Activated platelets release angiogenic growth factors and have therefore been proposed to contribute to tumor angiogenesis within a potentially prothrombotic tumor microcirculation. The aim of the study was to investigate interactions of platelets with the angiogenic microvascular endothelium of highly vascularized solid tumors during growth and in response to endothelial stimulation in comparison with normal subcutaneous tissue. Experiments were performed in the dorsal skinfold chamber preparation of C57BL/6J mice bearing the Lewis lung carcinoma (LLC-1) or methylcholanthrene-induced fibrosarcoma (BFS-1). Fluorescently labeled rolling and adherent platelets, red blood cell velocity, and vessel diameters were assessed by intravital fluorescence microscopy on days 1, 3, 8, and 14 after tumor cell implantation. Slightly elevated numbers of rolling platelets were observed in the early stages of tumor angiogenesis at day 1 (control, 1.7 ± 0.6; LLC-1, 3.4 ± 1.8; BFS-1, 3.0 ± 0.7 [1/mm/s],P < .05) and day 3 (control, 1.6 ± 0.6; LLC-1, 4.1 ± 1.7, P < .05; BFS-1, 2.3 ± 0.5 [1/mm/s]) after tumor cell implantation. Endothelial stimulation with calcium ionophore A23187 at day 14 after tumor cell implantation resulted in a minor increase to 2.1 ± 0.4 (LLC-1) and 1.8 ± 0.8 (BFS-1) rolling platelets (1/mm/s) in tumor microvessels compared with 4.9 ± 0.9 in controls (P < .05). Platelet adherence was not observed. We therefore conclude that in the 2 experimental tumors under study, (1) slightly increased platelet rolling is a transient phenomenon after tumor cell implantation, and (2) platelet-endothelial interaction in response to endothelial stimulation is reduced in tumor microvessels.
Introduction
Abnormalities in blood coagulation and fibrinolysis are a frequently recognized epiphenomenon of malignancies. The result can be vascular thrombosis and thromboembolic complications in cancer patients.1 Furthermore, thromboembolic complications are a potential first sign of occult malignancy.2 In a high percentage of cancer patients, laboratory parameters indicate activated coagulation and fibrinolysis characterized by elevated plasma concentrations of clotting factors, fibrinogen, and fibrin/fibrinogen degradation products. The incidence of thrombocytosis may be explained as overcompensation in response to proceeding low-grade disseminated intravascular coagulation and thrombocytolysis. Thrombocytopenia is less frequent, mostly related to chemotherapy or linked to increased platelet destruction or in vivo platelet activation and release. Tumor cells themselves exert a high prothrombotic potential by directly activating blood coagulation and releasing cytokines and growth factors to their environment.1,3 Finally, activation of blood coagulation may be favored within heterogeneous tumor microcirculation: solid tumors are characterized by compromised tissue perfusion with local areas of hypoxia, sluggish blood flow, and mosaic vessels with nonendothelial cells participating in formation of vascular lumen.4-6
Activated blood coagulation has been linked to the process of tumor angiogenesis since relevant clotting factors were found to exert potent regulatory functions on endothelial proliferation. Particularly tissue factor, expressed in tumor cells, regulates synthesis of the endothelial cell–specific growth factor vascular endothelial growth factor (VEGF) by its cytoplasmic domain.7Tumor-derived VEGF induces tissue factor expression in endothelial cells, resulting in enhanced thrombin formation. Thrombin is a potent mitogen of endothelial cells, which are induced to secrete growth factors and express both VEGF receptors, fetal liver kinase 1 (flk-1) and fms-like tyrosine kinase 1 (flt-1).8 Also, thrombin activates progelatinase A and initiates formation of intravascular and extravascular fibrin meshes at sites of angiogenesis.9 Fibrin meshes provide a provisional matrix for sprouting vessels and preserve angiogenic growth factors.10 Components of the hemostatic system and its side products can also suppress and antagonize angiogenesis.11 One well-known antiangiogenic factor of the hemostatic system is angiostatin, which is generated by proteolytic degradation of plasminogen.12
Besides the plasmatic factors of blood coagulation, platelets are increasingly considered to be involved in angiogenic processes. First evidence is based on in vitro observations of platelets preserving endothelial cell cultures and promoting formation of capillarylike structures in a matrigel assay.13,14 These early studies forwarded the identification of proangiogenic and antiangiogenic growth factors, for example VEGF and angiopoietin-1, stored at least partly in the α-granules of platelets.11,15 Furthermore, platelets are a rich source of phospholipids to which endothelial cells respond with angiogenic transformation. The 3 angiogenic phospholipids lysophosphatidate, phosphatidic acid, and sphingosin 1–phosphate express mitogenic activity and stimulate liberation of endothelial cells from established monolayers, chemotactic migration, proliferation, adherence, junction assembly, and morphogenesis into capillarylike structures.16 First in vivo experiments demonstrate that sphingosin 1–phosphate intensifies the angiogenic effect of basic fibroblast growth factor (FGF) in the avascular mouse cornea.17 So far, in vitro experiments have provided the evidence that angiogenic growth factors and phospholipids are released upon activation and aggregation of platelets.16 18
On the basis of the observation of activated blood coagulation accompanying malignancies, sluggish blood flow, and vascular hyperpermeability in tumor microcirculation, Pinedo et al19 proposed that platelets become activated and release angiogenic factors by forming microthrombi at sites of tumor growth. The aim of the present in vivo study was therefore to visualize platelets in the microcirculation of tumors and to quantify interactions of platelets with the endothelial lining of microvessels undergoing an angiogenic change in the course of tumor growth. In a second approach, the capability of tumor microvessels to accumulate platelets on their endothelial surface in response to stimulation should be investigated. Our results provide evidence that tumor angiogenesis is accompanied by a transient slight increase in platelet rolling. We further propose a reduced capability of tumor microvessels to promote platelet accumulation on their luminal surface.
Materials and methods
Animals
Male C57BL/6J mice (Charles River, Sulzfeld, Germany), aged 6 to 8 weeks (20 to 25 g body weight) were used as experimental animals and platelet donors. The animals were housed in single cages and had free access to water and standard laboratory food throughout the experiments. Following tumor cell implantation, mice were kept in an intensive-care incubator (7510; Draeger-Werk, Lübeck, Germany) at 32°C and 50% relative humidity for the first 4 days and thereafter at room temperature. All experimental procedures performed on mice were approved by the German legislation on protection of animals.
Surgical procedure and tumor cell implantation
Dorsal skinfold chambers and surgical preparation were performed as previously described, with minor modifications.6 20 Briefly, the mice were anesthetized by intramuscular injection of ketamin-xylazine (75 mg/kg body weight [Ketavet, 100 mg/mL; Pharmacia and Upjohn, Erlangen, Germany] and 25 mg/kg body weight [Rompun, 2%; Bayer, Leverkusen, Germany]). The hair was removed from the back of the animals, and 2 symmetric titanium frames were positioned to sandwich the extended double layer of skin of the dorsal skinfold. One layer of skin was completely removed in a circular area of 15 mm in diameter, and the remaining layers, consisting of the epidermis, subcutaneous tissue, and striated skin muscle, were covered with a glass coverslip that was incorporated into one of the frames.
After a 48-hour recovery period from anesthesia and microsurgery, chambers fulfilling the criteria of an intact microcirculation were used for implantation of 1 × 105 cells of 1 of 2 different syngenic tumors of the C57BL/6J mouse. Tumor cell lines LLC-1 generated from the primary Lewis lung carcinoma21 were purchased from the European Collection of Cell Cultures (Salisbury, United Kingdom), and tumor cell line BFS-1 of the methylcholanthrene-induced fibrosarcoma22 was kindly provided by Professor Clauss (Max-Plank-Institute Bad Nauheim, Germany). Tumor-free chamber preparations served as controls. The animals tolerated the dorsal skinfold chambers well and showed no signs of discomfort.
Blood sampling and platelet preparation
Separation and ex vivo fluorescent labeling of platelets was based on a previously described protocol.23 The method has been further improved by the use of a different fluorescent marker that provides long-term visualization of individual platelets and their interaction with the endothelial lining in normal and tumor microcirculation in vivo. For each experiment, 1 mL blood was harvested from a syngenic donor mouse by cardiac puncture and collected in polypropylene tubes containing 0.2 mL volume of 38 mM citratic acid, 75 mM trisodium citrate, and 100 mM dextrose; 20 μL prostaglandin E1 (PGE1) (650 nM final concentration) (Serva, Heidelberg, Germany); and 0.5 mL Dulbecco phosphate-buffered saline (D-PBS) (PAN Systems, Aidenbach, Germany). Blood was centrifuged at 130g for 10 minutes. Platelet-rich plasma was gently transferred to a fresh tube, containing 1.5 mL D-PBS (PAN Systems); 0.3 mL volume of 38 mM citratic acid, 75 mM trisodium citrate, and 100 mM dextrose; and 50 μL PGE1 (940 nM final concentration) (Serva). The fluorescent marker aminoreactive succinimidylester carboxyfluorescein-diacetat (CFDA-SE) (molecular weight [MW] 535) (Molecular Probes, Eugene, OR) was added to platelet-rich plasma, and centrifugation was repeated immediately at 1430g for 10 minutes. The resulting platelet pellet was resuspended in 0.4 mL D-PBS (PAN Systems). The platelet concentration and purity of the sample were measured by means of a Coulter ACT Counter (Coulter, Miami, FL). Experimental animals received a total of 100 × 106 fluorescently labeled platelets transfused via the lateral tail vein, corresponding to approximately 10% of all circulating platelets.24
Adequate functionality of fluorescently labeled platelets has been evaluated by flow cytometric analysis (FACSort flow cytometer; Becton Dickinson, Heidelberg, Germany) before and following in vitro activation by adenosine diphosphate (ADP) (100μM) (Sigma-Aldrich, Deisenhofen, Germany) and varying concentrations of human thrombin (0.05 U/mL, 0.5 U/mL, 5 U/mL) (Sigma-Aldrich) for 10 minutes. In addition, platelet function was examined by aggregometry (Aggregometer 2K-AGGR 126; Labor, Hamburg, Germany) in response to stimulation with 2 U/mL human thrombin (Sigma-Aldrich).
Intravital fluorescence microscopy
The awake animals were immobilized in a Plexiglas tube attached to a computer-controlled microscope stage to allow relocation and repeated observation of identical microvessel segments.25The microvasculature was observed by means of a 20-fold water immersion objective (total magnification × 460) (Zeiss Axiotech vario 100 HD microscope, Acroplan 20 × /0.5 W; Zeiss, Oberkochen, Germany) under epi-illumination (100-W HBO mercury vapor lamp; Zeiss). The images obtained with a charge coupled device–camera (FK 6990 IQ-S; Piper, Schwerte, Germany) were recorded on S-VHS videotape (video recorder SVO-9500 MDP; Sony, Cologne, Germany) for later offline analysis. Imaging of microvasculature and blood plasma flow was achieved by high–molecular-weight amino-dextran (2%, MW 500 000) (Molecular Probes) fluorescently labeled with aminoreactive carboxytetramethylrhodamin-succinimidylester (5-TAMRA-SE) (MW 528) (Molecular Probes). CFDA-labeled platelets (100 × 106) and TAMRA-dextran (2 mL/kg body weight) were infused via the lateral tail vein. The use of different fluorescence filter sets allowed selective visualization of either CFDA-labeled platelets or blood plasma labeled by TAMRA-dextran.
Video analysis
Video images were analyzed during playback by means of a computer-assisted image analysis system (CAP IMAGE; Dr H. Zeintl, Heidelberg, Germany).26 From the TAMRA-dextran images, the vessel diameter (in micrometers) and centerline red blood cell (RBC) velocity (millimeters per second) were determined. Wall shear rate (γ) was calculated on the basis of the Newtonian definition: γ = 8 × V × D−1[s−1], where V represents the mean red blood cell velocity ( = centerline velocity × 1.6),27 and D the diameter of individual microvessels.
Platelets were classified according to their interaction with the endothelial lining as free flowing, rolling, or adherent cells.23 Rolling platelets were defined as cells crossing an imaginary perpendicular through the vessel under study at a velocity significantly lower than the centerline velocity in the microvessel; their numbers are given as cells per vessel diameter per second (1/mm/s). Adherent platelets were defined as cells that did not move or detach from the endothelial lining in a vessel segment of 100-μm length within an observation period of 30 seconds. Adherence was quantified as number of cells per square millimeter of endothelial surface (1/mm2).
Experimental protocol
In the first series of experiments, microhemodynamic parameters and platelets were investigated at consecutive stages of tumor angiogenesis in comparison with normal tissue. Therefore, intravital microscopy was performed on days 1, 3, 8, and 14 after implantation of LLC-1 and BFS-1 tumor cells. Preselected postcapillary venules in tumor-free chamber preparations of control animals underwent intravital microscopy on corresponding days. Tortuous and slightly dilated angiogenic blood vessels of the host were investigated on the edge of implanted tumor cells on day 1; first newly formed tumor vessels were investigated within the developing tumor stroma on day 3 after tumor cell implantation. A well-vascularized tumor microcirculation had established and was evaluated on days 8 and 14. Six animals were included per group at each day of measurement.
In the second series of experiments, possible induction of platelet interaction with the microvascular endothelium of LLC-1 (n = 6) and BFS-1 tumors (n = 6) was evaluated on day 14 after tumor cell implantation. After baseline measurements were performed, the glass coverslip of the chamber preparation was removed, and calcium ionophore A23187 (3 × 100 μL of a 20 μM solution; Sigma-Aldrich) was superfused over 15 minutes. Intravital microscopy was repeated immediately after insertion of a new cover glass. As in the first set of experiments, postcapillary venules in tumor-free chamber preparations (n = 6) served as controls.
Only microvessels of similar diameters (18 to 25 μm) showing continuous blood flow were studied in both series of experiments. Throughout the experimental groups, microcirculatory parameters and platelet rolling and adhesion were analyzed within 6 to 8 microvessels per animal.
Statistics
All results are given as median ± standard error of the median. Data analysis was performed with a statistical software package (SigmaStat for Windows; SPSS Science, Chicago, IL). Kruskal-Wallis test followed by Dunn method was used for the estimation of stochastic probability in intergroup comparison, and Wilcoxon test was used for estimation of stochastic probability in intragroup comparison. P < .05 was considered significant.
Results
Ex vivo labeling of platelets
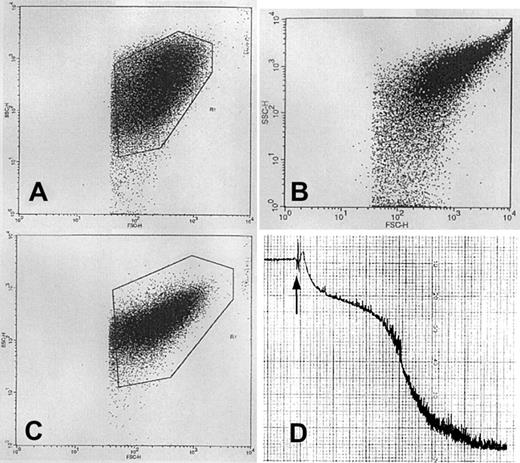
We used the methods originally described and validated by Massberg et al23 for intravital microscopy of platelet-endothelium interaction, modified by the use of carboxyfluorescein-diacetate (CFDA) instead of Rhodamine 6G as fluorescent dye for long-term visualization of platelets within the microcirculation of tumors and tumor-free tissues. The procedure for separation and CFDA labeling of platelets from C57BL/6J mice was carefully evaluated by fluorescence-activated cell sorter (FACS) analysis, platelet aggregometry, and in vivo experiments to assure adequate functionality of labeled platelets. In FACS analysis, fluorescently labeled platelets described a distinct population in log forward/log side light scatter, which shifted toward higher granularity and size after activation by ADP and human thrombin (Figure 1A-C). FACS analysis therefore proved that platelet aggregation is induced by weak agonist ADP and even low concentrations of human thrombin. Hence, platelet function was not impaired by the sampling and labeling procedure. This has been further confirmed by aggregometry, which revealed biphasic aggregation of fluorescently labeled platelets in response to human thrombin (Figure 1D). In vivo, platelet aggregation was evaluated in response to intestinal ischemia/reperfusion (90 minutes ischemia and 30 minutes reperfusion). Intravital fluorescence microscopy of small intestinal microvessels demonstrated massive and comparable interaction and aggregation of CFDA and rhodamine-labeled platelets in arterioles and postcapillary venules in vivo.
Assessment of platelet functionality following separation and fluorescent labeling.
(A-C) Log forward/log side light scatter FACS analysis of CFDA-labeled platelets demonstrates a distinct population of unstimulated platelets (A). Platelet aggregation demonstrates a shift of the platelet population toward higher granularity and size in response to weak agonist ADP (100 μM; panel B) and low concentrations of human thrombin (0.05 U/mL; panel C). (D) Aggregometry of CFDA-labeled platelets revealed biphasic platelet aggregation in response to 2 U/mL human thrombin.
Assessment of platelet functionality following separation and fluorescent labeling.
(A-C) Log forward/log side light scatter FACS analysis of CFDA-labeled platelets demonstrates a distinct population of unstimulated platelets (A). Platelet aggregation demonstrates a shift of the platelet population toward higher granularity and size in response to weak agonist ADP (100 μM; panel B) and low concentrations of human thrombin (0.05 U/mL; panel C). (D) Aggregometry of CFDA-labeled platelets revealed biphasic platelet aggregation in response to 2 U/mL human thrombin.
Microhemodynamic parameters of growing tumors
Results of the microhemodynamic parameters during tumor growth and angiogenesis are summarized in Table 1. Microvessels having diameters from 18 to 25 μm were most frequently found within the microcirculation of both tumors. Therefore, tumor and normal microvessels of similar diameters were included to facilitate comparability of different tissue microvessels.
Microhemodynamic parameters during the first 14 days of tumor growth
| Parameter . | Day . | |||
|---|---|---|---|---|
| 1 . | 3 . | 8 . | 14 . | |
| Vessel diameter, μm | ||||
| Controls | 20.2 ± 0.6 | 20.2 ± 0.8 | 21.0 ± 1.0 | 22.0 ± 0.7*,† |
| LLC-1 | 23.0 ± 2.0‡ | 17.7 ± 2.9 | 22.0 ± 3.0 | 22.0 ± 0.5 |
| BFS-1 | 21.5 ± 0.6 | 19.1 ± 0.4* | 21.1 ± 1.1 | 20.0 ± 0.8‡1-153 |
| RBC velocity, mm/s | ||||
| Controls | 0.32 ± 0.02 | 0.38 ± 0.07 | 0.35 ± 0.06 | 0.34 ± 0.05 |
| LLC-1 | 0.14 ± 0.04‡1-155 | 0.18 ± 0.05‡1-155 | 0.18 ± 0.09‡ | 0.28 ± 0.02*,† |
| BFS-1 | 0.25 ± 0.03 | 0.34 ± 0.04* | 0.25 ± 0.03† | 0.25 ± 0.02 |
| Wall shear rate, s−1 | ||||
| Controls | 122.0 ± 8.3 | 142.3 ± 32.3 | 134.4 ± 29.5 | 112.5 ± 19.0 |
| LLC-1 | 57.9 ± 12.5‡1-155 | 73.9 ± 25.8‡1-155 | 66.7 ± 24.4‡ | 98.5 ± 8.3*,† |
| BFS-1 | 86.6 ± 37.3 | 142.5 ± 20.2* | 94.3 ± 15.3† | 93.8 ± 9.3 |
| Parameter . | Day . | |||
|---|---|---|---|---|
| 1 . | 3 . | 8 . | 14 . | |
| Vessel diameter, μm | ||||
| Controls | 20.2 ± 0.6 | 20.2 ± 0.8 | 21.0 ± 1.0 | 22.0 ± 0.7*,† |
| LLC-1 | 23.0 ± 2.0‡ | 17.7 ± 2.9 | 22.0 ± 3.0 | 22.0 ± 0.5 |
| BFS-1 | 21.5 ± 0.6 | 19.1 ± 0.4* | 21.1 ± 1.1 | 20.0 ± 0.8‡1-153 |
| RBC velocity, mm/s | ||||
| Controls | 0.32 ± 0.02 | 0.38 ± 0.07 | 0.35 ± 0.06 | 0.34 ± 0.05 |
| LLC-1 | 0.14 ± 0.04‡1-155 | 0.18 ± 0.05‡1-155 | 0.18 ± 0.09‡ | 0.28 ± 0.02*,† |
| BFS-1 | 0.25 ± 0.03 | 0.34 ± 0.04* | 0.25 ± 0.03† | 0.25 ± 0.02 |
| Wall shear rate, s−1 | ||||
| Controls | 122.0 ± 8.3 | 142.3 ± 32.3 | 134.4 ± 29.5 | 112.5 ± 19.0 |
| LLC-1 | 57.9 ± 12.5‡1-155 | 73.9 ± 25.8‡1-155 | 66.7 ± 24.4‡ | 98.5 ± 8.3*,† |
| BFS-1 | 86.6 ± 37.3 | 142.5 ± 20.2* | 94.3 ± 15.3† | 93.8 ± 9.3 |
At the first day after tumor cell implantation, pre-existing venules on the edge of implanted tumor cells were included in the intravital microscopic studies, whereas newly developed tumor microvessels were observed on the following days. Subcutaneous venules of tumor-free chamber preparations served as controls. Wall shear rate was calculated from vessel diameter and red blood cell (RBC) velocity of individual microvessels. Data are given as the median ± standard error of the median; n = 6 experimental animals per group. P values are according to the Kruskal-Wallis test.
P < .05 versus day 1.
P < .05 versus day 3.
P < .05 versus controls.
P < .05 versus LLC-1.
P < .05 versus BFS-1.
RBC velocity was regularly reduced in tumor microvessels as compared with postcapillary venules of controls. At days 1, 3, and 8 after tumor cell implantation, microvessels of LLC-1 tumors showed values significantly below those of controls. Until day 14, RBC velocity increased in LLC-1 tumors but remained below RBC velocity of controls. A temporary increase in RBC velocity was recognized in BFS-1 tumors on day 3; the increase did not persist until subsequent observations. Comparison of tumors revealed a slightly higher RBC velocity within the microcirculation of BFS-1 than of LLC-1 tumors, especially in early stages of tumor angiogenesis.
Platelet rolling and adhesion are influenced by wall shear rate in the way that a high wall shear rate favors platelet-endothelial interaction.28 Therefore, this parameter was calculated from the diameter and RBC velocity of individual microvessels. Because of similar diameters of the individual microvessels, wall shear rate behaved like RBC velocity over the 14-day period, demonstrating reduced values for tumor microvessels. Lowest shear rate values were found in microvessels of LLC-1 tumors; these were significantly below those present in microvessels of normal tissue on days 1, 3, and 8 and BFS-1 tumors on days 1 and 3.
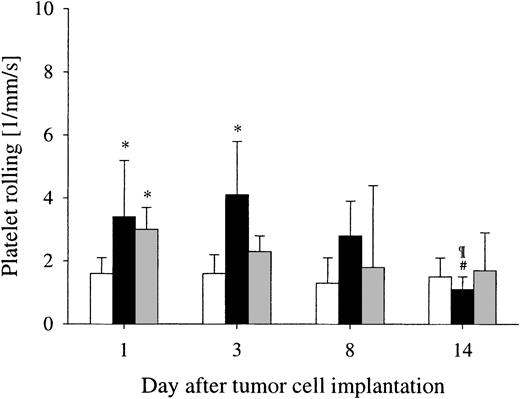
Platelet-endothelial interaction within the microcirculation of growing tumors
Platelet rolling occurred constantly on a low baseline level in postcapillary venules of normal tissue over the 14-day period. In the early stages of tumor growth and angiogenesis of LLC-1 and BFS-1 tumors, slightly enhanced interactions of platelets with the microvascular endothelium was observed as compared with postcapillary venules in normal tissue (Figures 2 and3). On the first day after implantation of LLC-1 and BFS-1 tumor cells, a significantly enhanced number of rolling platelets were found in pre-existing host vessels adjacent to tumor cells marked by a slight vasodilation and kinking in response to tumor cell–derived growth factors and cytokines. In newly developed tumor microvessels of LLC-1 tumors at day 3, a significantly enhanced number of rolling platelets were quantified, in contrast to BFS-1 tumors and controls. Highly vascularized LLC-1 and BFS-1 tumors at days 8 and 14 exhibited low numbers of rolling platelets on the endothelial lining of tumor microvessels in a range similar to that observed in postcapillary venules of controls. Adherence of platelets to the microvascular endothelium was not observed in either angiogenic vessels or normal postcapillary venules over the 14-day period.
Platelet-endothelial interaction during tumor angiogenesis.
Platelet-endothelial interaction is not an intense phenomenon during tumor angiogenesis. Platelet rolling was increased on day 1 in pre-existing microvessels of the host in response to both LLC-1 (▪) and BFS-1 ( ) and also on day 3 in LLC-1 tumor microvessels, but was only slightly above the low baseline level quantified in postcapillary venules of controls (■). Median ± standard error of the median; n = 6 experimental animals per group. *P < .05 versus controls; #P < .05 versus day 1; ¶P < .05 versus day 3 (Kruskal-Wallis test).
) and also on day 3 in LLC-1 tumor microvessels, but was only slightly above the low baseline level quantified in postcapillary venules of controls (■). Median ± standard error of the median; n = 6 experimental animals per group. *P < .05 versus controls; #P < .05 versus day 1; ¶P < .05 versus day 3 (Kruskal-Wallis test).
Platelet-endothelial interaction during tumor angiogenesis.
Platelet-endothelial interaction is not an intense phenomenon during tumor angiogenesis. Platelet rolling was increased on day 1 in pre-existing microvessels of the host in response to both LLC-1 (▪) and BFS-1 ( ) and also on day 3 in LLC-1 tumor microvessels, but was only slightly above the low baseline level quantified in postcapillary venules of controls (■). Median ± standard error of the median; n = 6 experimental animals per group. *P < .05 versus controls; #P < .05 versus day 1; ¶P < .05 versus day 3 (Kruskal-Wallis test).
) and also on day 3 in LLC-1 tumor microvessels, but was only slightly above the low baseline level quantified in postcapillary venules of controls (■). Median ± standard error of the median; n = 6 experimental animals per group. *P < .05 versus controls; #P < .05 versus day 1; ¶P < .05 versus day 3 (Kruskal-Wallis test).
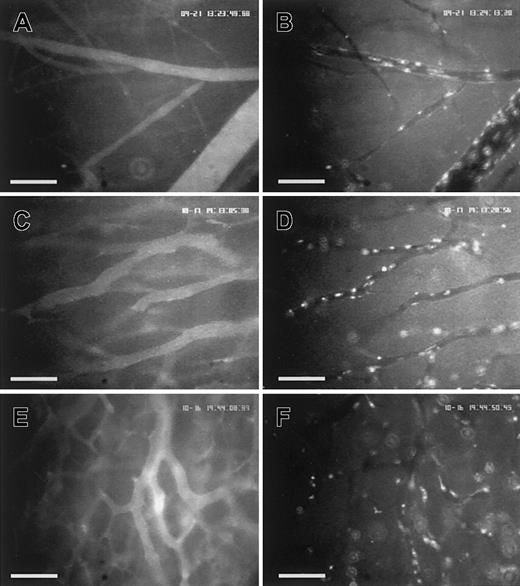
Visualization of platelets within the microcirculation of postcapillary venules and tumor microvessels in vivo.
The photographs of the intravital fluorescence microscopy demonstrate postcapillary venules of tumor-free striated skin muscle (A-B) and tumor microvessels of LLC-1 (C-D) and BFS-1 (E-F) tumors on day 14 after tumor cell implantation. Imaging of microvasculature and blood plasma flow was achieved after intravenous application of TAMRA-dextran (A,C,E). CFDA-labeled platelets were distributed homogeneously within the microcirculation of the different tissues (B,D,F). Assessment and quantification of platelet-endothelial interaction were performed during playback of the recorded video images. Scale bars represent 100 μm.
Visualization of platelets within the microcirculation of postcapillary venules and tumor microvessels in vivo.
The photographs of the intravital fluorescence microscopy demonstrate postcapillary venules of tumor-free striated skin muscle (A-B) and tumor microvessels of LLC-1 (C-D) and BFS-1 (E-F) tumors on day 14 after tumor cell implantation. Imaging of microvasculature and blood plasma flow was achieved after intravenous application of TAMRA-dextran (A,C,E). CFDA-labeled platelets were distributed homogeneously within the microcirculation of the different tissues (B,D,F). Assessment and quantification of platelet-endothelial interaction were performed during playback of the recorded video images. Scale bars represent 100 μm.
Calcium ionophore A23187 did not affect microhemodynamic parameters
Platelet interaction within tumor microcirculation following endothelial stimulation was evaluated on day 14 after tumor cell implantation. Damages and hemorrhagic bleeding of tumor and normal tissue were carefully prevented. As summarized in Table2, superfusion of tumor-free preparations and tumor tissue with calcium ionophore A23187 for 15 minutes did not provoke significant changes in microhemodynamics of normal or tumor tissue. Evaluation of microvessels of similar diameters ensured comparability of microhemodynamic parameters of different tissues. In both highly vascularized tumors, RBC velocity was still lower than in postcapillary venules of controls. A tendency of further RBC velocity reduction after application of calcium ionophore A23187 was noted in microvessels of LLC-1 tumors, while microcirculation of normal tissue and BFS-1 tumors remained unaffected. In consequence, wall shear rate was slightly reduced in microvessels of LLC-1 tumors in response to calcium ionophore A23187 and stayed at baseline values in microvessels of BFS-1 tumors and normal tissue. RBC velocity and wall shear rate in postcapillary venules of normal tissue exceeded parameters of tumor microcirculation in both baseline and treatment conditions.
Calcium ionophore A23187 exerts no profound effects on microhemodynamic parameters
| Parameter . | Baseline . | Ionophore . |
|---|---|---|
| Vessel diameter, μm | ||
| Controls | 20.4 ± 0.8 | 20.3 ± 0.5 |
| LLC-1 | 22.0 ± 0.5* | 22.3 ± 1.2* |
| BFS-1 | 20.0 ± 0.8† | 19.3 ± 0.2*,† |
| RBC velocity, mm/s | ||
| Controls | 0.33 ± 0.03 | 0.3 ± 0.06 |
| LLC-1 | 0.28 ± 0.02* | 0.23 ± 0.02* |
| BFS-1 | 0.25 ± 0.08* | 0.25 ± 0.02* |
| Wall shear rate, s−1 | ||
| Controls | 126.9 ± 13.8 | 119.7 ± 19.6 |
| LLC-1 | 98.5 ± 8.3* | 82.9 ± 4.7* |
| BFS-1 | 93.8 ± 9.3* | 103.7 ± 9.4† |
| Parameter . | Baseline . | Ionophore . |
|---|---|---|
| Vessel diameter, μm | ||
| Controls | 20.4 ± 0.8 | 20.3 ± 0.5 |
| LLC-1 | 22.0 ± 0.5* | 22.3 ± 1.2* |
| BFS-1 | 20.0 ± 0.8† | 19.3 ± 0.2*,† |
| RBC velocity, mm/s | ||
| Controls | 0.33 ± 0.03 | 0.3 ± 0.06 |
| LLC-1 | 0.28 ± 0.02* | 0.23 ± 0.02* |
| BFS-1 | 0.25 ± 0.08* | 0.25 ± 0.02* |
| Wall shear rate, s−1 | ||
| Controls | 126.9 ± 13.8 | 119.7 ± 19.6 |
| LLC-1 | 98.5 ± 8.3* | 82.9 ± 4.7* |
| BFS-1 | 93.8 ± 9.3* | 103.7 ± 9.4† |
Experiments were performed on highly vascularized tumors 14 days after tumor cell implantation and on subcutaneous venules within tumor-free chamber preparations of controls. Data are given as the median ± standard error of the median; n = 6 experimental animals per group. P values are according to the Kruskal-Wallis test.
P < .05 versus controls.
P < .05 versus LLC-1.
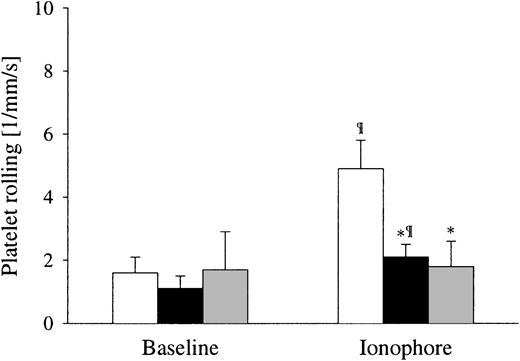
Calcium ionophore A23187 had only slight effects on platelet interaction with tumor microvessels
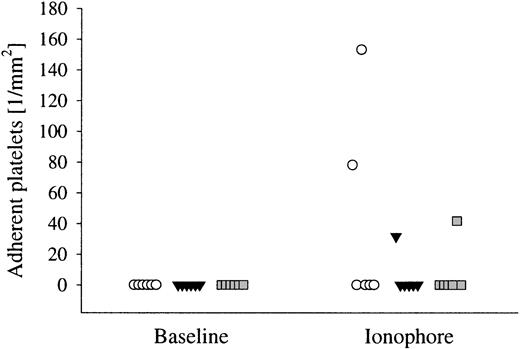
Before superfusion of tissues with calcium ionophore A23187, no differences were observed between normal and tumor microcirculation in the number of rolling platelets, with both types of microcirculation showing a low baseline number of rolling platelets. The most prominent effects of calcium ionophore A23187 occurred on postcapillary venules of the striated muscle, resulting in a 3-fold increase in the number of rolling platelets (Figure 4). No effect could be detected in microvessels of BFS-1 tumors, while a 2-fold increase in the number of rolling platelets was induced in microvessels of LLC-1 tumors. Adherence of platelets to the endothelial lining was observed only sporadically within the microcirculation of individual animals (Figure5). Similar to the findings of platelet rolling, adherence occurred more intensely in postcapillary venules of 2 animals of the control group and to a minor extent in tumor microvessels of 1 LLC-1 and 1 BFS-1 tumor–bearing animal.
Effect of calcium ionophore A23187 on platelet rolling.
Calcium ionophore A23187 induces platelet rolling favorably in normal and less in tumor microvessels. Superfusion of tumor tissues with calcium ionophore A23187 (20 μM) for 15 minutes causes a 2-fold increase of rolling platelets in LLC-1 (▪) and exerts no effects on BFS-1 ( ) on day 14 after tumor cell implantation. In contrast, treatment of tumor-free preparations resulted in a 3-fold increase of rolling platelets in postcapillary venules of controls (■) on corresponding days compared with tumor groups after chamber preparation. Median ± standard error of the median; n = 6 experimental animals per group, *P < .05 versus controls; ¶P < .05 versus baseline (Kruskal-Wallis and Wilcoxon tests).
) on day 14 after tumor cell implantation. In contrast, treatment of tumor-free preparations resulted in a 3-fold increase of rolling platelets in postcapillary venules of controls (■) on corresponding days compared with tumor groups after chamber preparation. Median ± standard error of the median; n = 6 experimental animals per group, *P < .05 versus controls; ¶P < .05 versus baseline (Kruskal-Wallis and Wilcoxon tests).
Effect of calcium ionophore A23187 on platelet rolling.
Calcium ionophore A23187 induces platelet rolling favorably in normal and less in tumor microvessels. Superfusion of tumor tissues with calcium ionophore A23187 (20 μM) for 15 minutes causes a 2-fold increase of rolling platelets in LLC-1 (▪) and exerts no effects on BFS-1 ( ) on day 14 after tumor cell implantation. In contrast, treatment of tumor-free preparations resulted in a 3-fold increase of rolling platelets in postcapillary venules of controls (■) on corresponding days compared with tumor groups after chamber preparation. Median ± standard error of the median; n = 6 experimental animals per group, *P < .05 versus controls; ¶P < .05 versus baseline (Kruskal-Wallis and Wilcoxon tests).
) on day 14 after tumor cell implantation. In contrast, treatment of tumor-free preparations resulted in a 3-fold increase of rolling platelets in postcapillary venules of controls (■) on corresponding days compared with tumor groups after chamber preparation. Median ± standard error of the median; n = 6 experimental animals per group, *P < .05 versus controls; ¶P < .05 versus baseline (Kruskal-Wallis and Wilcoxon tests).
Effect of calcium ionophore A23187 on platelet adherence.
Adherence of platelets occurs irregularly after application of calcium ionophore A23187. Platelet adhesion could be observed in individual experimental animals 15 minutes after application of calcium ionophore (20 μM). In 2 cases of the control preparations (○), and 1 case each of animals bearing LLC-1 (▾) and BFS-1 ( ), platelets adhere onto the luminal surface of microvessels for 30 seconds. Effects were more pronounced in postcapillary venules of controls than in tumor microvessels. Median, n = 6 to 8 microvessels per experimental animal.
), platelets adhere onto the luminal surface of microvessels for 30 seconds. Effects were more pronounced in postcapillary venules of controls than in tumor microvessels. Median, n = 6 to 8 microvessels per experimental animal.
Effect of calcium ionophore A23187 on platelet adherence.
Adherence of platelets occurs irregularly after application of calcium ionophore A23187. Platelet adhesion could be observed in individual experimental animals 15 minutes after application of calcium ionophore (20 μM). In 2 cases of the control preparations (○), and 1 case each of animals bearing LLC-1 (▾) and BFS-1 ( ), platelets adhere onto the luminal surface of microvessels for 30 seconds. Effects were more pronounced in postcapillary venules of controls than in tumor microvessels. Median, n = 6 to 8 microvessels per experimental animal.
), platelets adhere onto the luminal surface of microvessels for 30 seconds. Effects were more pronounced in postcapillary venules of controls than in tumor microvessels. Median, n = 6 to 8 microvessels per experimental animal.
Discussion
During activation and aggregation, platelets release angiogenic growth factors and may thereby favor endothelial cell proliferation at sites of vessel injury and wound healing. Activation of blood coagulation in cancer disease and contribution of plasma clotting factors in tumor angiogenesis are well accepted, whereas the role of platelets in tumor angiogenesis is controversial. Dvorak29 supposed that tumor cells secrete growth factors and exert procoagulant activity by themselves, thus performing functions ascribed to platelets in wound healing. In contrast, Pinedo et al19 and Verheul et al30 proposed a functional relevance of platelets in tumor angiogenesis since tumor microcirculation may present a thrombogenic environment owing to compromised blood flow and discontinuous endothelial layers.
In our current study, we quantified platelet-endothelial interactions within the microcirculation of 2 experimental tumors by intravital fluorescence microscopy. Fluorescent labeling of syngenic platelets ex vivo was based on a method described previously,23modified by the use of the fluorescent marker CFDA for long-term labeling. The influence of the separation and labeling procedure on platelets' functionality was examined by FACS analysis following stimulation by ADP and human thrombin. ADP is considered to be a weak agonist since it depends on autocrine stimulation to promote the full sequence of platelet aggregation.31 FACS analysis demonstrated that platelets were not activated owing to the separation and labeling procedure, and fluorescently labeled platelets still possess the ability to form aggregates. In addition, aggregometry of fluorescently labeled platelets described biphasic aggregation in response to human thrombin, characterizing secretion-independent reversible aggregation followed by irreversible aggregation due to release of α-granules.32
In normal subcutaneous venules of tumor-free chamber preparations, intravital microscopy revealed low baseline rolling of fluorescently labeled platelets along the endothelial lining. This finding is consistent with data described previously by others in different organ systems.23,33 Within the tumor microvasculature, we observed slightly elevated numbers of rolling platelets in early angiogenesis, and we could only rarely detect platelet adherence. However, at low shear rates (as observed in both experimental tumors), platelets roll on immobilized fibrinogen/fibrin and collagen in an activation-independent manner that results in platelet activation, firm adhesion, and further aggregation.34 35 Therefore, the slight increase in rolling platelets with rare tight adherence, as we found in tumors, was more likely due to concomitant hemodynamic alterations in the angiogenic blood vessels than to an adhesion molecule–mediated interaction on prothrombotic surfaces.
Our results are in accordance with a study concerning hemostatic alterations in tumor-bearing mice: Poggie et al36demonstrated accumulation of radioactively labeled fibrinogen in tumor stroma of Lewis lung carcinomas; however, accumulation of radioactively labeled platelets was not detected in the same tumors. They demonstrated, secondly, that decrease in platelet counts during cancer progression could be put down to an insufficient neosynthesis, excluding platelet consumption due to activated blood coagulation. Moreover, electron microscopic studies of melanomas had only occasionally revealed small platelet aggregates and single platelets adhering to a disrupted endothelial lining at sites of tumor cell invasion into the vascular lumen.4,5,37 A positive relationship between platelets, serum VEGF concentration, and disease progression has been reported only for advanced cancer diseases characterized by dense vascularization, invasiveness, and metastatic diseases.38,39 It has recently been discussed that VEGF content in platelets not only may be a result of increased protein synthesis in megakaryocytes in response to tumor-released cytokines and growth factors but could also be a consequence of endocytosis of tumor-derived VEGF by circulating platelets.40
Up to now, the mechanism of angiogenic growth factor release from platelets is not entirely clear, but in vitro experiments have demonstrated that it is dependent on platelet activation and aggregation.15,18 A prerequisite for the promoting effect of platelets on the formation of microvascular tubuli seems to involve direct cell-to-cell interactions between platelets and the proliferating endothelium.14 The absence of intense platelet-endothelial interactions and platelet aggregation as we have shown in the in vivo model of tumor angiogenesis suggests that (1) the luminal surface of angiogenic altered host and tumor microvessels does not provide enhanced adhesive structures for platelets and (2) platelets do not become activated within the microcirculation of tumors.
The capability of tumor microvessels to accumulate platelets on their endothelial surface in response to stimulation was the object of the second approach of experiments. Rapid initiation of platelet accumulation on the endothelial surface results from the presentation of P-selectin and von Willebrand factor (VWF) released from the endothelial cell–specific Weibel-Palade bodies. Fusion of the Weibel-Palade bodies with the surface membrane can be induced by thrombin, VEGF, mediators of inflammation and reperfusion damage, and experimental ionophores, which cause an increase in intracellular calcium ions.41 Calcium ionophore A23187 has revealed in vivo P-selectin dependence of platelet rolling in mesenteric venules of mice and, more recently, VWF-mediated platelet recruitment to the intact endothelial surface.42,43 Hence, application of calcium ionophore A23187 to tumor microcirculation facilitates selective investigation of the early phase of platelet recruitment onto endothelial surfaces, which may be of relevance in processes of local tumor tissue hypoxia, tumor radiation, and tumor hypercoagulability. Our results may indicate that release from Weibel-Palade bodies and subsequent presentation of P-selectin and VWF are diminished in tumor microvessels and are not sufficient to promote platelet rolling on the endothelial surface. The observed increase in platelet rolling in postcapillary venules of normal tissue is in accordance with previously described findings in mesenteric venules.42 The lower total amount of rolling platelets in postcapillary venules of striated skin muscle in comparison with mesenteric venules can be explained by the expression of P-selectin mainly in intestinal and lung tissue.44
It has been proposed that Weibel-Palade bodies positively correlate with the angiogenic activity of human brain tumors and are found in several types of human tumors.45,46 In experimental tumor models, Weibel-Palade bodies have not been detected within the microvasculature of the amelanotic melanoma (A-Mel-3) of hamsters,4 but were described in breast cancers of mice.47 Other immunhistological studies of tumor microvessels revealed decreased or even regional absence of VWF staining, which reflects a marked quantitative heterogeneity in the degree of VWF expression among the microvascular endothelial cells in tumors.48 A similar distribution has been described for the expression of P-selectin within the microcirculation of tumors.49 These data suggest a reduction in the number of Weibel-Palade bodies or decreased discharge of VWF and P-selectin by endothelial cells of tumor microvessels.
The reduced capability of rapid platelet accumulation on the endothelial surface in tumor microcirculation may be based on a missing or an ineffective release of preformed P-selectin from endothelial cell–specific Weibel-Palade bodies. One explanation may be the sustained influence of angiogenic growth factors, especially the high levels of VEGF, accompanying tumor growth that may result in continuous secretion of Weibel-Palade bodies, preventing recycling and redistribution of P-selectin into the intracellular storage granules. Secondly, angiogenic growth factors suppress de novo synthesis of adhesion molecules, which promote platelet and leukocyte endothelial interaction at sites of tissue inflammation.50Consequently, the lack of adhesion molecules prevents interaction of circulating blood cells with the endothelium, and the proposed anergy of tumor microcirculation to immune cells may be further extended to platelets.51-53
In conclusion, the growth of 2 experimental tumors was associated with a slight, but significant, increase of platelet rolling and concomitant reduction of red blood cell velocity in the microvasculature within the immediate vicinity of tumor cells. This effect was transient and restricted to a period immediately after tumor cell implantation. Platelet interaction with the vessel wall in established tumor microvessels was indistinguishable from that observed in microvessels of non–tumor-bearing subcutaneous tissue. To find out whether the enhanced platelet contact to the endothelium in microvessels close to the site of tumor cell implantation contributes to a local angiogenic stimulus will require further investigation.
We thank M. Clauss (Max-Plank-Institute Bad-Nauheim, Germany), for providing the BFS-1 fibrosarcoma and for his helpful comments. We also thank M. Bauer (Instit für Prophylaxe und Epidemiologie der Kreislaufkrankheiten, Ludwig-Maximilians-University, Munich, Germany) for his technical assistance with the aggregometry.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Marc Dellian, Institute for Surgical Research, Ludwig-Maximilians-University, Klinikum Grosshadern, Marchioninistrasse 15, 81377 Munich, Germany; e-mail:dellian@icf.med.uni-muenchen.de.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal