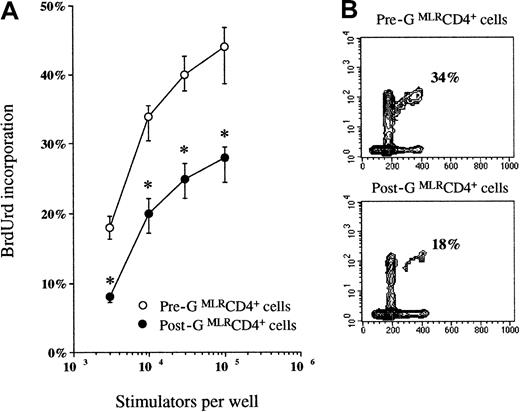
Because Tr1 cells have an intrinsically low ability to proliferate in response to antigen activation,13 experiments were conducted to determine whether the functional polarization of post-GMLRCD4+ T cells to a Tr1-like profile was associated with inhibited proliferation. In line with previously published data,10 the frequency of post-GMLRCD4+ T cells incorporating BrdUrd, in response to stimulation through the T-cell receptor (TCR) for antigen, was significantly lower than T-cell responses in the same donor before G-CSF was given (Figure4).
Proliferation ofMLRCD4+ T cells.
Pre-G or post-G CD4+ T cells from the same donor were activated with allogeneic TCD PBMCs for 7 days in MLR at a 1:3 stimulator-responder ratio. Proliferation was determined after 7 days of culture by the addition of BrdUrd for the final 24 hours. Proliferation of pre-G or post-G CD4+ T cells in the absence of stimulator cells never exceeded 5% (data not shown). (A) Median values and ranges recorded in 6 independent experiments are plotted. *P < .05 compared with pre-GMLRCD4+ T cells. (B) A representative experiment is shown. Percentage of cells incorporating BrdUrd has been indicated.
Proliferation ofMLRCD4+ T cells.
Pre-G or post-G CD4+ T cells from the same donor were activated with allogeneic TCD PBMCs for 7 days in MLR at a 1:3 stimulator-responder ratio. Proliferation was determined after 7 days of culture by the addition of BrdUrd for the final 24 hours. Proliferation of pre-G or post-G CD4+ T cells in the absence of stimulator cells never exceeded 5% (data not shown). (A) Median values and ranges recorded in 6 independent experiments are plotted. *P < .05 compared with pre-GMLRCD4+ T cells. (B) A representative experiment is shown. Percentage of cells incorporating BrdUrd has been indicated.
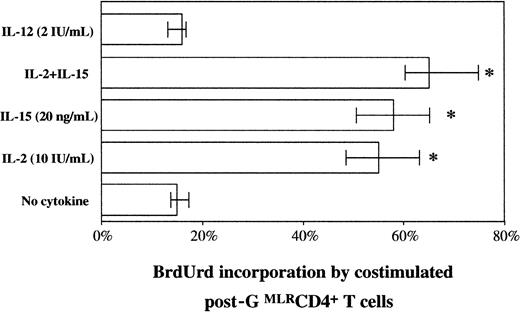
Defective production of the TH1-promoting cytokine IL-12 by antigen-presenting cells has been advocated as a potential mechanism of suppression of T-cell function by G-CSF.27 With these findings in mind, we provided exogenous IL-12 to hyporesponsive post-GMLRCD4+ T cells and measured T-cell proliferation after 4 days of culture. Unexpectedly, IL-12 was incapable of restoring post-G MLRCD4+T-cell proliferation to the levels recorded in pre-GMLRCD4+ T cells (Figure5). Conversely, high levels of bystander proliferation were found in post-GMLRCD4+ T cells after their exposure to IL-2, IL-15, or both (Figure 5), approaching proliferative responses of similarly costimulated pre-GMLRCD4+ T cells (data not shown).
Effect of costimulatory cytokines on the proliferation of post-G MLRCD4+ T cells.
After 7 days of culture, post-GMLRCD4+ T cells were removed from the MLR, rested for 24 hours, and cultured in the presence of exogenously added cytokines or with culture medium alone for an additional 4 days. Bystander proliferation was quantified after the provision of BrdUrd for the final 24 hours. *P < .05 compared with post-GMLRCD4+ T cells cultured in the absence of cytokines.
Effect of costimulatory cytokines on the proliferation of post-G MLRCD4+ T cells.
After 7 days of culture, post-GMLRCD4+ T cells were removed from the MLR, rested for 24 hours, and cultured in the presence of exogenously added cytokines or with culture medium alone for an additional 4 days. Bystander proliferation was quantified after the provision of BrdUrd for the final 24 hours. *P < .05 compared with post-GMLRCD4+ T cells cultured in the absence of cytokines.
Post-G MLRCD4+ T cells suppress the alloproliferative response of autologous T cells in a cell-contact–independent and an antigen-nonspecific manner
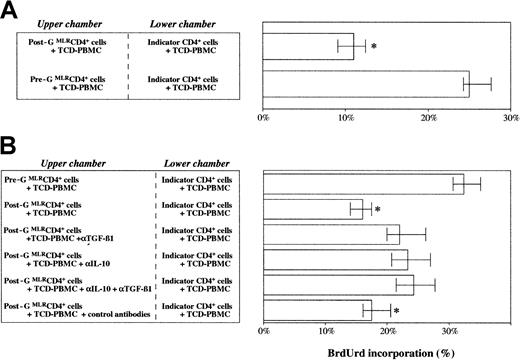
We then analyzed the regulatory properties of post-GMLRCD4+ T cells. To this purpose, freshly isolated post-G CD4+ T cells were immediately cocultured with pre-G CD4+ T cells from the same donor (primary coculture), or they were first separately activated and such prestimulated CD4+ T cells were used for secondary cocultures. As shown in Figure 6A, post-GMLRCD4+ T cells inhibited the alloreactivity of indicator CD4+ T cells in primary coculture, suggesting that cell–cell contact was dispensable for the regulatory function of post-G MLRCD4+T cells. Parallel coculture experiments conducted in the absence of a Transwell showed that post-G MLRCD4+T cells suppressed by a median of 30% the proliferation of indicator CD4+ T cells if added directly to the culture (data not shown). In addition, we found that significant suppression of bystander autologous CD4+ T cells was induced by the transfer of cell-free supernatants of activated post-GMLRCD4+ T cells (data not shown). As depicted in Figure 6B, the in vitro suppressive activities of post-GMLRCD4+ T cells were partially reversed by the addition of neutralizing antibodies to the cytokines IL-10 and TGF-β1. Interestingly, after removal of the suppressor cells from the coculture, indicator CD4+ T cells remained in a nonproliferating state and entered the cell cycle only if supplemented with exogenous IL-2 or IL-15 or, slightly more pronounced, the combination of both cytokines (data not shown). Because T-cell expansion may induce the recovery of responsiveness by T cells anergized in vitro, we tested the suppressive activity of post-GMLRCD4+ T cells after 4 days of costimulation with IL-2, IL-15, or both. Notably, cytokine-costimulated post-G MLRCD4+ T cells retained their suppressive activity in contrast to indicator CD4+ T cells, which continued not to be suppressive (data not shown).
Regulation of T-cell alloproliferation by post-GMLRCD4+ T cells is cell-contact independent and is affected in part by soluble IL-10 and TGF-β1.
(A) Freshly isolated post-G CD4+ T cells were immediately cocultured with pre-G CD4+ T cells from the same donor; both compartments of the Transwell system received allogeneic TCD PBMCs as stimulator cells and responder cells at a 1:3 ratio. Proliferation of indicator CD4+ T cells in the lower chamber of the Transwell was determined after 7 days of primary coculture by the addition of BrdUrd for the final 24 hours. Median and range recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells. (B) Primary cocultures were performed in the presence or absence of neutralizing antibodies directed against TGF-β1 (αTGF-β1; 20 ng/mL) or IL-10 (αIL-10; 10 μg/mL) or the combination of both mAbs. Control cultures contained an isotype-matched irrelevant mAb added at the same concentration as the αIL-10 and αTGF-β1 antibodies. Median values and ranges recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells.
Regulation of T-cell alloproliferation by post-GMLRCD4+ T cells is cell-contact independent and is affected in part by soluble IL-10 and TGF-β1.
(A) Freshly isolated post-G CD4+ T cells were immediately cocultured with pre-G CD4+ T cells from the same donor; both compartments of the Transwell system received allogeneic TCD PBMCs as stimulator cells and responder cells at a 1:3 ratio. Proliferation of indicator CD4+ T cells in the lower chamber of the Transwell was determined after 7 days of primary coculture by the addition of BrdUrd for the final 24 hours. Median and range recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells. (B) Primary cocultures were performed in the presence or absence of neutralizing antibodies directed against TGF-β1 (αTGF-β1; 20 ng/mL) or IL-10 (αIL-10; 10 μg/mL) or the combination of both mAbs. Control cultures contained an isotype-matched irrelevant mAb added at the same concentration as the αIL-10 and αTGF-β1 antibodies. Median values and ranges recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells.
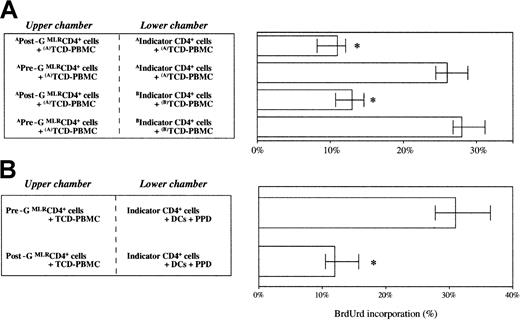
Further studies were conducted to investigate the antigen specificity of the suppression mediated by post-GMLRCD4+ T cells. In the 2-stage culture system that we used, post-GMLRCD4+ T cells were first preactivated with TCD PBMCs from an HLA-mismatched healthy donor (donor A), and these donor A–specific post-GMLRCD4+ T cells were placed in the upper chamber of a Transwell separated from autologous indicator CD4+ T cells preactivated with TCD PBMCs from the same donor or from a different donor (donor B). In these secondary cocultures, the alloreactivities of donor A–specific and of donor B–specific indicator CD4+ T cells were down-regulated, suggesting that the suppressor function of post-GMLRCD4+ T cells was antigen nonspecific (Figure 7A). Notably, triggering of post-G MLRCD4+ T cells through the TCR complex was required for the activation of their suppressor-effector function because quiescent post-GMLRCD4+ T cells did not mediate suppression (data not shown).
Regulation of T-cell alloproliferation by post-GMLRCD4+ T cells is antigen nonspecific.
Freshly isolated pre-G and post-G CD4+ T cells from the same donor were separately primed with allogeneic TCD PBMCs from a different healthy volunteer (donor A or donor B). After 7 days, secondary cocultures were set up by placing donor A–specific or donor B–specific pre-G MLRCD4+ T cells in the lower chamber of a Transwell separated from donor A–specific post-G MLRCD4+ T cells by a semipermeable membrane. Both compartments of the secondary Transwell culture received allogeneic TCD PBMCs (donor A or donor B, as indicated in the figure) as stimulator cells and responder cells at a 1:3 ratio. Proliferation of indicator CD4+ T cells in the lower chamber of the Transwell was determined after 7 days of coculture by the addition of BrdUrd for the final 24 hours. (A) Median values and ranges recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells. (B) Regulation of T-cell proliferation to recall antigens by post-GMLRCD4+ T cells. Freshly isolated pre-G or post-G MLRCD4+ T cells were activated with TCD PBMCs from an allogeneic donor and were cocultured with pre-G CD4+ T cells stimulated with PPD-pulsed autologous DCs (see “Patients, materials, and methods”). Proliferation of pre-G CD4+ T cells in the lower chamber of the Transwell was determined after 7 days of primary coculture by the addition of BrdUrd for the final 24 hours. *P < .05 compared with pre-G CD4+ T cells.
Regulation of T-cell alloproliferation by post-GMLRCD4+ T cells is antigen nonspecific.
Freshly isolated pre-G and post-G CD4+ T cells from the same donor were separately primed with allogeneic TCD PBMCs from a different healthy volunteer (donor A or donor B). After 7 days, secondary cocultures were set up by placing donor A–specific or donor B–specific pre-G MLRCD4+ T cells in the lower chamber of a Transwell separated from donor A–specific post-G MLRCD4+ T cells by a semipermeable membrane. Both compartments of the secondary Transwell culture received allogeneic TCD PBMCs (donor A or donor B, as indicated in the figure) as stimulator cells and responder cells at a 1:3 ratio. Proliferation of indicator CD4+ T cells in the lower chamber of the Transwell was determined after 7 days of coculture by the addition of BrdUrd for the final 24 hours. (A) Median values and ranges recorded in 6 independent experiments are shown. *P < .05 compared with pre-GMLRCD4+ T cells. (B) Regulation of T-cell proliferation to recall antigens by post-GMLRCD4+ T cells. Freshly isolated pre-G or post-G MLRCD4+ T cells were activated with TCD PBMCs from an allogeneic donor and were cocultured with pre-G CD4+ T cells stimulated with PPD-pulsed autologous DCs (see “Patients, materials, and methods”). Proliferation of pre-G CD4+ T cells in the lower chamber of the Transwell was determined after 7 days of primary coculture by the addition of BrdUrd for the final 24 hours. *P < .05 compared with pre-G CD4+ T cells.
Finally, we wanted to address whether post-GMLRCD4+ cells were also capable of suppressing T-cell proliferation in response to a recall antigen presented by professional antigen-presenting cells. To this purpose, PPD-pulsed, monocyte-derived DCs were used to stimulate pre-G CD4+ T cells in the lower compartment of a Transwell. Of note, post-G MLRCD4+ T cells placed in the upper chamber of the Transwell reproducibly suppressed the proliferation of pre-G CD4+ T cells in the lower chamber of the Transwell by a median of 50% (Figure 7B).
Generation of suppressor CD4+ T cells is not enhanced by in vitro exposure to immunosuppressive agents
To ascertain whether the in vitro generation of Tr1 cells could be potentiated by drugs routinely administered in vivo for the prevention or treatment of GVHD after HSC allografting, post-G CD4+ T cells were challenged with alloantigens in the presence of immunosuppressive drugs, as indicated in Table2 (primary MLR). Under these culture conditions, no induction of IL-10 or TGF-β1 production was noted at the single-cell level (data not shown) or in culture supernatants, compared with control cultures of post-G CD4+ T cells performed in the absence of pharmacologic agents. Although pre-GMLRCD4+ T cells differentiated in the presence of immunosuppressive drugs were incapable of mediating the suppression of indicator T cells restimulated with allogeneic TCD PBMCs in secondary Transwell cocultures (data not shown), post-GMLRCD4+ T cells generated in the absence or in the presence of exogenously added drugs inhibited the proliferation of indicator T cells by a median of 40%, suggesting comparable levels of regulatory activity (Table 2).
Effect of immunosuppressive drugs on cytokine production and regulatory activity of post-G CD4+ T cells
| Primary MLR . | Secondary coculture . | ||
|---|---|---|---|
| Drug . | IL-10, pg/mL−1 . | TGF-β1, pg/mL−1 . | BrdUrd incorporation by indicator CD4+ T cells, % . |
| None | 490 | 1175 | 13 |
| Vehicle (EtOH) | 155 | 412 | 15 |
| Tacrolimus, 1 μg/mL | 181 | 1032 | 17 |
| Cyclosporin A, 50 μg/mL | 76 | 976 | 12 |
| Infliximab, 5 μg/mL | 116 | 1000 | 12 |
| Methotrexate, 1 nM | 280 | 478 | 10 |
| Dexamethasone, 10−6 M | 190 | 972 | 12 |
| Mycophenolate mofetil, 0.1 μg/mL | 203 | 934 | 15 |
| Primary MLR . | Secondary coculture . | ||
|---|---|---|---|
| Drug . | IL-10, pg/mL−1 . | TGF-β1, pg/mL−1 . | BrdUrd incorporation by indicator CD4+ T cells, % . |
| None | 490 | 1175 | 13 |
| Vehicle (EtOH) | 155 | 412 | 15 |
| Tacrolimus, 1 μg/mL | 181 | 1032 | 17 |
| Cyclosporin A, 50 μg/mL | 76 | 976 | 12 |
| Infliximab, 5 μg/mL | 116 | 1000 | 12 |
| Methotrexate, 1 nM | 280 | 478 | 10 |
| Dexamethasone, 10−6 M | 190 | 972 | 12 |
| Mycophenolate mofetil, 0.1 μg/mL | 203 | 934 | 15 |
Post-G CD4+ T cells were activated with HLA-DR-mismatched TCD PBMCs in the presence or absence of 1 μg/mL tacrolimus, 50 μg/mL cyclosporin A, 5 μg/mL human or mouse chimeric anti-TNF antibody infliximab, 1 nM methotrexate, 10−6 M dexamethasone, or 0.1 μM mycophenolate mofetil. After 7 days of primary culture, supernatants were harvested for cytokine ELISA, and post-G CD4+ T cells were plated in secondary Transwell cultures separated from indicator (autologous pre-G) CD4+ T cells obtained from the same HSC donor. Both compartments of the Transwell received allogeneic TCD PBMCs as stimulator cells and responder cells at a 1:3 ratio. Proliferation of indicator CD4+ T cells in the lower chamber of the Transwell was determined after 7 days by the addition of BrdUrd for the final 24 hours. Data represent median values recorded in 4 independent experiments performed in duplicate. BrdUrd incorporation by pre-G CD4+ T cells cocultured in the absence of suppressor post-G CD4+ T cells in the Transwell approached 30% in all experiments (data not shown). Pre-G CD4+ T cells released comparable cytokine amounts after activation and exerted no measurable suppression of indicator T cells (data not shown).
EtOH indicates ethyl alcohol.
Lack of suppressor activity by peripheral CD4+ T cells from patients who received allografts with G-CSF–mobilized HSCs
Next, we sought to determine whether T cells with regulatory activity could be differentiated from the peripheral blood of patients who underwent allografting with G-CSF–mobilized HSCs from HLA-identical siblings. Interestingly enough, no increase in the proportion of alloantigen-activated CD4+ T cells releasing IL-10 and TGF-β1 or in cytokine levels in culture supernatants was found compared with CD4+ T cells from healthy donors (Table3). Conversely, CD4+ T cells from patients who underwent allografting secreted significant amounts of the prototypic TH1 cytokine IFN-γ. Consistent with the lack of regulatory activity, these CD4+ T cells did not mediate detectable levels of suppression of third-party bystander T cells when plated in secondary Transwell cocultures (Table 3). In particular, BrdUrd incorporation by indicator CD4+ T cells was of the same order of magnitude in cocultures performed with CD4+ T cells from healthy controls and from patients who underwent allografting. Of interest, TH1 and Tr1 cytokine production was depressed in patient 3, who was receiving immunosuppressive therapies for acute GVHD. Overall, these findings suggested that allogeneic stimulation occurring in vivo after HSC transplantation was insufficient to promote the generation of CD4+ T cells with a Tr1-like functional profile, at least in the context of HLA-identical transplantation.
Cytokine production and regulatory activity of CD4+ T cells from patients who received allografts
| . | Activation stimulus (anti-CD3 mAb + TPA) . | Transwell coculture . | |||||
|---|---|---|---|---|---|---|---|
| IL-10, pg/mL−1 . | IL-10, % . | TGF-β1, pg/mL−1 . | TGF-β1, % . | IFN-γ, pg/mL−1 . | IFN-γ, % . | Lower chamber, % (indicator CD4+ T cells) . | |
| Control 1 | 148 | 4.5 | 378 | 3.0 | 5617 | 20 | 20 |
| Control 2 | 280 | 6.3 | 352 | 3.0 | 7700 | 25 | 27 |
| Patient 1 | 82 | 4.3 | 383 | 1.9 | 9518 | 28 | 23 |
| Patient 2 | 61 | 4.0 | 436 | 3.0 | 5815 | 16 | 16 |
| Patient 3 | < 10 | < 1.0 | 70 | < 1.0 | 80 | 3 | 24 |
| . | Activation stimulus (anti-CD3 mAb + TPA) . | Transwell coculture . | |||||
|---|---|---|---|---|---|---|---|
| IL-10, pg/mL−1 . | IL-10, % . | TGF-β1, pg/mL−1 . | TGF-β1, % . | IFN-γ, pg/mL−1 . | IFN-γ, % . | Lower chamber, % (indicator CD4+ T cells) . | |
| Control 1 | 148 | 4.5 | 378 | 3.0 | 5617 | 20 | 20 |
| Control 2 | 280 | 6.3 | 352 | 3.0 | 7700 | 25 | 27 |
| Patient 1 | 82 | 4.3 | 383 | 1.9 | 9518 | 28 | 23 |
| Patient 2 | 61 | 4.0 | 436 | 3.0 | 5815 | 16 | 16 |
| Patient 3 | < 10 | < 1.0 | 70 | < 1.0 | 80 | 3 | 24 |
CD4+ T cells were purified from 2 healthy cytokine-untreated subjects (ctrl) and from 3 patients with leukemia after transplantation with G-CSF–mobilized peripheral blood HSCs from HLA-identical siblings. Patients 1 and 2 showed no clinical signs of GVHD and were on prophylactic cyclosporin A at testing (days 105 and 30 after grafting, respectively). Patient 3 had acute GVHD at testing (day 38 after grafting) and was receiving immunosuppressive therapies, according to standard clinical practice (mycophenolate mofetil and methylprednisolone). To detect cytokine production, purified CD4+ T cells were activated with 0.1 μg/mL anti-CD3 mAbs and 10 ng/mL 12-O-tetradecanoylphorbol-13-acetate (TPA; both from Sigma Chemical) for 24 hours at 37°C. Culture supernatants were collected and used for cytokine ELISA, whereas cells were used for the flow cytometric evaluation of cytokine production and for Transwell studies, as already detailed. Both compartments of the Transwell received allogeneic TCD PBMCs as stimulator cells and responder cells at a 1:3 ratio. Proliferation of indicator CD4+ T cells from a healthy control was determined after 7 days by the addition of BrdUrd for the final 24 hours. Data represent median values recorded in 2 experiments performed in duplicate.
Discussion
Tr cells play a key role in the maintenance of immunologic tolerance to self-antigens and foreign antigens.26Different subsets of Tr cells, generated in vitro or isolated ex vivo, have the capacity to inhibit the response of other T cells through a cell contact–dependent or a cytokine-dependent mechanism.12 In particular, naturally occurring human CD4+ T cells that constitutively express the CD25 marker have been identified and exert immunosuppression through cell–cell interaction involving cell-surface TGF-β1 but not through soluble factors.28-33 Importantly, human thymus might be crucial for the generation of Tr cells because CD4+CD8− single-positive thymocytes expressing CD25 can inhibit T-cell proliferation in vitro and prevent the development of gastritis, diabetes, and colitis in vivo.34However, Tr cells might also reside within the CD25−compartment, and CD25 expression might be dynamic and not suitable to describe the entire pool of Tr cells.35 36
To date, limited attempts to identify surface markers specific for Tr cells have been made. Relationships among different subsets of Tr cells—for example, Th3 cells that arise after the oral administration of antigen, Tr1 cells, and CD4+CD25+ Tr cells and the precise mechanisms of action and induction of Tr cells in vivo—remain to be thoroughly defined.12
Whereas further studies are needed to characterize the potentially multiple types of regulatory–suppressor T cells, it is well established that the secretion of IL-10 and TGF-β1 is integral to the function of Tr1 cells, as shown by the SCID model of inflammatory bowel disease, in which the cotransfer of CD4+CD45RBlow T cells releasing TGF-β and IL-10 protects from the development of experimental colitis induced by pathogenic CD4+CD45RBhigh T cells.37 38
Our interest in TGF-β1 and IL-10 as candidate effector cytokines contributing to proliferative hyporesponsiveness and suppressor activity of post-G T cells was prompted by several observations. First, TGF-β1 and IL-10 have immunosuppressive and antiproliferative effects.15,17 Second, it has been demonstrated that IL-10 and TGF-β1 are necessary, but each alone is insufficient, to induce antigen-specific T-cell hyporesponsiveness and to protect from GVHD-induced lethality after murine histoincompatible bone marrow transplantation.19,20 Third, we have recently described that T-cell exposure to G-CSF affects the expression of key components of the cell cycle machinery and inhibits the progression through the G1-S restriction point11; this observation is in line with studies showing failure to progress into the late G1 and S phases of the cell cycle following T-cell tolerization with IL-10 and TGF-β1.19
In this study, we used culture conditions in which purified CD4+ T cells were activated with alloantigens through their TCRs, and we found that post-GMLRCD4+ T cells acquired a Tr1-like profile of cytokine secretion, consisting of high IL-10 and moderate TGF-β release, in the absence of significant IL-2 and IL-4 production. Although overall levels of IL-10 were considerably high in bulk cultures of post-G MLRCD4+ T cells, a median of 10% post-G T cells was found to produce IL-10 on a per-cell basis. This observation was not surprising given that the frequency of peripheral T cells responding to allogeneic stimulators is less than 1 of 20 peripheral T cells.39
Consistent with the specific role of GATA-3 in the induction of TH2 cells,40 we found that post-GMLRCD4+ T cells expressed low levels of GATA-3 mRNA, supporting the view that, unlike murine T cells, human T cells are not genuinely polarized to a TH2 profile after exposure to G-CSF in vivo.41
Among the phenotypic features of post-GMLRCD4+ T cells we identified, markedly reduced CD62L and CD28 expression was of interest because CD62L-negative T cells with impaired alloproliferative responses have been reported to increase after in vivo exposure to G-CSF, and defective CD28 costimulation has been advocated as a potential mechanism of T-cell hyporesponsiveness induced by G-CSF.42,43 Notably, CD122 and CD132 expression was enhanced on post-G compared with pre-GMLRCD4+ T cells; this finding was intriguing because Tr1 cells might be exquisitely sensitive to stimulation with the IL-2R γ-chain signaling cytokines.12 No differences in CD25 levels were found in freshly isolated pre-G or post-GMLRCD4+ T cells. Furthermore, the extent of CD25 up-regulation was comparable in pre-G and post-GMLRCD4+ T cells on activation with alloantigens. In contrast to murine CD4+CD45RBlow Tr cells,13 post-GMLRCD4+ T cells with regulatory activity expressed similar levels of CD45RB compared with nonsuppressor pre-G MLRCD4+ T cells. Collectively, post-G MLRCD4+ T cells displayed a memory and partially activated phenotype and exhibited relevant differences to the recently characterized CD4+CD25+ Tr cells, which are known to express similar levels of CD28 and CD62L but reduced levels of CD45RB compared with nonregulatory CD4+CD25−cells.29,32 33
The human chemokine system encompasses a variety of chemotactic cytokines that recruit leukocyte subsets to sites of antigen presentation and inflammation.44-46 Chemokine receptor expression is tightly regulated depending on stage of activation and differentiation of T cells.44 So far, no data on the differential expression of chemokine receptors on Tr1 cells have been published; conversely, CD4+CD25+ Tr cells were recently found to express preferentially CCR4 and CCR8 chemokine receptors and to migrate in response to a number of inflammatory chemokines.46 When we studied post-GMLRCD4+ T cells for the expression of receptors for inflammatory (CXCR3, CCR5) and homeostatic chemokines (CXCR4, CCR7) and for chemokines ascribed to both subfamilies (CCR6), we found a distinctive pattern consisting of high CCR7 levels in the absence of significant CXCR3, CCR5, and CCR6 receptor expression. Cell-surface expression of CXCR4, which is known to be down-regulated after T-cell activation,47 48 was significantly higher in post-G MLRCD4+ T cells than in pre-GMLRCD4+ T cells. Although evaluation of the migratory behavior of post-GMLRCD4+ T cells was beyond the aims of the present investigation, the study of chemokine responses by post-G MLRCD4+ T cells is crucial to assess whether Tr1 cells have the capacity to migrate to sites of inflammation and to control immune responses.
Somewhat expected as a result of the inhibitory effects of IL-10 and TGF-β1 on T-cell expansion,16 17 post-GMLRCD4+ T cells proliferated poorly. Although costimulation with the TH1-promoting cytokine IL-12 was incapable of restoring post-GMLRCD4+ T-cell proliferation, nonproliferating post-G MLRCD4+ T cells rapidly entered the cell cycle if provided exogenous IL-2 or IL-15. Such cytokine-driven or bystander proliferation—for example, proliferation occurring in the absence of antigen recognition by the TCR complex—was equal to that observed with similarly costimulated nonregulatory pre-G MLRCD4+ T cells, indicating a strict requirement for the IL-2R γ-chain signaling cytokines by post-G MLRCD4+ T cells for growth in vitro.
Cultures containing post-G MLRCD4+ T cells inhibited the proliferation of autologous pre-GMLRCD4+ T cells (indicator cells) to allogeneic stimulators and to recall antigens presented by monocyte-derived DCs, demonstrating that post-GMLRCD4+ T cells have the key functional property of Tr cells. It should be pointed out that in vitro–differentiated post-G MLRCD4+T cells were remarkably potent suppressor cells. The percentage of cells with a Tr1-like profile of cytokine production—IL-10++TGF-β1+IL-2low/−IL-4low/−—within post-G cultures approached 10%, as shown by analysis of intracellular cytokines at the single-cell level. Secondary coculture experiments showed that stimulated post-G MLRCD4+T cells were capable of suppressing indicator CD4+ T cells preactivated with TCD PBMCs from a different donor, suggesting that, once triggered through the TCR complex, post-GMLRCD4+ T cells suppressed in an antigen-nonspecific, MHC-unrestricted manner. The concept that post-G MLRCD4+ T cells require TCR triggering to mediate suppression was backed by our finding that the proliferation of autologous indicator CD4+ T cells was not affected by unstimulated post-G CD4+ T cells. Mechanistically, the regulation effected by post-GMLRCD4+ T cells appeared to be independent of cell–cell contact and was counteracted in part by the addition of blocking antibodies to IL-10 and TGF-β1, supporting the view that post-G MLRCD4+ T cells mediated suppression through soluble immunoregulatory factors. Interestingly, neither IL-10 nor TGF-β1 was dispensable for post-GMLRCD4+ T cells to mediate suppression because the proliferative response of indicator CD4+ T cells was partially restored by neutralizing mAbs used separately. Furthermore, pre-GMLRCD4+ T cells remained in a nonproliferating state after the removal of suppressor post-GMLRCD4+ T cells from the Transwell, and only the addition of IL-2 or IL-15 was capable of restoring measurable levels of proliferation. As already shown for human CD4+CD25+ Tr cells,49 IL-2– or IL-15–costimulated post-G MLRCD4+ T cells continued to be suppressive against nonregulatory autologous pre-G MLRCD4+ T cells, indicating that expansion was not associated with the loss of regulatory properties, at least not in short-term culture.
Previously, it has been shown that immunosuppressive drugs might induce human CD4+ T cells to differentiate in vitro into regulatory T cells producing high levels of IL-10.50Importantly, an increase of CD4+CD25+ Tr cells has also been demonstrated in tolerant mice receiving short treatment with vitamin D3 and mycophenolate mofetil after fully mismatched islet allografting,51 suggesting that pharmacologic agents added in vitro or administered in vivo might favor the development of Tr cells that can adoptively transfer transplantation tolerance. In our system model, no enhancement of Tr1 cell differentiation was evident when post-G CD4+ T cells were activated in vitro in the presence of a wide spectrum of drugs routinely administered in vivo for GVHD prevention or treatment. Further studies are ongoing to test whether in vivo immunosuppressive therapies can alter the balance between autoaggressive and regulatory T-cell responses.
Because studies in mice and humans have suggested that the activation of Tr cells might be an integral component of the allograft response,52,53 we investigated whether Tr cells could be generated in vitro from the peripheral blood of patients who underwent allograft with G-CSF–mobilized HSCs from HLA-identical siblings. Interestingly, no increase of the IL-10– and TGF-β1–producing ability of CD4+ T cells and no significant regulatory activity against bystander T cells were evidenced when compared with CD4+ T cells from healthy control subjects; rather, alloantigen-activated CD4+ T cells from patients who received allografts were polarized to a TH1-like cytokine production profile. These findings suggested that allorecognition was insufficient to promote the differentiation of Tr cells, at least in the context of HLA-identical HSC transplantation. Investigations on a wide cohort of patients who undergo transplantation with HLA-mismatched HSCs are needed to determine whether the spontaneous generation of Tr1 cells may correlate with the lack of in vivo GVHD or with immunologic tolerance of donor-derived T cells to antigens uniquely expressed on recipient cells, as recently shown in one patient with SCID.53
From the results shown here, cytokine secretion and immunoregulatory properties of the human CD4+ T cells generated after in vivo treatment with G-CSF were superimposable with those of Tr1 cells.12 13 To our knowledge, this is the first set of data reporting the development of Tr1 cells from human peripheral blood T cells exposed to G-CSF in vivo. Interestingly, a suppressive and regulatory phenotype was induced specifically by in vivo exposure to G-CSF because normal CD4+ T cells activated with alloantigens in the presence of exogenously provided G-CSF were incapable of mediating suppression of bystander autologous CD4+ T cells (data not shown).
At present, the cellular and molecular events that direct Tr1 cell development in vivo are unknown, and whether Tr cells are a unique lineage of cells imprinted with a regulatory function or whether Tr cell function may be acquired by naive T cells in the periphery is still unresolved.34 Of interest, an average 3.5-fold increase of IFN-α and IL-10 serum levels was found after clinical provision of G-CSF to healthy donors (S.R., unpublished data, March 2001). Because IFN-α and IL-10 may function as growth or differentiation factors for human Tr1 cells,54 it is tempting to speculate that IFN-α and IL-10 induced by G-CSF might favor the differentiation of Tr1 cells in the periphery. In addition, IFN-α and IL-10 may affect DC generation and maturation, providing an additional pathway for the development of T cells with regulatory activity.34
Because Tr cells can be expanded and maintained in vitro,49 adoptive transfer of Tr1 cells generated ex vivo after G-CSF treatment or immune manipulation to re-establish dominant Tr activities in vivo can be envisaged as potential therapeutic options for GVHD and other human T-cell–mediated diseases and for the prevention of graft rejection. However, such strategies should be approached cautiously—Tr1 cells might down-regulate T-cell responses to antigens presented by autologous DCs and induce systemic collapse of antitumor immunity.55 56
We thank Dr Tiziana Di Pucchio (Laboratory of Virology, Istituto Superiore di Sanità, Rome, Italy) for the generous gift of monoclonal antibodies against chemokine receptors and for helpful discussions. We also thank Dr Mothanje Barbara Lucia (Department of Infectious Diseases, Catholic University, Rome, Italy) for providing PPD for autologous MLR experiments.
Prepublished online as Blood First Edition Paper, June 7, 2002; DOI 10.1182/blood-2001-12-0291.
Supported in part by M.U.R.S.T. (Ministero dell'Università e della Ricerca Scientifica e Tecnologica, Italy).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Sergio Rutella, Department of Hematology, Catholic University Medical School, Largo A. Gemelli 8-00168, Rome, Italy; e-mail: sergiorutella@tin.it.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal