Growth and survival of chronic B-cell tumors are favored by the malignant cell's capacity to respond to selected microenvironmental stimuli provided by nontumoral bystander cells. To investigate which mechanisms operate in these crosstalks and whether they are malignancy-related or reproduce the mechanisms used by normal B cells we have studied the expression and functional role of semaphorin CD100 (now called Sema4D) in chronic lymphocytic leukemia (CLL) cells and normal CD5+ B cells. We demonstrate here that (1) leukemic and normal CD5+ B lymphocytes uniformly express CD100; (2) the CD100 high-affinity receptor Plexin-B1 is expressed by bone marrow stromal cells, follicular dendritic cells, and activated T lymphocytes, and is thus available to CD100+ lymphocytes in different specific microenvironments; and (3) upon interaction between CD100 and Plexin-B1 both CLL and normal CD5+ B cells increase their proliferative activity and extend their life span. These findings establish that Plexin-B1 is an easily accessible receptor for CD100 within the immune system. The encounter of CD100+ leukemic cells with Plexin-B1 may promote the proliferation and survival of malignant cells. The crosstalk operated by the CD100/Plexin-B1 interaction is not malignancy related but reproduces a mechanism used by normal CD5+ B cells.
Introduction
Evidence is accumulating that the capacity of malignant cells to respond to selected microenvironmental signals confers a growth advantage and an extended cell survival to chronic lymphoid tumors of B-cell type (reviewed in Ghia and Caligaris-Cappio1). Therefore it becomes crucial to identify which molecular interactions link malignant B cells to the microenvironment and to investigate whether the neoplastic clone's response to microenvironmental signals is malignancy-related or reproduces a pattern used by normal B cells. B-cell chronic lymphocytic leukemia (CLL) is a suitable model to address these problems as it is characterized by the expansion of monoclonal CD5+ B lymphocytes that accumulate in secondary lymphoid organs, bone marrow (BM), and peripheral blood (PB),2 not only because of genetic lesions but also thanks to their interactions with nontumoral bystander cells.1
Accessory cells and T lymphocytes appear to play a critical role in the CLL cell/microenvironment crosstalks. A direct physical contact between BM stromal cells and leukemic cells extends the CLL cell survival.3,4 Follicular dendritic cells (FDCs) are closely associated with CLL cells in the early phase of BM involvement.5 Moreover the PB of CLL patients has been shown to contain cells that in vitro can differentiate into adherent nurselike cells, endowed with the capacity of protecting the attached leukemic B cells from spontaneous apoptosis.6 The absolute number of T cells is increased in CLL patients7 and T-cell subsets are redistributed: CD4+ T cells predominate in involved BM and lymph nodes (LNs)8 where they tend to concentrate around and within the proliferating pseudofollicles.9 The T-cell receptor (TCR) repertoire frequently shows an oligoclonal pattern10 and several T-cell cytokines (including interleukin-4 [IL-4], interferon-α [IFN-α], and IFN-γ) are able to inhibit CLL cell apoptosis.11 Many reports suggest that CLL cells and T cells may be involved in a reciprocal dialog via CD40/CD40Ligand (CD40L) interactions because the stimulation of CD40 rescues CLL cells from apoptosis and induces their proliferation.12-16
Taken together these observations lead to the view that bystander/malignant cell contacts deliver signals important for the extended survival and proliferation of CLL cells.1 To identify which molecular interactions link malignant B, T, and accessory cells we have focused our attention upon CD100 (recently renamed Sema4D),17 a transmembrane protein belonging to the fourth group of the semaphorin family. Semaphorins are soluble or membrane-bound proteins that are mainly involved in neuronal guidance,18-20 but also play a role in organogenesis, angiogenesis, and neoplastic progression.21-23 CD100 is the only human semaphorin known to be expressed by normal T and B lymphocytes and its expression is enhanced after lymphocyte activation.24,25 Of interest, in CD100-deficient mice, CD5+ B cells, the putative normal counterpart of CLL cells,26 are significantly reduced in number suggesting a role for CD100 in their development.27 So far, 2 receptors for CD100 have been described: CD7225,28 and Plexin-B1.29 CD72 acts as a low-affinity receptor for CD100 expressed by lymphocytes. Plexin-B1, expressed by epithelial cells, specifically binds CD100 with high affinity,29 but it is unknown whether it exerts the same function also within the immune system.
In this work, we start from the observation that CLL cells express CD100. We next demonstrate that Plexin-B1 is expressed by FDC, BM stromal cells, and activated T lymphocytes, and is thus potentially available to CD100+ lymphocytes in different specific microenvironments. We then provide evidence that CD100/Plexin-B1 interactions deliver survival and proliferation signals to leukemic CD5+ B cells. Finally we show that such a mechanism is not malignancy related but is also operating in normal CD5+ B cells. These data indicate that CD100/Plexin-B1 interactions allow the crosstalks of B lymphocytes with a host of different cells within the immune system. CLL cells may take advantage of these interactions to receive both proliferative and antiapoptotic stimuli in the different microenvironments where they accumulate.
Patients, materials, and methods
Patients and tissues
We analyzed PB samples from 46 CLL patients diagnosed according to standard clinical and laboratory criteria and staged according to Rai et al.30
From patients undergoing tonsillectomy, 5 tonsils were obtained as discarded tissues. Two histologically normal BM samples from patients undergoing evaluation for nonhematologic malignancies and 2 BM samples from CLL patients were used to establish long-term primary cultures of BM stromal cells.
All tissue samples were obtained following institutional guidelines (Ospedale Mauriziano “Umberto I,” Torino).
Cells
Mononuclear cells from CLL PB and manually disaggregated tonsils were isolated by centrifugation through a Ficoll-Hypaque (FH) density gradient. Cells were washed with phosphate-buffered saline solution and resuspended in RPMI 1640 medium supplemented with 10% fetal calf serum (FCS), 2 mM L-glutamine and 15 μg/mL gentamicin (complete RPMI [cRPMI]; Invitrogen-Life Technologies, Glasgow, United Kingdom).
The FDC cell lines FDC-1 (kind gift of E. Clark, Seattle, WA)31,32 and HK (kind gift of Y. S. Choi, New Orleans, LA)33 were maintained in cRPMI. The murine MLP2934 (MLP) was maintained in Dulbecco modified Eagle medium supplemented with 10% FCS.
The murine epithelial cell line MLP29 stably expressing Plexin-B1 (MLP/Plex-B1) was obtained by transfection with the calcium-phosphate procedure, followed by G418 selection. Plexin-B1 cDNA was a kind gift of L. Tamagnone (IRCC, Candiolo). Expression of the exogenous protein was checked by cytofluorograph analysis after each transfection.
Monocyte-derived dendritic cells (DCs) were generated by culturing PB monocytes from healthy donors in cRPMI supplemented with 50 ng/mL granulocyte-macrophage colony-stimulating factor (GM-CSF) and 100 U/mL IL-4 for 7 days.35
T cells were negatively purified from healthy donor's PB and patient's BM using anti-CD16, -CD56, -CD14, and -CD19 Dynabeads (Dynal, Oslo, Normay). Normal PB T cells were activated by culturing on anti-CD3– and anti-CD28–coated plates (5 μg/mL; Caltag Laboratories, San Francisco, CA).
To establish BM stromal cell cultures, mononuclear cells from BM aspirates were isolated by centrifugation through an FH density gradient. BM mononuclear cells were cultured in α-minimal essential medium (α-MEM; Invitrogen-Life Technologies, Glasgow, United Kingdom) supplemented with 20% FCS and 2 × 10−6 M methylprednisolone (Sigma-Aldrich, Milano, Italy). The adherent cells were weekly fed with replacement of 50% of the medium until confluent layers were formed.
CD19+ enrichment
Tonsillar mononuclear cells were labeled with a mixture of anti-CD3, -CD14, -CD16, and -CD56 (Caltag Laboratories) monoclonal antibodies (mAbs). After washing, the cells were incubated with goat anti–mouse immunoglobulin (Ig) microbeads (Miltenyi Biotech, Germany) and separated on a magnetic-activated cell separation (MACS) column according to the manufacturer's instructions. The total B fraction was more than 97% pure as determined by flow cytometry.
Flow cytometric analysis
Surface staining of cells was performed using the following mAbs: fluorescein isothiocyanate (FITC)–labeled anti-CD5 (Becton Dickinson, San Jose, CA), anti-CD72 (PharMingen, San Diego, CA), phycoerythrin (PE)–labeled anti-CD23 (Caltag Laboratories), anti-CD100 (Immunotech, Marseille, France), and tricolor (TC)–labeled anti-CD19 (Caltag Laboratories). Polyclonal FITC-conjugated rabbit anti–human IgM, IgG, IgA and IgD, antihuman κ light chain, and polyclonal PE-conjugated rabbit antihuman λ light chain were purchased from Southern Biotechnology Associates (SBA, Birmingham, AL). Expression of surface Plexin-B1 was determined by indirect immunofluorescence using an unlabeled polyclonal rabbit anti–Plexin-B1 Ab (kind gift of L. Tamagnone) and an FITC-conjugated goat anti–rabbit Ig (SBA). The specificity of the anti–Plexin-B1 Ab was assessed by immunoprecipitation and Western blot analysis (Figure1).
The polyclonal antibody against Plexin-B1 is specific for the molecule.
The specificity of the Ab against Plexin-B1 was assessed by Western blot analysis after immunoprecipitation with an anti–Plexin-B1 monoclonal Ab (A) and further confirmed by cytofluorograph analysis (B) on the following cells: 1, MLP/Plex-B1; 2, follicular dendritic cell line (FDC-1); 3, normal in vitro activated T lymphocytes; and 4, MLP wild type.
The polyclonal antibody against Plexin-B1 is specific for the molecule.
The specificity of the Ab against Plexin-B1 was assessed by Western blot analysis after immunoprecipitation with an anti–Plexin-B1 monoclonal Ab (A) and further confirmed by cytofluorograph analysis (B) on the following cells: 1, MLP/Plex-B1; 2, follicular dendritic cell line (FDC-1); 3, normal in vitro activated T lymphocytes; and 4, MLP wild type.
Flow cytometric analyses were performed on a FACScalibur equipped with Cellquest research software (Becton Dickinson) and mean fluorescence intensity (MFI) was evaluated.
Immunoprecipitation and Western blot analysis
Cells were lysed with extraction buffer (EB) 20 mM Tris-HCl at pH 7.4, 5 mM EDTA (ethylenediaminetetraacetic acid), 150 mM sodium chloride, 10% glycerol, and 1% Triton X-100 in the presence of protease inhibitors and 1 mM sodium orthovanadate. After immunoprecipitation with an unlabeled monoclonal mouse anti–Plexin-B1 Ab (kind gift of L. Tamagnone), Western blots were performed according to standard methods using an unlabeled polyclonal rabbit anti–Plexin-B1 Ab (kind gift of L. Tamagnone). Final detection was performed by enhanced chemiluminescence (ECL; Amersham Biosciences Europe, Cologno Monzese, Milan, Italy).
RNA preparation and reverse transcriptase–polymerase chain reaction (RT-PCR)
Total RNA was extracted from 1 to 3 × 106cells using guanidinium thiocyanate method (RNAzol; Biotecx Laboratories, Houston, TX). RNA was reverse-transcribed into cDNA using 200 U of Superscript II, Rnase H− Reverse Transcriptase (Invitrogen-Life Technologies Italia S.r.l., San Giuliano Milanese, MI, Italy) and amplified by PCR. The PCR reaction was performed in 20 μL with 0.2 mM deoxynucleoside triphosphate (dNTP), 10x GeneAmp buffer (Perkin Elmer Italia, Monza, MI, Italy), 0.5 U AmpliTaq DNA polymerase (Perkin Elmer) and 10 pmol of each specific primer for Plexin-B1: forward, 5′-AAGAACCCCAAGCTGATGCTGCGCAGG-3′; reverse, 5′-CCTTCACGGGCACGCCCTGGGCCT-3′.
Cycling conditions were as follows: 1 cycle at 94°C for 3 minutes followed by 35 cycles at 94°C for 45 seconds, 68°C for 45 seconds, 72°C for 45 seconds, and a final cycle of extension at 72°C for 10 minutes.
Amplified products were resolved by electrophoresis on a 1.5% agarose gel.
Analysis of Ig VH gene sequences
To determine the Ig VH gene family used by leukemic cells, 1 μL of cDNA was amplified using a sense VH leader primer in combination with the appropriate antisense CHprimer (Table 1). The PCR reactions were performed in 20 μL using 10 pmol of each primer and the following cycling conditions: 1 cycle at 94°C for 3 minutes followed by 35 cycles at 94°C for 45 seconds, 62°C for 30 seconds, 72°C for 45 seconds, and a final cycle of extension at 72°C for 10 minutes.
Oligonucleotide primers used for VH gene amplification
| . | Primers . |
|---|---|
| VH leader primers | |
| VH1 | ATGGACTGGACCTGGAGG |
| VH2 | CACGAACTCCTGCTGCTGACCA |
| VH3a | GCTGGGTTTTCCTTGTTGC |
| VH3b | ATGGAGTTTGGGAGCTGAGCTG |
| VH4 | GCTCCCAGATGGGGTCCTG |
| VH5 | CTCCTCCTGGCTGTTCTCC |
| VH6 | CTGTCTCCTTCCTCATCTTCC |
| CHisotype-specific primers | |
| IgM | CAGGAGAAAGTGATGGAGTCG |
| IgG | GGGGAAGTAGTCCTTGACCAG |
| IgA | GACGCTCAGCGGGAAGACCTT |
| . | Primers . |
|---|---|
| VH leader primers | |
| VH1 | ATGGACTGGACCTGGAGG |
| VH2 | CACGAACTCCTGCTGCTGACCA |
| VH3a | GCTGGGTTTTCCTTGTTGC |
| VH3b | ATGGAGTTTGGGAGCTGAGCTG |
| VH4 | GCTCCCAGATGGGGTCCTG |
| VH5 | CTCCTCCTGGCTGTTCTCC |
| VH6 | CTGTCTCCTTCCTCATCTTCC |
| CHisotype-specific primers | |
| IgM | CAGGAGAAAGTGATGGAGTCG |
| IgG | GGGGAAGTAGTCCTTGACCAG |
| IgA | GACGCTCAGCGGGAAGACCTT |
VH gene sequences were determined by reamplifying 2.5 μL of the original cDNA using the appropriate VH leader and CH primers. These reactions were carried out at the same cycling conditions described in “RNA preparation and reverse transcriptase–polymerase chain reaction (RT-PCR).” PCR products were sequenced directly after purification with PCR Preps (Promega, Madison, WI) using an automated DNA sequencer (Applied Biosystem, Foster City, CA). Sequences were compared with those present in the V BASE sequence directory (http://www.mrc-cpe.cam.ac.uk/databases.php?menu9).36The sequences with a germ-line homology 98% or higher were considered unmutated, whereas those with a homology less than 98% mutated.37 38
Quantitative assessment of apoptosis
Binding of Annexin V–FITC was used to follow phosphatidylserin exposition on early apoptotic cells. The staining was performed according to manufacturer's instruction using the Annexin V–based apoptosis detection kit (Bender MedSystem, Vienna, Austria). To selectively analyze the CD5+ B-cell subset, CD19+ purified B cells were stained with allophycocyanin (APC)–labeled anti-CD5 (Caltag Laboratories) and properly gated during the analysis.
Cell-cycle analysis
The percentage of proliferating CLL cells was determined by assessment of DNA content after staining with propidium iodide (PI) using DNA-con kit Cicloscope B-NL (Cytognos, Salamanca, Spain) and following manufacturer's instructions. To selectively analyze the features of the CD5+ B-cell subset, CD19+purified B cells were stained with APC-labeled anti-CD5 and properly gated during the analysis. PI incorporation was analyzed using a FACScalibur instrument equipped with the Doublet Discriminator Module (Becton Dickinson).
Soluble CD100 (sCD100)
The CD100 construct described in Giordano et al39 was fused in frame with glutathione-S–transferase (GST) at the C′ protein terminus. The construct was cloned in pMT2 eukaryotic expression vector and transfected in COS cells. Supernatants were incubated for 2 hours at 4°C in the presence of glutathione-sepharose. The fusion protein was first eluted with 50 mM glutathione and 100 mM HEPES (4-(2-Hydroxyethyl)-1-piperazineethanesulfonic acid; pH 8) and dialyzed. The purified protein was then run on a sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) under reducing conditions, subjected to silver staining (Pierce, Helsingborg, Sweden), and quantified.
Cell cultures
Leukemic and normal CD5+ B cells were cultured in 6-well plates at a concentration of 1 × 106 cells/mL in a total volume of 3 mL. In coculture experiments, 2 × 105 MLP (either wild type or Plexin-B1–transfected) or autologous Plexin-B1+ primary BM stromal cells from CLL patients were cultured together with 1.5 × 106 leukemic cells in a 12-well plate in α-MEM with 10% FCS. In selected experiments, sCD100 was either added to plated CLL cells or preincubated for 2 hours with MLP or MLP/Plex-B1 transfectants. In the experiments with CD40L, cells were cultured in 6-well plates at a concentration of 1 × 106 cells/mL with or without 0.5 μg/mL of trimeric human recombinant CD40L protein, (Alexis Biochemicals, San Diego, CA).
Statistical analysis
The statistical analysis of the data was performed using the Dunnet test.
Results
CD100 is expressed by CLL cells
The expression of CD100 was analyzed by flow cytometry on CD19+CD5+ cells from 46 CLL patients. CD100 was expressed by virtually all leukemic cells in all cases studied (Figure2) irrespective of their Ig VH mutational status. The MFI range of CD100 expression in all patients was 200 to 280. In the same specimens also CD3+ T cells were CD100+.
CLL cells express CD100 on the surface.
The leukemic cells from CLL patients were stained with PE–labeled anti-CD100 mAb and analyzed by flow cytometry. The analysis was performed gating on CD19+CD5+cells and the level of CD100 expression was measured by MFI. Dark histogram represents the fluorescence obtained with negative control isotype–matched mAb; white histogram shows positive cells in a representative case.
CLL cells express CD100 on the surface.
The leukemic cells from CLL patients were stained with PE–labeled anti-CD100 mAb and analyzed by flow cytometry. The analysis was performed gating on CD19+CD5+cells and the level of CD100 expression was measured by MFI. Dark histogram represents the fluorescence obtained with negative control isotype–matched mAb; white histogram shows positive cells in a representative case.
Plexin-B1 is expressed in LN and BM microenvironments
We then asked whether CD100+ CLL cells might be exposed to the CD100 receptor Plexin-B1 in the tissues where they usually accumulate during the disease progression (ie, LN and BM). The expression of Plexin-B1 was screened by RT-PCR and confirmed at protein level by cytofluorograph analysis. The protein was observed in CLL BM stromal cells and T cells (Figure 3).
Plexin-B1 expression in CLL microenvironmental cells obtained from patients' BM.
Primary cultures of stromal cells and isolated T cells were evaluated for the expression of Plexin-B1 both at RNA level by RT-PCR (A) and at protein level by cytofluorograph analysis (B-C) with a polyclonal rabbit antihuman Plexin-B1 Ab (right panels) or with an irrelevant Ab as control (left panels).
Plexin-B1 expression in CLL microenvironmental cells obtained from patients' BM.
Primary cultures of stromal cells and isolated T cells were evaluated for the expression of Plexin-B1 both at RNA level by RT-PCR (A) and at protein level by cytofluorograph analysis (B-C) with a polyclonal rabbit antihuman Plexin-B1 Ab (right panels) or with an irrelevant Ab as control (left panels).
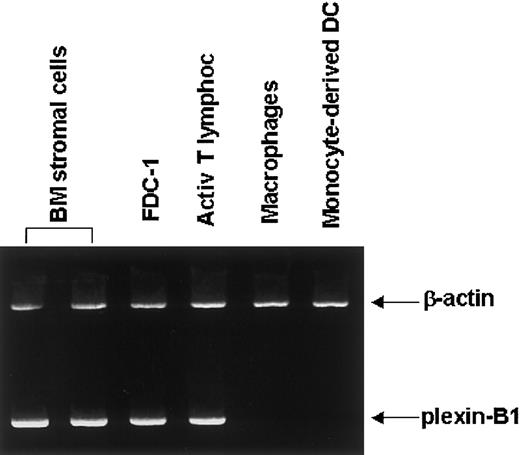
As for normal cell populations, Plexin-B1 was detected in primary normal BM stromal cells, normal in vitro–activated PB T lymphocytes, and FDC cell lines (FDC-1 and HK), whereas it was negative in normal macrophages and monocyte-derived DCs (Figure4).
Plexin-B1 expression in normal microenvironmental cells.
RT-PCR analysis of Plexin-B1 expression in 2 samples of normal primary BM stromal cells, in a follicular dendritic cell line (FDC-1), in normal in vitro–activated T lymphocytes, in macrophages, and in monocyte-derived dendritic cells (DCs). The size of Plexin-B1–amplified products was 303 base pairs as expected.
Plexin-B1 expression in normal microenvironmental cells.
RT-PCR analysis of Plexin-B1 expression in 2 samples of normal primary BM stromal cells, in a follicular dendritic cell line (FDC-1), in normal in vitro–activated T lymphocytes, in macrophages, and in monocyte-derived dendritic cells (DCs). The size of Plexin-B1–amplified products was 303 base pairs as expected.
CD100 engagement sustains viability and enhances proliferation of CLL cells
We next addressed the question whether Plexin-B1 can be a receptor for CD100 also within the immune system. CLL cells from 12 patients (7 with mutated and 5 with germ-line Ig VH genes) were cocultured with murine MLP epithelial cell line either wild type (MLP) or stably transfected with human Plexin-B1 (MLP/Plex-B1). Viability and proliferation of CLL cells were tested at different time points.
CLL cells showed a significantly better viability, as shown by Annexin V staining (Table 2) and higher proliferation rate (ie, cells in the S, G2, M phases of the cell cycle as shown by PI staining; Table4) after 72 to 96 hours of coculture with MLP/Plex-B1, compared with the cocultures with wild-type MLP suggesting a functional significance of the CD100/Plexin-B1 interaction. Given the supportive effect of adherent cell layers on normal and malignant B cells, it was not surprising to observe better viability and increased proliferation when malignant cells were cultured in the presence of wild-type MLP rather than with medium only. No difference was detected between Ig VH–mutated and unmutated cases. To ensure that the effects obtained with murine MLP cell lines actually reproduced what might happen in vivo in CLL patients, in 2 patients where both PB and BM samples were available we set up coculture experiments in which CLL cells were cultured with autologous Plexin-B1+ primary BM stromal cells. Autologous cocultures yielded the same results in terms of both cell viability (Table 3) and cell proliferation (Table 5).
CLL cell viability is sustained when exposed to Plexin-B1 transfectants (MLP/Plex-B1)
| Day . | CLL cells alone . | + MLP . | + MLP/Plex-B1* . | + MLP/Plex-B1 + sCD100 . | + CD40L . | + MLP + CD40L . | + MLP/Plex-B1 + CD40L . |
|---|---|---|---|---|---|---|---|
| 1 | 66 (± 7.1) | 58 (± 8.8) | 65 (± 9.5) | 63 (± 3.4) | 55 (± 10) | 58 (± 8.3) | 69 (± 7) |
| 2 | 52 (± 6.4) | 56 (± 7.1) | 70 (± 4.5) | 57† (± 6) | 52 (± 8.4) | 59 (± 4.8) | 72 (± 4.1) |
| 3 | 48 (± 3.9) | 52 (± 4.2) | 67 (± 3.2) | 40† (± 4.5) | 53 (± 2.7) | 54 (± 3.3) | 75 (± 2.5) |
| 4 | 38 (± 6.4) | 53 (± 7.2) | 73 (± 4.5) | 41† (± 4.3) | 53 (± 7.4) | 54 (± 5.2) | 75 (± 3.9) |
| Day . | CLL cells alone . | + MLP . | + MLP/Plex-B1* . | + MLP/Plex-B1 + sCD100 . | + CD40L . | + MLP + CD40L . | + MLP/Plex-B1 + CD40L . |
|---|---|---|---|---|---|---|---|
| 1 | 66 (± 7.1) | 58 (± 8.8) | 65 (± 9.5) | 63 (± 3.4) | 55 (± 10) | 58 (± 8.3) | 69 (± 7) |
| 2 | 52 (± 6.4) | 56 (± 7.1) | 70 (± 4.5) | 57† (± 6) | 52 (± 8.4) | 59 (± 4.8) | 72 (± 4.1) |
| 3 | 48 (± 3.9) | 52 (± 4.2) | 67 (± 3.2) | 40† (± 4.5) | 53 (± 2.7) | 54 (± 3.3) | 75 (± 2.5) |
| 4 | 38 (± 6.4) | 53 (± 7.2) | 73 (± 4.5) | 41† (± 4.3) | 53 (± 7.4) | 54 (± 5.2) | 75 (± 3.9) |
Leukemic cells significantly sustained their viability when exposed to Plexin-B1 transfectants (MLP/Plex-B1) in comparison with MLP wild type (*P < .05). The effect on viability was significantly abolished by soluble CD100 (MLP/Plex-B1 or stromal cells + sCD100; †P < .05). The coculture experiments were performed also in the presence of soluble CD40L (MLP or MLP/Plex-B1 + CD40L). Viability was assessed by cytofluorograph analysis of Annexin V staining. The numbers express the percentage of viable CLL cells and represent the mean values ± standard deviations obtained in 12 independent experiments.
CLL cell viability is sustained when cocultured with autologous Plexin-B1+ BM stromal cells
| Day . | CLL cells alone . | + Autologous stromal cells* . | + Autologous stromal cells + sCD100 . |
|---|---|---|---|
| 1 | 58 (± 0.7) | 81 (± 10.6) | 72 (± 10.6) |
| 3 | 57 (± 1.4) | 82 (± 5.6) | 65† (± 6.3) |
| 4 | 56 (± 4.9) | 84 (± 4.9) | 60† (± 2.1) |
| Day . | CLL cells alone . | + Autologous stromal cells* . | + Autologous stromal cells + sCD100 . |
|---|---|---|---|
| 1 | 58 (± 0.7) | 81 (± 10.6) | 72 (± 10.6) |
| 3 | 57 (± 1.4) | 82 (± 5.6) | 65† (± 6.3) |
| 4 | 56 (± 4.9) | 84 (± 4.9) | 60† (± 2.1) |
Leukemic cells significantly sustained their viability when cocultured with autologous Plexin-B1+ BM stromal cells in comparison with CLL cells alone. (*P < .01.) The effect on viability was significantly abolished by soluble CD100 (stromal cells + sCD100; †P < .05). Viability was assessed by cytofluorograph analysis of Annexin V staining. The numbers express the percentage of viable CLL cells and represent the mean values ± standard deviations obtained in 2 independent experiments.
In order to demonstrate that the effects described were specifically generated by the CD100/Plexin-B1 interaction, we blocked the availability of Plexin-B1 by preincubating the xenogeneic cell line or the human BM stromal cell cultures with sCD100. As shown in Tables 2-5, both sustained viability, and proliferation of CLL cells was completely abolished in the presence of sCD100. As CLL cells are CD72+ and as CD72 is a low-affinity receptor for CD100, the possibility exists that some of the observed effects might be at least in part accounted for by the concomitant inhibition of the CD72/CD100 interactions that likely take place whenever CLL cells are in contact. To rule out this possibility another set of experiments was performed aimed at blocking the CD72 availability by adding sCD100 to cultured CD72+, CD100+ CLL cells. No difference in terms of both cell viability and cell proliferation was observed when CLL cells were exposed also to sCD100 (Table 6). Likewise the addition of sCD100 to CLL cells cultured in presence of MLP did not influence the supporting effect of MLP. On the contrary, sCD100 drastically reduced the effects of MLP/Plexin-B1 (Table 6) indicating a major role for Plexin-B1.
CLL cell proliferation is enhanced when exposed to Plexin-B1 transfectants (MLP/Plex-B1)
| Day . | CLL cells alone . | + MLP . | + MLP/Plex-B1* . | + MLP/Plex-B1 + sCD100† . | + CD40L . | + MLP + CD40L . | + MLP/Plex-B1 + CD40L . |
|---|---|---|---|---|---|---|---|
| 1 | 0.8 (± 0.3) | 3.3 (± 0.7) | 7.0 (± 0.4) | 1 (± 0.2) | 1.8 (± 0.5) | 4.2 (± 0.7) | 8.0 (± 0.6) |
| 2 | 0.5 (± 0.2) | 3.1 (± 0.5) | 6.7 (± 0.5) | 1.3 (± 0.3) | 1.9 (± 0.3) | 4.3 (± 0.5) | 8.1 (± 0.6) |
| 3 | 0.2 (± 0.1) | 3.1 (± 0.3) | 6.9 (± 0.5) | 1.2 (± 0.2) | 2.0 (± 0.3) | 4.3 (± 0.6) | 8.0 (± 0.5) |
| 4 | 0.2 (± 0.2) | 3.3 (± 0.1) | 7.0 (± 0.6) | 1.1 (± 0.7) | 2.1 (± 0.1) | 4.2 (± 0.4) | 7.5 (± 0.4) |
| Day . | CLL cells alone . | + MLP . | + MLP/Plex-B1* . | + MLP/Plex-B1 + sCD100† . | + CD40L . | + MLP + CD40L . | + MLP/Plex-B1 + CD40L . |
|---|---|---|---|---|---|---|---|
| 1 | 0.8 (± 0.3) | 3.3 (± 0.7) | 7.0 (± 0.4) | 1 (± 0.2) | 1.8 (± 0.5) | 4.2 (± 0.7) | 8.0 (± 0.6) |
| 2 | 0.5 (± 0.2) | 3.1 (± 0.5) | 6.7 (± 0.5) | 1.3 (± 0.3) | 1.9 (± 0.3) | 4.3 (± 0.5) | 8.1 (± 0.6) |
| 3 | 0.2 (± 0.1) | 3.1 (± 0.3) | 6.9 (± 0.5) | 1.2 (± 0.2) | 2.0 (± 0.3) | 4.3 (± 0.6) | 8.0 (± 0.5) |
| 4 | 0.2 (± 0.2) | 3.3 (± 0.1) | 7.0 (± 0.6) | 1.1 (± 0.7) | 2.1 (± 0.1) | 4.2 (± 0.4) | 7.5 (± 0.4) |
Leukemic cells significantly enhanced their proliferative activity when exposed to Plexin-B1 transfectants (MLP/Plex-B1) in comparison with MLP wild type (*P < .01). The effect on proliferation was significantly abolished by soluble CD100 (MLP/Plex-B1 or stromal cells + sCD100; †P < .05). The coculture experiments were performed also in the presence of soluble CD40L (MLP or MLP/Plex-B1 + CD40L). Proliferation activity was measured by the evaluation of DNA content after PI staining. The numbers express the percentage of CLL cells in S, G2, M phases of the cell cycle and represent the mean values ± standard deviations obtained in 12 independent experiments.
CLL cell proliferation is enhanced when cocultured with autologous Plexin-B1+ BM stromal cells
| Day . | CLL cells alone . | + Autologous stromal cells* . | + Autologous stromal cells + sCD100† . |
|---|---|---|---|
| 1 | 0.4 (± 0.1) | 1.6 (± 0.1) | 0.6 (± 1.4) |
| 3 | 0.5 (± 0.2) | 4.5 (± 1.3) | 0.5 (± 0.5) |
| 4 | 0.3 (± 0.2) | 4.6 (± 1.3) | 0.2 (± 0.1) |
| Day . | CLL cells alone . | + Autologous stromal cells* . | + Autologous stromal cells + sCD100† . |
|---|---|---|---|
| 1 | 0.4 (± 0.1) | 1.6 (± 0.1) | 0.6 (± 1.4) |
| 3 | 0.5 (± 0.2) | 4.5 (± 1.3) | 0.5 (± 0.5) |
| 4 | 0.3 (± 0.2) | 4.6 (± 1.3) | 0.2 (± 0.1) |
Leukemic cells significantly enhanced their proliferative activity when cocultured with autologous Plexin-B1+ BM stromal cells in comparison with CLL cells alone (*P < .01). The effect on proliferation was significantly abolished by soluble CD100 (stromal cells + sCD100; †P < .05). Proliferation activity was measured by the evaluation of DNA content after PI staining. The numbers express the percentage of CLL cells in S, G2, M phases of the cell cycle and represent the mean values ± standard deviations obtained in 2 independent experiments.
Effects of soluble CD100 (sCD100) on CLL cells viability and proliferation
| . | CLL cells alone . | + sCD100 . | + MLP . | + MLP + sCD100 . | + MLP/Plex-B1 . | + MLP/Plex-B1 + sCD100 . |
|---|---|---|---|---|---|---|
| Viability | ||||||
| Day 3 | 62.5 (± 9.2) | 61.5 (± 14.8) | 70.5 (± 10.6) | 66 (± 8.5) | 93.5 (± 3.5) | 71 (± 5.7) |
| Day 5 | 59 (± 14.1) | 57.5 (± 19.1) | 73.3 (± 2.1) | 62 (± 19.8) | 94 (± 1.4) | 64 (± 4.2) |
| Proliferation | ||||||
| Day 3 | 1.1 (± 1.0) | 1 (± 0.7) | 1.6 (± 0.6) | 1.7 (± 0.3) | 5.6 (± 1.6) | 1.6 (± 0.8) |
| Day 5 | 1 (± 0.6) | 1 (± 0.7) | 1.7 (± 0.4) | 1.8 (± 0.3) | 6 (± 1.6) | 2 (± 0.9) |
| . | CLL cells alone . | + sCD100 . | + MLP . | + MLP + sCD100 . | + MLP/Plex-B1 . | + MLP/Plex-B1 + sCD100 . |
|---|---|---|---|---|---|---|
| Viability | ||||||
| Day 3 | 62.5 (± 9.2) | 61.5 (± 14.8) | 70.5 (± 10.6) | 66 (± 8.5) | 93.5 (± 3.5) | 71 (± 5.7) |
| Day 5 | 59 (± 14.1) | 57.5 (± 19.1) | 73.3 (± 2.1) | 62 (± 19.8) | 94 (± 1.4) | 64 (± 4.2) |
| Proliferation | ||||||
| Day 3 | 1.1 (± 1.0) | 1 (± 0.7) | 1.6 (± 0.6) | 1.7 (± 0.3) | 5.6 (± 1.6) | 1.6 (± 0.8) |
| Day 5 | 1 (± 0.6) | 1 (± 0.7) | 1.7 (± 0.4) | 1.8 (± 0.3) | 6 (± 1.6) | 2 (± 0.9) |
sCD100 was added to the cultures and its effects on viability and proliferation were evaluated by Annexin V and PI staining, respectively. The numbers express the percentage of viable cells and of cells in S, G2, M phases of the cell cycle and represent the mean values ± standard deviations obtained in 2 independent experiments.
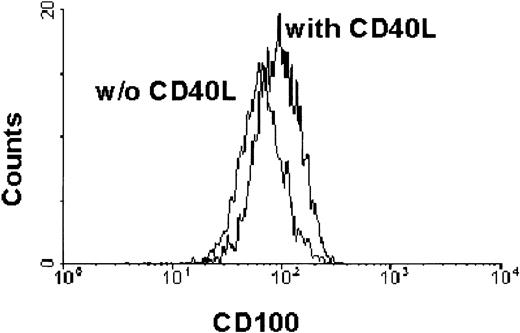
CD40 engagement increases CD100 expression and response to Plexin-B1 in CLL cells
As CD40L is an inducer of viability and proliferation of CLL cells,12-16 and as CD100 appeared to have similar effects, we asked how CLL cells would react in the presence of both stimuli.
We first investigated the possibility that CD40 stimulation might affect the expression of CD100, by culturing leukemic cells in the presence or absence of human soluble CD40L (sCD40L). The stimulation of CD40 up-regulated the expression of CD100 starting on day 3 of culture, with an MFI increasing by 21% compared with the unstimulated controls (Figure 5).
CLL expression of CD100 is up-regulated by CD40 stimulation.
Leukemic cells from CLL patients either unstimulated or stimulated with soluble CD40L were stained with PE–labeled anti-CD100 mAb and analyzed by flow cytometry. The analysis was performed gating on CD19+CD5+ cells and the level of CD100 expression was indicated as MFI.
CLL expression of CD100 is up-regulated by CD40 stimulation.
Leukemic cells from CLL patients either unstimulated or stimulated with soluble CD40L were stained with PE–labeled anti-CD100 mAb and analyzed by flow cytometry. The analysis was performed gating on CD19+CD5+ cells and the level of CD100 expression was indicated as MFI.
CD100/Plexin-B1 interactions extend viability and enhance proliferation also in normal CD19+CD5+cells
In order to evaluate whether CD100/Plexin-B1 interaction could also occur in a physiologic scenario, we analyzed CD19+CD5+ cells from 5 normal tonsils. CD19+CD5+ cells were found to be consistently CD100+ with an MFI range and a slight CD40-induced up-regulation superimposable to that of CLL cells. We performed coculture experiments with normal CD19+CD5+exposed to the same conditions described for CLL cells (media alone, wild-type MLP, or MLP/Plex-B1 cells in the presence or absence of sCD40L). As leukemic B cells, normal CD5+ B cells also showed an extended life span and an increased proliferation (Table7) when exposed to Plexin-B1 transfectants, suggesting that CD100/Plexin-B1 interactions also operate in normal CD5+ B cells. No statistically significant differences in terms of survival and proliferation were observed by the concomitant exposure of normal CD5+ B cells to Plexin-B1 and to sCD40L (Table 7).
CD19+CD5+ cell viability and proliferation are sustained by CD100/Plexin-B1 interaction
| . | CD19+CD5+ cells alone . | + MLP . | + MLP/Plex-B1* . | + CD40L . | + MLP + CD40L . | + MLP/Plex-B1 + CD40L . |
|---|---|---|---|---|---|---|
| Viability | ||||||
| Day 2 | 8 (± 10.8) | 38 (± 4.1) | 62 (± 3.9) | 32 (± 12.3) | 44 (± 7.1) | 68 (± 2.5) |
| Day 3 | 5 (± 9.4) | 34 (± 4.9) | 69 (± 3.2) | 18 (± 6.9) | 37 (± 8.4) | 72 (± 3.7) |
| Day 4 | 5 (± 7.6) | 32 (± 8.2) | 67 (± 4.5) | 20 (± 5.6) | 36 (± 7.3) | 71 (± 3.0) |
| Proliferation | ||||||
| Day 2 | 1.6 (± 0.3) | 2.8 (± 1.0) | 6.0 (± 1.8) | 3.2 (± 0.8) | 3.5 (± 1.1) | 6.4 (± 1.5) |
| Day 3 | 1.3 (± 0.4) | 3.2 (± 0.9) | 9.7 (± 1.4) | 1.6 (± 0.4) | 3.7 (± 1.4) | 7.0 (± 1.7) |
| Day 4 | 1.1 (± 0.2) | 3.3 (± 1.0) | 9.5 (± 1.6) | 1.7 (± 0.2) | 3.7 (± 1.2) | 7.2 (± 1.0) |
| . | CD19+CD5+ cells alone . | + MLP . | + MLP/Plex-B1* . | + CD40L . | + MLP + CD40L . | + MLP/Plex-B1 + CD40L . |
|---|---|---|---|---|---|---|
| Viability | ||||||
| Day 2 | 8 (± 10.8) | 38 (± 4.1) | 62 (± 3.9) | 32 (± 12.3) | 44 (± 7.1) | 68 (± 2.5) |
| Day 3 | 5 (± 9.4) | 34 (± 4.9) | 69 (± 3.2) | 18 (± 6.9) | 37 (± 8.4) | 72 (± 3.7) |
| Day 4 | 5 (± 7.6) | 32 (± 8.2) | 67 (± 4.5) | 20 (± 5.6) | 36 (± 7.3) | 71 (± 3.0) |
| Proliferation | ||||||
| Day 2 | 1.6 (± 0.3) | 2.8 (± 1.0) | 6.0 (± 1.8) | 3.2 (± 0.8) | 3.5 (± 1.1) | 6.4 (± 1.5) |
| Day 3 | 1.3 (± 0.4) | 3.2 (± 0.9) | 9.7 (± 1.4) | 1.6 (± 0.4) | 3.7 (± 1.4) | 7.0 (± 1.7) |
| Day 4 | 1.1 (± 0.2) | 3.3 (± 1.0) | 9.5 (± 1.6) | 1.7 (± 0.2) | 3.7 (± 1.2) | 7.2 (± 1.0) |
CD19+CD5+ B cells significantly sustained their viability and increased their proliferation when exposed to Plexin-B1 transfectants (MLP/Plex-B1) in comparison with MLP wild type (*P < .01). The coculture experiments were performed also in the presence of soluble CD40L (MLP or MLP/Plex-B1 + CD40L). Viability was assessed by cytofluorograph analysis of Annexin V staining and proliferation activity was measured by the evaluation of DNA content after PI staining. The numbers express the percentage of CD19+CD5+cells in S, G2, M phases of the cell cycle and represent the mean values ± standard deviations obtained in 5 independent experiments.
Discussion
In this work we have asked which mechanisms operate in the crosstalks between malignant B cells and bystander nontumoral cells and whether these mechanisms are malignancy-related or reproduce those used by their normal equivalent cells. To address these issues we have studied CLL, as there is compelling evidence that the relentless in vivo accumulation of CLL cells26 is under microenvironmental influence.1 CLL cells seed, grow, and accumulate within different microenvironments, namely BM and LN, where they come in close contact with different types of nontumoral bystander cells, like activated CD4+ T cells,9 BM stromal cells,3,4 and possibly also FDC.5Further, the distinctive cellular phenotype of CLL cells, that coexpress CD5 together with mature B-cell markers,26allows the comparison with CD19+CD5+ normal B cells.
While searching for a crosstalk molecule between CLL cells and the microenvironment, we reasoned that CD100 was an attractive candidate because of its role in the development of CD5+ B cells27 and its action in rescuing B cells from apoptosis.24
We demonstrate here that (1) CLL cells uniformly express CD100; (2) the CD100 high-affinity receptor Plexin-B1 is expressed by BM stromal cells, FDC, and activated T lymphocytes; (3) CD100+ CLL cells exposed in vitro to Plexin-B1 increase their proliferative activity and extend their life span; and (4) CD100/Plexin-B1 interactions sustain proliferation and survival also of CD19+CD5+ normal B cells.
These findings establish 3 major points. First, Plexin-B1 is a receptor for CD100 also within the immune system. In tissues as diverse as BM and peripheral lymphoid organs, Plexin-B1 entails crucial environmental elements that interact with B cells. Activated T cells, BM stromal cells, and FDC may all make Plexin-B1 available to B cells and through CD100/Plexin-B1 interactions enhance the proliferation and extend the life span of CD5+ B lymphocytes.
The second point is that the CD100+ leukemic cell encounter with Plexin-B1 in distinct microenvironments may represent a mechanism favoring the proliferation and survival of malignant B cells. As all leukemic cases are CD100+ and have the same type of response irrespective of their Ig VH mutational status, it follows that CD100/Plexin-B1 interaction may be a general mechanism favoring the expansion of leukemic clones. In leukemic CD5+B cells the antiapoptotic and proliferative response shown by CD100+ CLL cells exposed to Plexin-B1 reveals an interaction that is alternative to that possibly provided by the low-affinity receptor CD72. It has been suggested that CD100/CD72 interaction is an important pathway for B cell/B cell interaction of CD100+ B cells.28 Although CD72 is generally regarded as an inhibitory receptor, the possibility also exists that CD100 interaction with CD72 may have a stimulating effect.28 If CD72 is a negative regulator of B cells24 it might concur to confer to CLL cells their inert state.40 However, in a microenvironment where Plexin-B1 and CD72 coexist (eg, LN and BM) CD100 would preferentially interact with the high-affinity receptor Plexin-B1 and give rise to activation signals that lead to enhanced proliferation and survival of malignant cells.
The third point is that both normal and leukemic CD5+ B cells may use the CD100/Plexin-B1 system to interact with disparate microenvironmental elements in different tissues. Our data demonstrate that the CD100/Plexin-B1 interactions lead to increased proliferation and sustained viability not only of leukemic but also of normal CD5+ B cells and document the physiologic versatility of CD100 within the immune system. Therefore the crosstalk operated by the CD100/Plexin-B1 interactions is not malignancy related, rather it reproduces in leukemic CD5+ B cells the mechanism used by normal CD5+ B cells, reinforcing the concept that B-cell malignant clones take advantage of bystander nontumoral cells in their natural history.
Both Plexin-B1 and CD40L9 appear to be available to CLL cells in the different microenvironments where they accumulate in vivo. The signals delivered to normal B lymphocytes by activated T cells through CD40L induce B-cell growth, differentiation, and rescue from apoptosis.41,42 CD40 stimulation of CLL cells has been shown in vitro to prevent apoptosis and to induce the malignant cell proliferation.12-16 However, transfection of CLL cells with CD40L leads to improved stimulation and killing by activated T cells,43 and costimulation of CLL cells with IL-15, CD40, and CD95 cross-linking may promote CLL cell death.44 It is plausible to consider that the role of CD40 stimulation may rely highly on the context of specific cell types in the microenvironment where CLL cells gather, the activation status of T cells, and the release of cytokines in close proximity of CLL cells. The concomitant in vivo exposure of CLL cells to CD40L and to CD100 high-affinity receptor within specific microenvironments may favor the malignant cell survival and proliferation.
The data presented here suggest that the interruption of the CD100-mediated interactions between leukemic CD5+ B cells and microenvironmental bystander nontumoral cells might provide a new therapeutic approach that needs to be explored. Further, considering that one of the most puzzling features of CLL is the development of autoimmune manifestations and that a role has been suggested for CD100 in autoimmune diseases,45 the possible involvement of CD100 in these unexplained events also warrants further investigation.
We thank Luca Tamagnone for helpful discussion and suggestions; and Simona Corso, Paolo Conrotto, and Sergio Anguissola for kindly providing the transfected cell lines.
Prepublished online as Blood First Edition Paper, October 24, 2002; DOI 10.1182/blood-2002-05-1339.
Supported by Associazione Italiana per la Ricerca sul Cancro (AIRC), Ministero dell' Universita' e della Ricerca Scientifica e Tecnologica (MURST) 40%, 60% and Consiglio Nazionale delle Ricerche (CNR) Progetto Finalizzato (PF) Biotecnologie.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Federico Caligaris-Cappio, Ospedale Mauriziano Umberto I, Largo Turati 62, 10128 Torino, Italy; e-mail:fcaligaris@mauriziano.it.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal