Abstract
We report here 2 patients with chronic nonspherocytic hemolytic anemia (CNSHA) and severe red blood cell (RBC) adenylate kinase (AK) deficiency. One of these patients, a boy of Spanish origin, exhibited a neonatal icterus and splenomegaly and required blood transfusions until the age of 2 years. The other patient was a white, American infant born to parents who were first cousins; he also presented with neonatal icterus and anemia. In neither case was psychomotor impairment observed. The first patient was found to be a compound heterozygote for 2 different missense mutations, 118G>A(Gly40Arg) and 190G>A(Gly64Arg) (cDNA sequence first described by Matsuura et al, 1989). The second patient was homozygous for an in-frame deletion (GAC) from nucleotide (nt) 498 to 500 or nt 501 to 503 of the cDNA sequence, predicting deletion of either aspartic acid (Asp) 140 or 141. The crystal structure of porcine cytosolic AK was used as a molecular model to investigate how these mutations may affect enzyme structure and function. (Blood. 2003;102:353-356)
Introduction
Adenylate kinase (AK; adenosine triphosphate—adenosine monophosphate [ATP-AMP] phosphotransferase, EC 2.7.4.3) modulates the interconversion of adenine nucleotides: Mg2+ + ATP + AMP = Mg2+ + ADP + ADP.
AK deficiency is a rare genetic disorder that has been reported in 9 unrelated families distributed worldwide.1-9 Moderate to severe chronic nonspherocytic hemolytic anemia (CNSHA) occurred in all patients except one of black ancestry.4 Therefore, the direct relationship between the reduced erythrocyte survival and the enzyme defect has been questioned by some authors, and other concomitant causes of hemolysis have been hypothesized.4,6,7 Psychomotor impairment has been also observed in about 50% of the reported cases.2,7,9
We report here for the first time 2 cases of moderate red cell AK deficiency associated with CNSHA; 1 of them represents the first description of this enzymopathy in Spain. In one patient's parents half-normal AK activity was found, according to the autosomal recessive mode of inheritance of this enzymopathy. A molecular study of the patient's AK gene disclosed 3 different mutations: 2 point mutations located in exon 4 and leading to a 40 Gly→Arg and to a 64 Gly→Arg substitution, respectively, and a 3-bp deletion located in exon 6 leading to a codon Asp140(or 141) deletion. Apparently, these 3 mutations have not been previously described and accordingly they are considered unique. In order to study the possible effects of these mutations on enzyme molecular structure and function, a human enzyme working model derived from the porcine AK structure, with 95% sequence identity to human AK, was used.
The present study demonstrates that AK deficiency is also present in Spain and gives further support to the existence of a relationship between the enzyme molecular defect and reduced red cell survival.
Patients and methods
Patients
Patient 1. A 2-year-old Spanish boy presented with severe neonatal anemia and hyperbilirubinemia requiring blood transfusions. The hemoglobin concentration was stable at about 90 to 100 g/L with increased reticulocyte counts (190 × 109/L). Slight decreases of hemoglobin concentration were observed on occasion of intercurrent viral infections, but no further transfusions were required and psychomotor development was normal. All tests for red cell defects that were performed, including a screening for abnormal or unstable hemoglobins, red cell osmotic fragility, acidified serum, and sucrose lysis tests, were negative. The study of a battery of 20 red blood cell (RBC) enzymes revealed a partial deficiency of AK of about 25% of normal. The other enzyme activities were normal or elevated according to the 5.3% reticulocytosis. The patient's parents displayed an intermediate AK activity of about 50%.
Patient 2. This 11-week-old male infant had hyperbilirubinemia at birth and required phototherapy. The spleen tip was palpable. The direct and indirect Coombs tests were negative, the serum lactate dehydrogenase level was increased, and the total bilirubin was approximately 85.5 μM (6.84 μM direct reacting). His hemoglobin was 70 g/L and the reticulocyte count .145 × 109/L. The study of a battery of 21 RBC enzymes revealed a partial deficiency of AK of about 30% of normal. Enzyme activities that are higher than the normal range are commonly found in young RBCs in patients with hemolytic anemia. The parents of the patient were first cousins from the United States of white ethnic origin.
Hematologic assays and enzymes studies
Genetic analysis
Genomic DNA was extracted from peripheral blood leukocytes using standard techniques. The erythrocyte adenylate kinase 1 (AK-1) gene sequence (GenBank accession no. J04809) and mRNA sequence (GenBank accession no. BC001116) were used to construct oligonucleotide primers (Table 1) for polymerase chain reaction (PCR) amplification of the 7 exons of the AK-1 gene. PCR reactions contained 34 mM Tris (tris(hydroxymethyl)aminomethane)—HCl, pH 8.8; 8.3 mM NH4SO4; 1.5 mM MgCl2; 85 μg/mL bovine serum albumin; 0.2 mM each of deoxyadenosine triphosphate (dATP), deoxycytidine triphosphate (dCTP), deoxyguanosine triphosphate (dGTP), and deoxythymidine triphosphate (dTTP); 1 U AmpliTaq DNA polymerase; 250 ng of each oligonucleotide primer; either 0% or 5% dimethyl sulfoxide (DMSO); and 200 ng genomic DNA in a 50-μL system. After denaturation at 98°C for 4 minutes the PCR was carried out for 31 cycles of 94°C for 30 seconds, and then at the annealing temperatures as shown in Table 1 for 30 seconds and 72°C for 30 seconds. The PCR fragments were purified using a QIAamp PCR Purification Kit (Qiagen, Valencia, CA) and were sequenced using one of the amplification primers on an Applied Biosystems (Foster City, CA) automatic DNA sequencer.
Oligonucleotide primers for AK PCR amplification and sequencing
Exon . | Name . | Amplification primer, 5′ to 3′ . | DMSO, % . | Annealing temperature, °C . | Fragment size, bp . |
|---|---|---|---|---|---|
| 1 | AK 1FN | GGTGTCGCCGCGCACCCG | 5 | 66 | 394 |
| AK 1RO | CGAGGCACAGATCCCCAGCG | ||||
| 2 | AK 2F | GCACACACCAGTTGCCTTGG | 5 | 66 | 271 |
| AK 2R | TGGAGGCTCCCAGCCAGG | ||||
| 3 to 4 | AK 3F | GCCTGGGACTCCAGAGGTG | 5 | 63 | 543 |
| AK 4R | AGCTTTGCCTGTGTGCCGTG | ||||
| 5 | AK 5FN | GCAGCGTGACGAGAGGCTG | 0 | 66 | 293 |
| AK 5R | GAACTCTGACCTGCATCACAG | ||||
| 6 | AK 6F | GAAGGGATTGAAGGTCTGAGG | 5 | 63 | 398 |
| AK 6R | AGAGGGGCTGGCCTGAGG | ||||
| 7 | AK 7F | AGGCAGGCCTGGTCTCTGG | 5 | 67 | 263 |
| AK 7R | GTCTGTGCTCAGCAGGGCAG |
Exon . | Name . | Amplification primer, 5′ to 3′ . | DMSO, % . | Annealing temperature, °C . | Fragment size, bp . |
|---|---|---|---|---|---|
| 1 | AK 1FN | GGTGTCGCCGCGCACCCG | 5 | 66 | 394 |
| AK 1RO | CGAGGCACAGATCCCCAGCG | ||||
| 2 | AK 2F | GCACACACCAGTTGCCTTGG | 5 | 66 | 271 |
| AK 2R | TGGAGGCTCCCAGCCAGG | ||||
| 3 to 4 | AK 3F | GCCTGGGACTCCAGAGGTG | 5 | 63 | 543 |
| AK 4R | AGCTTTGCCTGTGTGCCGTG | ||||
| 5 | AK 5FN | GCAGCGTGACGAGAGGCTG | 0 | 66 | 293 |
| AK 5R | GAACTCTGACCTGCATCACAG | ||||
| 6 | AK 6F | GAAGGGATTGAAGGTCTGAGG | 5 | 63 | 398 |
| AK 6R | AGAGGGGCTGGCCTGAGG | ||||
| 7 | AK 7F | AGGCAGGCCTGGTCTCTGG | 5 | 67 | 263 |
| AK 7R | GTCTGTGCTCAGCAGGGCAG |
Working model for human AK
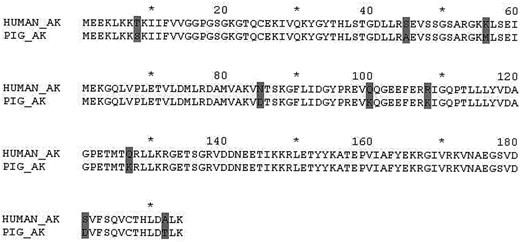
In order to investigate how these mutations could lead to dysfunction of the molecule, we used the crystal structure of porcine cytosolic AK13 with sequence identity to the human AK of 95% (Figure 1). The structure of the complex of AK and AMP was deduced from the structure of AK from beef heart mitochondrial matrix in complex with AMP.14 The beef heart AK is 46—amino acid residues longer than the human AK; however the 2 molecules have the same overall tertiary structure and the AMP binding domains are highly homologous.
A comparison porcine and human AK. Numbers and asterisks indicate the consecutive sequence of amino acid residues: * (10, 30, 50, etc) and number (20, 40, 60, etc). Gray shaded areas indicate the amino acid differences between porcine and human AK.
A comparison porcine and human AK. Numbers and asterisks indicate the consecutive sequence of amino acid residues: * (10, 30, 50, etc) and number (20, 40, 60, etc). Gray shaded areas indicate the amino acid differences between porcine and human AK.
Results
Red cell enzyme assays
The results of enzyme assays performed in the patients are summarized in Table 2. AK activity was about 25% to 30% of normal in both patients and intermediate in the parents of case 1. The other enzymatic activities were normal or slightly increased in relation to reticulocytosis.
Red cell enzymes in the patients with AK deficiency
. | Patient 1 . | Reference values, range* . | Patient 2 . | Reference values, range† . |
|---|---|---|---|---|
| Hexokinase | 1.88 | 0.62-1.26 | 2.23 | 0.67-1.79 |
| Glucosephosphate isomerase | 69 | 45.0-66.0 | 45.2 | 25.4-51.6 |
| Phosphofructokinase | 9.4 | 6.20-13.9 | 3.80 | 3.02-6.38 |
| Triosephosphate isomerase | 1446 | 1361-2769 | 1560 | 805-1971 |
| Glyceraldehyde-P-dehydrogenase | 291 | 168-300 | 152 | 119-258 |
| Phosphoglycerate kinase | 394 | 197-343 | 239.9 | 175-260 |
| Pyruvate kinase | 19.6 | 8.40-15.2 | 11.97 | 7.32-16.0 |
| Glucose-6-phosphate dehydrogenase | 11.7 | 5.70-9.90 | 14.1 | 9.30-14.2 |
| 6-phosphogluconic dehydrogenase | 11.6 | 6.12-10.2 | 9.65 | 6.75-10.7 |
| Adenylate kinase | 64 | 180-310 | 44.9 | 87.7-241 |
| Enolase | 10 | 3.58-8.22 | 6.80 | 2.91-6.0 |
| Monophosphoglyceratemutase | 13.6 | 10.7-20.63 | 22.63 | 13.4-24.10 |
| Diphosphoglyceratemutase | 8.0 | 2.86-7.70 | 6.54 | 1.21-5.27 |
| Lacticdehydrogenase | 202 | 135-233 | 128 | 60.4-214 |
| Glutathione reductase | 12.3 | 5.30-11.90 | 5.10 | 0.62-8.83 |
| Glutathione peroxidase | 10.2 | 9.10-25.0 | 33.7 | 21.4-40.3 |
| Adenosine deaminase | 2.0 | 0.54-1.40 | 1.06 | 0.70-1.60 |
| Pyrimidine 5′ nucleotidase, mU/gHb | 230 | 150-210 | 299.7 | 100.5-176.1 |
| Aldolase | 2.8 | 1.46-3.46 | 2.65 | 1.01-3.29 |
. | Patient 1 . | Reference values, range* . | Patient 2 . | Reference values, range† . |
|---|---|---|---|---|
| Hexokinase | 1.88 | 0.62-1.26 | 2.23 | 0.67-1.79 |
| Glucosephosphate isomerase | 69 | 45.0-66.0 | 45.2 | 25.4-51.6 |
| Phosphofructokinase | 9.4 | 6.20-13.9 | 3.80 | 3.02-6.38 |
| Triosephosphate isomerase | 1446 | 1361-2769 | 1560 | 805-1971 |
| Glyceraldehyde-P-dehydrogenase | 291 | 168-300 | 152 | 119-258 |
| Phosphoglycerate kinase | 394 | 197-343 | 239.9 | 175-260 |
| Pyruvate kinase | 19.6 | 8.40-15.2 | 11.97 | 7.32-16.0 |
| Glucose-6-phosphate dehydrogenase | 11.7 | 5.70-9.90 | 14.1 | 9.30-14.2 |
| 6-phosphogluconic dehydrogenase | 11.6 | 6.12-10.2 | 9.65 | 6.75-10.7 |
| Adenylate kinase | 64 | 180-310 | 44.9 | 87.7-241 |
| Enolase | 10 | 3.58-8.22 | 6.80 | 2.91-6.0 |
| Monophosphoglyceratemutase | 13.6 | 10.7-20.63 | 22.63 | 13.4-24.10 |
| Diphosphoglyceratemutase | 8.0 | 2.86-7.70 | 6.54 | 1.21-5.27 |
| Lacticdehydrogenase | 202 | 135-233 | 128 | 60.4-214 |
| Glutathione reductase | 12.3 | 5.30-11.90 | 5.10 | 0.62-8.83 |
| Glutathione peroxidase | 10.2 | 9.10-25.0 | 33.7 | 21.4-40.3 |
| Adenosine deaminase | 2.0 | 0.54-1.40 | 1.06 | 0.70-1.60 |
| Pyrimidine 5′ nucleotidase, mU/gHb | 230 | 150-210 | 299.7 | 100.5-176.1 |
| Aldolase | 2.8 | 1.46-3.46 | 2.65 | 1.01-3.29 |
Enzyme activities are expressed in IU/gHb, except where indicated otherwise.
From the laboratory of J.-L.V.C. (Barcelona, Spain).
From the laboratory of E.B. (La Jolla, CA).
Genetic analysis
The sequence of complete erythrocyte AK-1 cDNA showed the presence of 2 different missense mutations in patient 1 in exon 4: one cDNA nucleotide 118G>A leading to a glycine (Gly) to arginine (Arg) change in amino acid (AA) 40, and the other cDNA nucleotide 190G>A changing AA 64 from Gly to Arg. When exon 4 of the DNA from the patient's parents was sequenced, the father was found to be a heterozygote G/A at nucleotide (nt) 118 and the mother G/A at nt 190. Patient 2 was homozygous for an in-frame deletion of nucleotides GAC in exon 6 causing a deletion of an aspartic acid (Asp) residue. This region consists of 2 consecutive GACs, so that the deletion is of either nt 498 to 500 or nt 501 to 503 causing a deletion of Asp 140 or 141.
Working model for human AK deficiency
The comparison of the AK structures from beef heart mitochondrial matrix bound to AMP and apoporcine cytosol reveals that significant rearrangements take place in the AMP binding domain upon AMP binding. This observation suggests that large movements are likely to occur during catalysis. We used the position of AMP from the beef structure and placed it in the porcine structure to create a working model for the substrate-bound human enzyme (Figure 2). The residue Gly40 is located at the AMP binding site and the residue Gly64 is in the vicinity of the AMP binding site. Replacement of the smallest amino acid Gly by Arg with a large side chain is likely to hinder AMP binding. Residue Asp140(141) is part of the connecting link between 2 helices, and its deletion may result in changes in shape and/or flexibility of enzyme structure.
A stereoscopic view of a model for the human AK bound to the substrate AMP. The locations of the 3 mutations, 40, 64, and 140 (141), are indicated in red. The flexible loop containing residue 64 is shown in orange and AMP in blue. The N and C termini are labeled as N and C. The figure was produced using the program BOBSCRIPT.15
A stereoscopic view of a model for the human AK bound to the substrate AMP. The locations of the 3 mutations, 40, 64, and 140 (141), are indicated in red. The flexible loop containing residue 64 is shown in orange and AMP in blue. The N and C termini are labeled as N and C. The figure was produced using the program BOBSCRIPT.15
Discussion
AK is present in red cells and muscle and exists as 3 different isozymes designated AK1, AK2-1, and AK2.16 Chronic hemolytic anemia associated with AK deficiency is a rare condition; only 9 unrelated families have been reported so far.1-9 AK deficiency is transmitted by autosomal recessive mode of inheritance and the heterozygous state is not accompanied by disease. Homozygotes or compound heterozygotes exhibit moderate to severe CNSHA with hemoglobin levels of 80 to 90 g/L. In some cases, splenectomy results in a complete remission of the hemolytic process.7 The first case of AK deficiency was described by Szeinberg et al1 in 2 offspring of second-cousin Arab parents with severe hemolytic anemia. In 1971, Boivin et al2 described mental retardation in a patient with severe red cell AK deficiency and hemolytic anemia. Although in this case the neurologic impairment was attributed to the forceps delivery and resuscitation at birth, mental retardation from mild to severe has been later reported in other patients with severe red cell AK deficiency.7-9 Since the AK1 isoenzyme is expressed in red cells and brain, it can be suggested that the mutation, especially in such cases of severe enzyme deficiency, may be accompanied by brain abnormalities. Conversely, patients with residual red cell AK activity that was only partially reduced (from 20% to 50% of normal) exhibit a mild to moderate hemolytic anemia but normal physical and mental development.5,6,8 The finding by Beutler et al4 of a child with total absence of RBC AK activity and no evidence of hemolysis or mental retardation raised a question regarding the cause-effect relationship between AK deficiency and hemolytic anemia. Some investigators suggested that the shortened survival of AK-deficient RBCs was caused, or at least enhanced, by the coexistence of defects of other enzymes such as phosphoribosyl pyrophosphate synthetase, pyruvate kinase, and AMP—guanosine triphosphate (GTP) phosphotransferase6 ; glucose-6-phosphate dehydrogenase (G6PD)1,7 ; or other unidentified factors.17 The most recently reported case by Bianchi et al9 of a nonsense mutation in 2 siblings with severe red cell AK deficiency and mental retardation fully explains the biochemical phenotype and definitely shows that AK gene inactivation causes a complete lack of AK. In fact, this is the most drastic molecular abnormality of the AK-1 gene so far reported, and its relationship with the lack of enzyme activity is unequivocal.
The AK1 gene is located in 9q34.1—q34.3; it is 12-kb long and has 7 exons. Until now only 3 of the AK deficiency reported cases have been characterized in molecular terms. The first case, originally reported by Miwa et al5 and Matsuura et al,17 determined the nucleotide sequences of 2 alleles of the AK1 gene cloned from DNA, and a transition mutation (CGG>TGG) was found in exon 6 on one allele, resulting in an Arg to tryptophan (Trp) substitution at the 128—amino acid residue of AK1. The second analysis of AK gene exons,8 based on polymerase chain reaction—single-strand conformational polymorphism, showed an abnormality in the fragment containing exon 6. The subsequent sequence analysis of this abnormal fragment revealed homozygous and heterozygous A>G substitutions at codon 164 in the proband and in the parents and a brother, respectively, corresponding to a tyrosine to cysteine substitution in the AK protein. Finally, in the case of Bianchi et al,9 the sequence of complete erythrocyte AK-1 cDNA showed the presence in 2 siblings of a nonsense homozygous mutation at codon 107 (CGA>TGA, Arg→Stop). This mutation, which results in a truncated protein of 107 amino acids, fully explains the biochemical phenotype of AK deficiency and definitely shows that AK gene inactivation causes a complete lack of AK activity.
In the present study, 3 new mutations of AK have been found in 2 unrelated patients. They are Gly40Arg, Gly64Arg, and deletion of residue 140 (or 141). To investigate how these mutations could lead to dysfunction of the enzyme molecule, we examined the crystal structure of porcine cytosolic AK13 and created a working model for the substrate-bound human enzyme by placing on it the position of AMP from the beef heart mitochondrial matrix AK structure (Figure 2).14 Both residues Gly40 and Gly64 are located in the AMP binding domain of AK. The substitution of Gly40 by Arg would interfere with the AMP binding. The residue Gly64 is located in a loop that connects 2 helices, and this loop undergoes large movements upon AMP binding, changing the cleft from an “open” state to a “closed” state.18 The Gly64Arg mutation would reduce the flexibility of this loop and possibly cause steric hindrance to AMP binding. The consequences of the deletion of residue Asp140(141) are harder to visualize. However, since this residue is part of the connecting link between 2 helices, one could speculate that the resulting changes in shape and/or flexibility may have some indirect effect on the function of the enzyme molecule.
Prepublished online as Blood First Edition Paper, March 20, 2003; DOI 10.1182/blood-2002-07-2288.
Supported in part by National Institutes of Health grants HL25552, HL0555375, RR00833, and HL55375; the Stein Endowment Fund; and the Spanish Ministry of Health FISS grants 00/0584 and SAF 01-1205.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
This is manuscript number 15030-MEM from The Scripps Research Institute.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal