Abstract
The breaking of immune tolerance of “self-antigens” associated with angiogenesis is an attractive approach to cancer therapy by active immunity. We used vascular endothelial growth factor receptor-2 (VEGFR-2) as a model antigen to explore the feasibility of the immunotherapy with a vaccine based on a xenogeneic homologous protein. To test this concept, we prepared a quail homologous VEGFR-2 protein vaccine (qVEGFR) based on quail VEGFR-2. At the same time, a protein vaccine based on the corresponding ligand-binding domain of mouse self-VEGFR-2 (mVEGFR) was also prepared and used as a control. We found that immunotherapy with qVEGFR was effective at protective and therapeutic antitumor immunity in several solid and hematopoietic tumor models in mice. Autoantibodies against mouse VEGFR-2 (Flk-1) were identified by Western blot analysis and enzyme-linked immunosorbent assay (ELISA). Anti-VEGFR antibody-producing B cells were detectable by ELISPOT. Endothelial deposition of immunoglobulins developed within tumor. VEGF-mediated endothelial cell proliferation was inhibited in vitro by immunoglobulins from qVEGFR-immunized mice. Antitumor activity was caused by the adoptive transfer of the purified immunoglobulins. Antitumor activity and production of autoantibodies against Flk-1 could be abrogated by the depletion of CD4+ T lymphocytes. Angiogenesis was apparently inhibited within the tumors, and the vascularization of alginate beads was also reduced. No marked toxicity was found in the immunized mice. The observations may provide a vaccine strategy for cancer therapy through the induction of autoimmunity against the growth factor receptor associated with angiogenesis in a cross-reaction with single xenogeneic homologous protein.
Introduction
The formation of new capillaries from pre-existing vessels, angiogenesis, is a complex multistep process that includes endothelial proliferation, migration and differentiation, degradation of extracellular matrix, and so on.1,2 Angiogenesis is important not only for some physiological processes but also for the development of pathologic conditions such as cancer, rheumatoid arthritis, and retinopathies.3-6 There is accumulating evidence that the growth and persistence of solid tumors and their metastasis are angiogenesis dependent.7,8 Antiangiogenic therapy, which targets activated endothelial cells, might represent a good alternative for the treatment of tumors.1,3,7,9
Vascular endothelial growth factor receptor-2 (VEGFR-2, also called Flk-1 in mice, KDR in humans, and Quek-1 in quail) is the main receptor responsible for the angiogenic activity of VEGF.10,11 The extracellular region of KDR consists of 7 immunoglobulin-like domains. The third one is critical for ligand binding, and the second and fourth domains are important for ligand association.12 Targeted inactivation of the gene for Flk-1 in mice results in the impairment of vasculogenesis and the death of the embryo at day 8.5.6 Overexpression of KDR is found on activated endothelial cells of newly formed vessels and is strongly associated with invasion and metastasis in human malignant diseases.8,13,14 Moreover, it has been reported that the inhibition of tumor growth and metastasis in a variety of animal models has been achieved by various approaches that disrupt or neutralize the functions of either VEGF or VEGFR-2,15-17 suggesting that VEGF and VEGFR-2 play an important role in tumor angiogenesis, a process essential for tumor growth and metastasis. It has been suggested that angiogenesis mediated by the VEGF/VEGFR-2 signaling pathway also plays an important role in the development and progression of hematopoietic malignancies.18,19
It is conceivable that the breaking of immune tolerance against this VEGFR-2 (Flk-1) on autologous angiogenic endothelial cells is a useful approach for cancer therapy with active immunity. However, immunity to angiogenic vessels is presumably difficult to elicit by a vaccine based on autologous or syngeneic molecules because of the immune tolerance acquired during the early development of the immune system.
Many genes were highly conserved during the evolutionary process, which is characterized by the varying degrees of gene similarity among different species.20 Many counterparts of the genes of human and mouse can even be identified from the genome sequence of the fruit fly, Drosophila melanogaster, and of animals such as quail. For example, Quek-1 in quail is known to be homologous, to a varying extent, with KDR in human and Flk-1 in mouse. Sequence comparison analysis by searching the SwissProt database in the present study indicates that the primary sequence of quail VEGFR-2 (Quek-1) at the amino acid level is 67% and 70% identical with mouse homologue (Flk-1) and human (KDR), respectively. The current study explores the feasibility of immunotherapy of tumors with a vaccine based on quail homologous VEGFR-2 as a model antigen, used in breaking the immune tolerance against VEGFR-2 in a cross-reaction between the xenogeneic homologues and self-molecules.
To test this concept, we prepared a quail homologous VEGFR-2 protein vaccine (qVEGFR) based on quail VEGFR-2. At the same time, the protein vaccine based on the corresponding ligand-binding domain of mouse self–Flk-1 (mVEGFR) was also prepared and used as a control. Vaccines were tested for the ability to induce antitumor immunity in tumor models in mice.
Materials and methods
Vaccine preparation
Total RNA was isolated from mouse or quail embryos using TRIzol reagent (Invitrogen, Grand Island, NY) and was subjected to reverse transcription–polymerase chain reaction (RT-PCR) for the amplification of the encoding sequence comprising the N-terminal 134 to 417 amino acid residues of extracellular domains of Flk-1 and the corresponding fragment of Quek-1. The amplified fragment covered the coding sequence of the ligand-binding domain of VEGFR-2. Upstream primer and downstream primer for the amplified fragment of Flk-1 were 5′-TAGGTACCCAGCATGGCATCGTGTACATC-3′ (a KpnI site was introduced at the 5′ end) and 5′-GACTGCAGTTACAGAGAGACCATGTGGCTC-3′ (a PstI site and a termination codon were introduced at the 5′ end), respectively. The primers for that of Quek-1 were 5′-TAGGTACCCAGCTTGGCATTGTGTACATC-3′ (a KpnI site was introduced at 5′ end) and 5′-GAGTCGACTTACAGGGTGAATGTATGTCTCTTC-3′ (a SalI site and a termination codon were introduced at 5′ end), respectively. Amplified products were then subcloned into the pQE30 expression vector (Qiagen, Chatsworth, CA). Ligated DNA was used to transform Escherichia coli JM109 strains. The correct coding sequence was verified by nucleotide sequencing of the insert in the plasmid. Transformants were cultured for recombinant protein expression by adding isopropyl-β-d-thiogalactoside (IPTG) to a final concentration of 1 mM. Recombinant proteins were purified from the bacterial lysates by affinity chromatography on a nickel-nitrilotriacetic acid (Ni-NTA) gel matrix (Qiagen) under denaturing conditions (8 M urea, 100 mM NaH2PO4, 10 mM Tris, 10 mM mercaptoethanol, pH 8), and elution was achieved with the same buffer (pH 4.5). Thereafter, the purified proteins were extensively dialyzed to allow refolding. Refolded proteins were further purified by ion exchange and gel filtration chromatography, then lyophilized and stored in 4°C. Purified proteins were confirmed by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) and Western blot analysis and were also tested for endotoxin. Recombinant protein vaccines based on the fragment of Quek-1 and Flk-1 were named qVEGFR and mVEGFR, respectively. They were dissolved in phosphate-buffered saline (PBS) before use for vaccination and were mixed with an equal volume of aluminum hydroxide (ALUM) adjuvant at 4 mg/mL for 30 to 60 minutes as described.21
Immunotherapy and tumor models
Mice at 6 to 8 weeks of age were injected subcutaneously once weekly for 4 continuous weeks with different doses (1-50 μg per mouse) of protein vaccine. Additional control animals were injected with vaccine vehicle (ALUM) alone or PBS alone (nonimmunized). Mice were then challenged with 1 × 106 live tumor cells after the fourth immunization. For the investigation of the therapeutic effect against the established tumors, 10 mice in each group were treated with subcutaneous injection of the vaccines or ALUM once weekly for 4 weeks starting on day 7 after the subcutaneous introduction of 5 × 105 to 1 × 106 live tumor cells. LL/2 Lewis lung carcinoma (LL/2), CT26 colon carcinoma (CT26), and Meth A fibrosarcoma (Meth A) were selected for the present study because these tumors are dependent on the VEGFR-2 pathway, as reported previously.22-27 We also found that the administration of an adenoviral vector encoding soluble forms of Flk-1 significantly inhibited the growth rate of these 3 tumors (more than 76%). In addition, MOPC-315 plasmacytoma (MOPC-315) and EL4 lymphoma (EL4) was also used to investigate the antitumor activity of the vaccines. CT26 colon carcinoma, Meth A fibrosarcoma, and MOPC-315 plasmacytoma models were established in BALB/c mice, and LL/2 Lewis lung carcinoma and EL4 lymphoma models were established in C57BL/6 mice. Tumor volume was determined by the following formula: tumor volume (mm3) = π/6 × length (mm) × width (mm) × width (mm). All studies involving mice were approved by the West China Hospital Cancer Center's Animal Care and Use Committee.
To test the efficacy of protein vaccines to the tumor metastasis model, 5 × 105/100 μL CT26 cells were injected into the tail vein of each BALB/c mouse on day 7 after the fourth immunization (as described). Eighteen days later, when control mice became moribund, the mice were killed to count lung metastasis nodules and to measure the weight of lungs.28
ELISA
Ninety-six–well plates were coated with purified recombinant proteins (100 μL/well, 3 μg/mL) in coating buffer (carbonate-bicarbonate, pH 9.6) overnight at 4°C. Plates were washed with PBST (0.05% Tween 20 in PBS) and were blocked for 1 hour at 37°C with 200 μL/well 1% bovine serum albumin (BSA) in PBST. Mouse sera diluted serially in PBS were added for 2 hours at 37°C, followed by a dilution of antimouse immunoglobulin G (IgG) subclass or anti-IgM or anti-IgA antibody conjugated to alkaline phosphatase. Enzyme activity was measured with an enzyme-linked immunosorbent assay (ELISA) reader (Bio-Rad Laboratories, Hercules, CA).
Enzyme-linked immunospot assay
The enzyme-linked immunospot (ELISPOT) assay for the enumeration of anti-VEGFR antibody-producing cells has been described.29 Briefly, polyvinylidene difluoride (PVDF)–bottomed 96-well Filtration Plates (Millipore, Bedford, MA) were coated with 30 μg/mL recombinant mVEGFR or qVEGFR protein. Mononuclear cells prepared from spleen were incubated on the plates at 37°C for 4 hours. IgG bound to the membrane was revealed as spots with alkaline phosphatase–conjugated antimouse IgG antibodies.
Western blot analysis
Western blot analysis was performed as described.26,30 Briefly, recombinant proteins or lysates of cells were separated by SDS-PAGE. Gels were electroblotted with Sartoblot onto a PVDF membrane. Membrane blots were blocked at 4°C in 5% nonfat dry milk, washed, and probed with mouse sera at 1:500. Blots were then washed and incubated with a biotinylated secondary antibody (biotinylated horse antimouse IgG or IgM), followed by transfer to Vectastain ABC (Vector Laboratories).
Purification of immunoglobulin, its inhibition of cell proliferation in vitro, and its adoptive transfer in vivo
Immunoglobulins were purified from the pooled sera derived from the mice at day 7 after the fourth immunization or from control mice by affinity chromatography (CM Affi-gel Blue Gel Kit; Bio-Rad). The inhibition of VEGF-mediated endothelial cell proliferation was described.31 Briefly, exponentially growing human umbilical vein endothelial cells (HUVECs, 1 × 103 cells/well in 96-well plates) were exposed to human VEGF (200 ng/mL; Sigma-Aldrich) (untreated) or with various concentrations of the immunoglobulins (1-150 μg/mL) (treated) for 72 hours of culture. The number of viable cells was determined by a trypan blue dye exclusion test, and the percentage inhibition was calculated by the following formula: inhibition % = [(N – NT)/(N – N0)] × 100, where N is the number of untreated cells cultured for 3 days, N0 is the cell number on day 0, and NT is the number of treated cells cultured for 3 days.
To assess the efficacy of immunoglobulins in antitumor in vivo, purified immunoglobulins (10-300 mg/kg) were adoptively and intravenously transferred 1 day before mice were challenged with 1 × 105 to 1 × 107 tumor cells and then were treated twice per week for 3 weeks.
In vivo depletion of immune cell subsets
Immune cell subsets were depleted as described.26,32 Mice were injected intraperitoneally with 500 μg of either the anti-CD4 (clone GK 1.5, rat IgG), anti-CD8 (clone 2.43, rat IgG), anti-natural killer (NK) (clone PK136) monoclonal antibody (mAb), or isotype controls 1 day before immunization and then twice per week for 3 weeks. Tumor cells (1 × 106 to 1 × 107) were challenged after the fourth immunization. These hybridomas were obtained from the American Type Culture Collection (Manassas, VA). The depletion of CD4+, CD8+, and NK cells was consistently greater than 98%, as determined by flow cytometry (Coulter Elite ESP).
In vitro cytotoxicity assay
For the determination of the possible Flk-1–specific cytotoxicity mediated by CTL, a 4-hour chromium Cr 51 release assay was performed as described by others and us previously.30,33 Briefly, CT26/Flk-1 and LL/2/Flk-1 expressing Flk-1 were created by retroviral transduction with Flk-1 and were used as target cells.33 Splenocytes obtained from the immunized or control mice were treated with ammonium chloride–potassium lysing buffer to deplete erythrocytes. To prepare T-enriched cell fraction, these splenocytes were further incubated in complete medium for 90 minutes. Nonadherent cells were removed gently and incubated on nylon wool columns. One hundred microliters effector cells and 51Cr-labeled target cells were assigned at different E:T (effector-target) ratios to each well of microtiter plates and were incubated for 4 hours at 37°C. Samples were then harvested, and the activity was calculated by the formula: % cytotoxicity = [(experimental release – spontaneous release)/(maximum release – spontaneous release)] × 100. As a positive control, we also tested Flk-1–specific cytotoxicity against Flk-1–transfected cells as target cells with the T-enriched cell fraction isolated from mice immunized with dendritic cells transfected with adenovirus encoding Flk-1.
Immunohistochemistry
Frozen sections were fixed in acetone, incubated, and stained with an antibody reactive to CD31, as described.34 Sections were then stained with labeled streptavidin biotin reagents (DAKO LSAB kit, peroxidase; DAKO, Carpinteria, CA). Vessel density was determined by counting the number of microvessels per high-power field in the sections, as described.34 For the identification of autoantibodies through immunohistochemistry, frozen sections were fixed in acetone, washed with PBS, and incubated with goat fluorescein isothiocyanate (FITC)–conjugated antibody against mouse IgA, IgM, or IgG (Sigma). Slides were examined by fluorescence microscopy.
Alginate encapsulation assay
Alginate-encapsulated tumor cell assays were performed as described previously.15,35 Briefly, Meth A or CT26 cells were resuspended in a 1.5% solution of sodium alginate and added dropwise into a swirling 37°C solution of 250 mM calcium chloride. Alginate beads were formed containing approximately 1 × 105 tumor cells per bead. Mice immunized with vaccines or ALUM alone were then anesthetized, and 4 beads were implanted subcutaneously into an incision made on the dorsal side. Incisions were closed with surgical clamps. After 12 days, mice were injected intravenously with 100 μL of a 100 mg/kg FITC-dextran solution (Sigma). Beads were surgically removed, and FITC-dextran was quantified against a standard curve of FITC-dextran.
Evaluation of possible adverse effects
Mice immunized with these vaccines have been investigated, in particular for potential toxicity, for more than 10 months. Gross measures such as weight loss, ruffling of fur, life span, behavior, and feeding were investigated. Tissues of heart, liver, spleen, lung, kidney, brain, bone marrow, and so on were also fixed in 10% neutral buffered formalin solution and embedded in paraffin. Sections of 3 to 5 μm were stained with hematoxylin and eosin (H&E).
Immunostaining for active caspase-3 in lung was performed as described previously.36 Briefly, acetone-fixed, frozen sections from lung tissues were incubated with a monoclonal rabbit antimouse active caspase-3 at a 1:250-1000 dilution (BD PharMingen, San Diego, CA) at 4°C overnight. Following washes, the secondary antibody, biotinylated goat antirabbit antibody at a 1:100 dilution, (DAKO) was added. Sections were then stained with streptavidin biotin reagents (DAKO LSAB kit; peroxidase). Terminal dUTP nick-end labeling (TUNEL) staining was performed using an in situ cell death detection kit (Roche Molecular Biochemicals) following the manufacturer's protocol, as reported previously by others and us.36,37 It is based on the enzymatic addition of digoxigenin-nucleotide to the nicked DNA by terminal deoxynucleotidyl transferase. Sections in H&E staining and immunohistochemical staining were observed by 2 pathologists masked to the study.
Fertility was evaluated as reported previously.33 Briefly, 2 weeks after the fourth immunization with qVEGFR, mVEGFR, ALUM alone, or nonimmunization, female mice were allowed to cohabitate with males. Days until parturition and number of pups were recorded.
Evaluation of effects on hematopoiesis was described previously.16 Animals were subjected to complete peripheral blood counts and differentials. In addition, bone marrow cells were also enumerated. Vaccinated and control mice were evaluated for neuromuscular performance by the wire hang test and the footprint test, as reported previously.33,38,39
Results
Induction of protective and therapeutic antitumor immunity
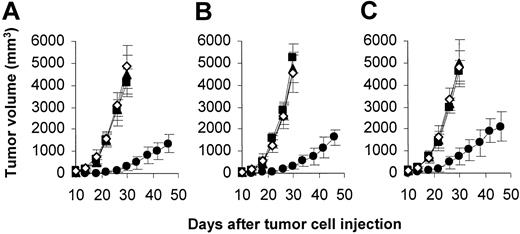
Mice were immunized with protein vaccines (qVEGFR or mVEGFR), vaccine vehicle (ALUM), or PBS alone (nonimmunized mice) once a week for 4 weeks and then were challenged with tumor cells. Tumors grew progressively in all nonimmunized mice and in mice immunized with mVEGFR or ALUM, but there was an apparent protection from tumor growth in mice immunized with qVEGFR (Figure 1).
Induction of protective antitumor immunity. Mice (10 mice/group) were immunized with 10 μ g qVEGFR (•), mVEGFR (▪), vehicle (ALUM; ▴) alone, or PBS alone (nonimmunized; ⋄) once a week for 4 weeks. Mice were then challenged subcutaneously with 1 × 106 CT26 (A), LL/2 (B), or Meth A cells (C) 1 week after the fourth immunization. There was an apparent difference in tumor volume between qVEGFR-immunized and control groups. Results are expressed as mean ± SEM.
Induction of protective antitumor immunity. Mice (10 mice/group) were immunized with 10 μ g qVEGFR (•), mVEGFR (▪), vehicle (ALUM; ▴) alone, or PBS alone (nonimmunized; ⋄) once a week for 4 weeks. Mice were then challenged subcutaneously with 1 × 106 CT26 (A), LL/2 (B), or Meth A cells (C) 1 week after the fourth immunization. There was an apparent difference in tumor volume between qVEGFR-immunized and control groups. Results are expressed as mean ± SEM.
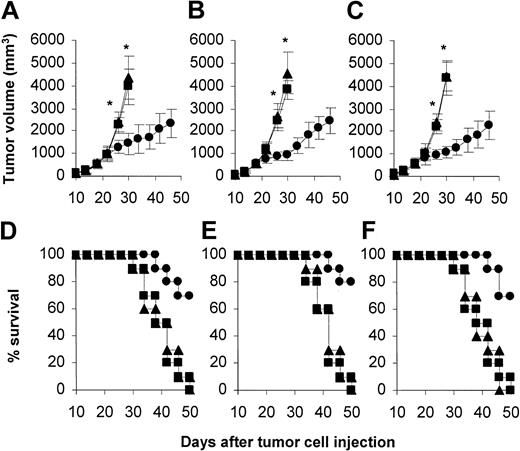
To explore the therapeutic efficacy of qVEGFR vaccine, we treated the mice on day 7 after the implantation of tumor cells, when the tumors were palpable. Treatment with qVEGFR once weekly resulted in significant antitumor activity in Lewis lung carcinoma (LL/2), CT26 colon carcinoma (CT26), and Meth A fibrosarcoma (Meth A) models. Survival of the tumor-bearing mice treated with qVEGFR was also significantly greater than that of the controls (Figure 2).
Induction of the therapeutic antitumor immunity. Mice (10 mice/group) were treated by subcutaneous injection of 10 μg qVEGFR (•), mVEGFR (▪), or ALUM (▴) once a week for 4 weeks starting at day 7 after 1 × 106 CT26 (A,D) or LL/2 (B,E) or Meth A cells (C,F) were introduced subcutaneously into mice. Results are expressed as mean ± SEM. Asterisks (*) indicate a significant difference in tumor volume (P < .05) between qVEGFR-treated and control groups. A significant increase in survival in qVEGFR-treated mice, compared with the control groups (P < .01, by log-rank test), was found in 3 tumor models.
Induction of the therapeutic antitumor immunity. Mice (10 mice/group) were treated by subcutaneous injection of 10 μg qVEGFR (•), mVEGFR (▪), or ALUM (▴) once a week for 4 weeks starting at day 7 after 1 × 106 CT26 (A,D) or LL/2 (B,E) or Meth A cells (C,F) were introduced subcutaneously into mice. Results are expressed as mean ± SEM. Asterisks (*) indicate a significant difference in tumor volume (P < .05) between qVEGFR-treated and control groups. A significant increase in survival in qVEGFR-treated mice, compared with the control groups (P < .01, by log-rank test), was found in 3 tumor models.
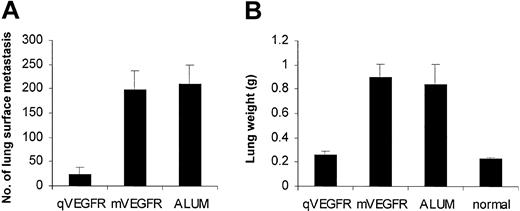
Treatment with qVEGFR vaccine in a prophylactic protocol also suppressed the formation and growth of lung metastasis in mouse CT26 colon adenocarcinoma. The number of surface metastases was significantly smaller in qVEGFR-immunized mice than in controls (24.4 ± 14.64 vs 210.4 ± 39.49 [vehicle] or 199.0 ± 38.07 [mVEGFR]; P < .01) (Figure 3A). In addition, the average lung weight of mice immunized by qVEGFR was similar to that of age- and sex-matched nontumor-bearing animals (0.262 ± 0.033 and 0.232 ± 0.013, respectively) (Figure 3B), whereas the mean lung weight in animals immunized with ALUM or mVEGFR was more than 3 times higher (0.84 ± 0.17 g and 0.90 ± 0.10 g, respectively; P < .01).
Inhibition of the formation and growth of lung metastases in mouse CT26 colon adenocarcinoma. Mice were immunized as described, and 5 × 105 CT26 cells were then injected into tail vein 1 week after the fourth immunization. The experiment was terminated after 18 days when control mice became moribund, and lungs were weighed and assessed for the presence of surface metastasis. qVEGFR vaccine can decrease the number of surface metastases (A) and abolish tumor burden by rendering the weight of lungs similar to that of no-intervention mice (normal) (B). Values are plotted as mean ± SEM (P < .01).
Inhibition of the formation and growth of lung metastases in mouse CT26 colon adenocarcinoma. Mice were immunized as described, and 5 × 105 CT26 cells were then injected into tail vein 1 week after the fourth immunization. The experiment was terminated after 18 days when control mice became moribund, and lungs were weighed and assessed for the presence of surface metastasis. qVEGFR vaccine can decrease the number of surface metastases (A) and abolish tumor burden by rendering the weight of lungs similar to that of no-intervention mice (normal) (B). Values are plotted as mean ± SEM (P < .01).
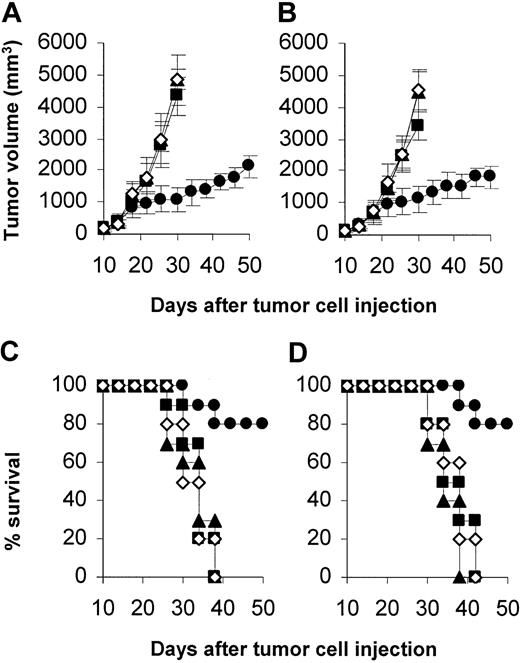
Furthermore, we found that treatment with qVEGFR resulted in significant antitumor activity against hematopoietic tumors, including MOPC-315 plasmacytoma in BALB/c mice and EL4 lymphoma in C57BL/6 (Figure 4).
Inhibition of the growth of hematopoietic tumors. Mice (10 mice/group) were treated with qVEGFR (•), mVEGFR (▪), ALUM (▴), or PBS alone (⋄) at day 7 after 5 × 105 MOPC-315 (A,C) or EL4 (B,D) were introduced subcutaneously into mice. Mice were treated as described in the legend to Figure 2. Treatment with qVEGFR resulted in the inhibition of tumor growth and longer life span. Error bars indicate SEM.
Inhibition of the growth of hematopoietic tumors. Mice (10 mice/group) were treated with qVEGFR (•), mVEGFR (▪), ALUM (▴), or PBS alone (⋄) at day 7 after 5 × 105 MOPC-315 (A,C) or EL4 (B,D) were introduced subcutaneously into mice. Mice were treated as described in the legend to Figure 2. Treatment with qVEGFR resulted in the inhibition of tumor growth and longer life span. Error bars indicate SEM.
Characterizations of autoantibodies
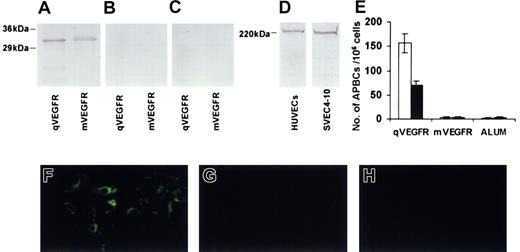
To explore the possible mechanism by which the antitumor activity was induced with qVEGFR, we identified autoantibodies against Flk-1 in the immunized mice. Sera from qVEGFR-immunized mice recognized not only recombinant protein qVEGFR, they also recognized recombinant protein mVEGFR in Western blot analysis (Figure 5A). In contrast, the sera isolated from controls showed negative staining (Figure 5B-C). Sera from mice immunized with qVEGFR recognized a single band in Flk-1–positive mouse SVEC4-10 endothelial cells and KDR-positive HUVECs (Figure 5D), with the same size as recognized by commercially available Flk-1 or KDR antibodies. Sera from qVEGFR-immunized mice also recognized recombinant protein qVEGFR and mVEGFR by ELISA. Immunoglobulin subclass response to VEGFRs was found to be elevated significantly in IgG1 and IgG2b.
Characterization of the autoantibodies. Recombinant qVEGFR and mVEGFR can be recognized by the sera isolated from mice immunized with qVEGFR (A) but negative staining from mice immunized with mVEGFR (B) or ALUM (C) in Western blot analysis. Sera from mice immunized with qVEGFR also recognized a single band in Flk-1–positive mouse SVEC4-10 endothelial cells and KDR-positive HUVECs (D). The number of anti-qVEGFR– (□) or anti-mVEGFR– (▪) producing B lymphocytes in spleens of mice immunized with qVEGFR, mVEGFR, or ALUM were counted in an ELISPOT assay (E). Mice were immunized once a week for 4 weeks, and mononuclear cells were prepared from spleens 1 week after the fourth immunization. Data presented are mean ± SEM. There was endothelial deposition of autoantibodies within tumor tissue from mice immunized with qVEGFR (F), but not from mice immunized with mVEGFR (G) or ALUM (H). Panels F-H were stained with immunofluorescence stain; original magnifications, × 200.
Characterization of the autoantibodies. Recombinant qVEGFR and mVEGFR can be recognized by the sera isolated from mice immunized with qVEGFR (A) but negative staining from mice immunized with mVEGFR (B) or ALUM (C) in Western blot analysis. Sera from mice immunized with qVEGFR also recognized a single band in Flk-1–positive mouse SVEC4-10 endothelial cells and KDR-positive HUVECs (D). The number of anti-qVEGFR– (□) or anti-mVEGFR– (▪) producing B lymphocytes in spleens of mice immunized with qVEGFR, mVEGFR, or ALUM were counted in an ELISPOT assay (E). Mice were immunized once a week for 4 weeks, and mononuclear cells were prepared from spleens 1 week after the fourth immunization. Data presented are mean ± SEM. There was endothelial deposition of autoantibodies within tumor tissue from mice immunized with qVEGFR (F), but not from mice immunized with mVEGFR (G) or ALUM (H). Panels F-H were stained with immunofluorescence stain; original magnifications, × 200.
Anti-VEGFR antibody-producing B cells (APBCs) were detected by ELISPOT. The number of anti-VEGFR antibody-producing B cells was elevated in the spleens of mice immunized with qVEGFR, compared with that in controls (Figure 5E).
To identify the possible deposition of autoantibodies within tumor tissues, we investigated the tissues by immunofluorescence staining. There was the endothelial deposition of IgG within tumor tissues from qVEGFR-immunized mice (Figure 5F), but not from controls (Figure 5G-H). In addition, no IgM- or IgA-specific fluorescence was found, nor was detectable deposition of autoantibodies found within the major organs, such as kidney, liver, spleen, and brain, in the immunized or control mice.
Treatment with purified immunoglobulins isolated from qVEGFR-immunized mice resulted in apparent inhibition of VEGF-mediated endothelial cell proliferation (Figure 6A), compared with those from controls. In addition, the immunoglobulins had no direct effect on the proliferation of CT26, LL/2, or Meth A tumor cells in vitro. Moreover, adoptive transfer of purified immunoglobulins isolated from qVEGFR-immunized mice provided effective protection against tumor growth (Figure 6B).
Inhibition of VEGF-mediated endothelial cell proliferation in vitro and the antitumor effect by the adoptive transfer of immunoglobulins in vivo. (A) HUVECs were incubated with human VEGF (200 ng/mL) in the presence of various concentrations of immunoglobulins. Treatment with immunoglobulins from mice immunized with qVEGFR (•) resulted in apparent inhibition of endothelial cell proliferation compared with those from mice immunized with mVEGFR (▪) or ALUM (▴) alone. However, it had no effect on basic fibroblast growth factor (bFGF)–mediated endothelial cell proliferation (data not shown). (B) Adoptive transfer of immunoglobulins in vivo. The protective antitumor effect against Meth A cells was tested with purified immunoglobulins (50 mg/kg) from mice immunized with qVEGFR (•), mVEGFR (▪), or ALUM (▴). Treatment with immunoglobulins isolated from qVEGFR mice showed apparent protective antitumor effect, compared with controls. Results are expressed as means ± SEMs.
Inhibition of VEGF-mediated endothelial cell proliferation in vitro and the antitumor effect by the adoptive transfer of immunoglobulins in vivo. (A) HUVECs were incubated with human VEGF (200 ng/mL) in the presence of various concentrations of immunoglobulins. Treatment with immunoglobulins from mice immunized with qVEGFR (•) resulted in apparent inhibition of endothelial cell proliferation compared with those from mice immunized with mVEGFR (▪) or ALUM (▴) alone. However, it had no effect on basic fibroblast growth factor (bFGF)–mediated endothelial cell proliferation (data not shown). (B) Adoptive transfer of immunoglobulins in vivo. The protective antitumor effect against Meth A cells was tested with purified immunoglobulins (50 mg/kg) from mice immunized with qVEGFR (•), mVEGFR (▪), or ALUM (▴). Treatment with immunoglobulins isolated from qVEGFR mice showed apparent protective antitumor effect, compared with controls. Results are expressed as means ± SEMs.
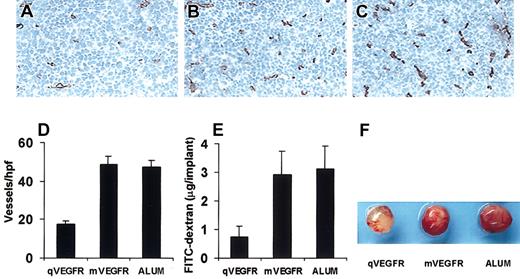
Inhibition of angiogenesis
Vaccination with qVEGFR resulted in the apparent inhibition of angiogenesis in tumors (Figure 7A) compared with controls (Figure 7B-C). Angiogenesis within tumor tissue was estimated counting the number of microvessels on the section staining with an antibody reactive to CD31 (Figure 7D). The inhibition of angiogenesis in immunized mice was confirmed in alginate encapsulation assay. Alginate implant angiogenesis was quantitated by measuring the uptake of FITC-dextran into beads. Vascularization of alginate beads was apparently reduced, and FITC-dextran uptake was decreased 75% to 77% in qVEGFR-immunized mice against that in controls (Figure 7E-F) (P < .01).
Inhibition of angiogenesis within tumor from qVEGFR-immunized mice was estimated by immunohistochemical analysis and alginate encapsulation assay. Sections of frozen LL/2 tumor tissues obtained from mice immunized with qVEGFR (A), mVEGFR (B), and ALUM (C). Vessel density was determined by counting the number of the microvessels per high-power field (D) in tumor sections stained with Peroxidase-DAB, an antibody reactive to CD31 (brown). Original magnification, × 200 (A-C) Alginate beads containing 1 × 105 Meth A cells were implanted subcutaneously into BALB/c mice on day 7 after the fourth immunization. Twelve days later, beads were surgically removed, and FITC-dextran was quantified as described in “Materials and methods.” FITC-dextran uptake (E) and photograph of alginate implants (F) showed the reduction of vascularization in implants of qVEGFR-immunized mice.
Inhibition of angiogenesis within tumor from qVEGFR-immunized mice was estimated by immunohistochemical analysis and alginate encapsulation assay. Sections of frozen LL/2 tumor tissues obtained from mice immunized with qVEGFR (A), mVEGFR (B), and ALUM (C). Vessel density was determined by counting the number of the microvessels per high-power field (D) in tumor sections stained with Peroxidase-DAB, an antibody reactive to CD31 (brown). Original magnification, × 200 (A-C) Alginate beads containing 1 × 105 Meth A cells were implanted subcutaneously into BALB/c mice on day 7 after the fourth immunization. Twelve days later, beads were surgically removed, and FITC-dextran was quantified as described in “Materials and methods.” FITC-dextran uptake (E) and photograph of alginate implants (F) showed the reduction of vascularization in implants of qVEGFR-immunized mice.
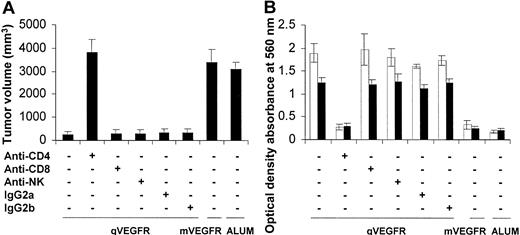
Function of T-cell subsets in antitumor activity
To explore the roles of immune cell subsets in antitumor activity elicited by qVEGFR, we depleted CD4+ or CD8+ T lymphocytes or NK cells through injection of the corresponding monoclonal antibodies. Mice depleted of CD4+ T lymphocytes and vaccinated with qVEGFR were not protected from tumor challenge. In contrast, treatment with mAb against CD8 or NK cells failed to abrogate the antitumor activity (Figure 8A). Furthermore, sera from mice depleted of CD4+ T lymphocytes and vaccinated with qVEGFR did not react with recombinant protein mVEGFR and qVEGFR in ELISA. In contrast, sera from mice depleted of CD8 or NK and vaccinated with qVEGFR had detectable antibodies against recombinant protein VEGFRs (Figure 8B).
Abrogation of antibodies' production and antitumor activity by the depletion of immune cell subsets. (A) Abrogation of antitumor activity by the depletion of immune cell subsets. Depletion of CD4 T lymphocytes showed complete abrogation of the antitumor activity of the qVEGFR vaccine (n = 10). In contrast, treatment with anti-CD8, anti-NK, or isotype controls (IgG2a and IgG2b) had no effect. Results showed the tumor volume on day 26 after tumor cell injection (mean ± SEM). (B) Abrogation of antibody production by the depletion of immune cell subsets. Sera obtained from mice immunized with qVEGFR were tested against qVEGFR (□) or mVEGFR (▪) by ELISA on day 7 after the fourth immunization. Treatment with anti-CD4 can abrogate the elevation of antibodies against qVEGFR and mVEGFR. In contrast, treatment with anti-CD8, anti-NK, or isotype control had no effect.
Abrogation of antibodies' production and antitumor activity by the depletion of immune cell subsets. (A) Abrogation of antitumor activity by the depletion of immune cell subsets. Depletion of CD4 T lymphocytes showed complete abrogation of the antitumor activity of the qVEGFR vaccine (n = 10). In contrast, treatment with anti-CD8, anti-NK, or isotype controls (IgG2a and IgG2b) had no effect. Results showed the tumor volume on day 26 after tumor cell injection (mean ± SEM). (B) Abrogation of antibody production by the depletion of immune cell subsets. Sera obtained from mice immunized with qVEGFR were tested against qVEGFR (□) or mVEGFR (▪) by ELISA on day 7 after the fourth immunization. Treatment with anti-CD4 can abrogate the elevation of antibodies against qVEGFR and mVEGFR. In contrast, treatment with anti-CD8, anti-NK, or isotype control had no effect.
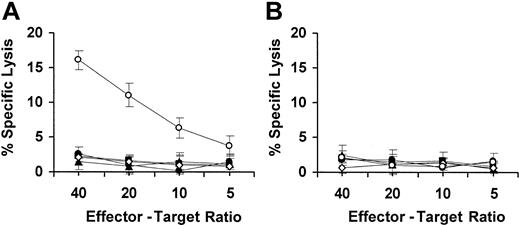
T cells isolated from mice immunized with qVEGFR, mVEGFR, ALUM alone, or nonimmunized mice did not show increased cytotoxicity against Flk-1–positive target cells (Figure 9A) or Flk-1–negative target cells (Figure 9B). As a positive control, we induced Flk-1–specific cytotoxicity against Flk-1–positive target cells with T-enriched cell fraction isolated from mice immunized with the dendritic cells transfected with adenovirus encoding Flk-1 (Figure 9A), but not against Flk-1–negative target cells (Figure 9B).
Representative experiment of CTL-mediated cytotoxicity in vitro. T cells derived from the spleens of qVEGFR-immunized mice were tested against Flk-1–transfected CT26 target cells (A) and nontransfected CT26 (B) at different effector-target ratios by a standard 4-hour 51Cr release assay, as described in “Materials and methods.” T cells isolated from mice immunized with qVEGFR (•) did not show increased cytotoxicity against Flk-1–positive target cells (A) and Flk-1–negative target cells (B) compared with control groups, including mVEGFR (▪), ALUM (▴), or nonimmunized (⋄) mice. As a positive control, T cells from mouse vaccinated with the dendritic cells transfected with adenovirus encoding Flk-1 (○) showed increased cytotoxicity against Flk-1–positive target cells (A) but not against Flk-1–negative target cells (B). Error bars indicate SD.
Representative experiment of CTL-mediated cytotoxicity in vitro. T cells derived from the spleens of qVEGFR-immunized mice were tested against Flk-1–transfected CT26 target cells (A) and nontransfected CT26 (B) at different effector-target ratios by a standard 4-hour 51Cr release assay, as described in “Materials and methods.” T cells isolated from mice immunized with qVEGFR (•) did not show increased cytotoxicity against Flk-1–positive target cells (A) and Flk-1–negative target cells (B) compared with control groups, including mVEGFR (▪), ALUM (▴), or nonimmunized (⋄) mice. As a positive control, T cells from mouse vaccinated with the dendritic cells transfected with adenovirus encoding Flk-1 (○) showed increased cytotoxicity against Flk-1–positive target cells (A) but not against Flk-1–negative target cells (B). Error bars indicate SD.
Observation of potential toxicity
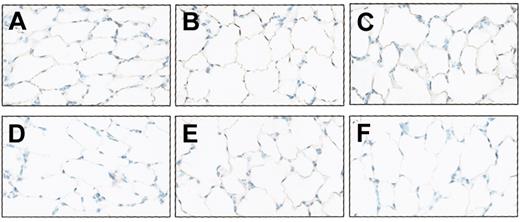
Vaccinated animals without tumor were particularly investigated for potential toxicity for more than 10 months. No adverse consequences were indicated in gross measures such as weight loss, ruffling of fur, life span, behavior, or feeding. No pathologic changes of liver, lung, kidney, spleen, brain, heart, or bone marrow were found by microscopic examination. Furthermore, no increased active caspase-3 or apoptosis was found in the lungs of vaccinated mice by immunostaining for active caspase-3 and by TUNEL staining (Figure 10). In addition, immunized mice did not have alveolar enlargement compared with control groups (Figure 10).
No apoptotic activity in the lungs of the immunized mice by the immunostaining for active caspase-3 and by TUNEL staining. Mice without tumor were immunized, and active caspase-3 was determined by staining the section of the lungs with an antibody reactive to mouse active caspase-3 (A-C), as described in “Materials and methods.” Apoptotic cells in the lungs of the mice were also estimated with TUNEL assay (D-F). No apoptotic activity was found by immunostaining active caspase-3 or by TUNEL staining. (A,D) Immunization with qVEGFR. (B,E) Immunization with mVEGFR. (C,F) Nonimmunization. In addition, qVEGFR-immunized mice (A,D) did not show the alveolar enlargement compared with control groups. Original magnification is ×200 for all panels.
No apoptotic activity in the lungs of the immunized mice by the immunostaining for active caspase-3 and by TUNEL staining. Mice without tumor were immunized, and active caspase-3 was determined by staining the section of the lungs with an antibody reactive to mouse active caspase-3 (A-C), as described in “Materials and methods.” Apoptotic cells in the lungs of the mice were also estimated with TUNEL assay (D-F). No apoptotic activity was found by immunostaining active caspase-3 or by TUNEL staining. (A,D) Immunization with qVEGFR. (B,E) Immunization with mVEGFR. (C,F) Nonimmunization. In addition, qVEGFR-immunized mice (A,D) did not show the alveolar enlargement compared with control groups. Original magnification is ×200 for all panels.
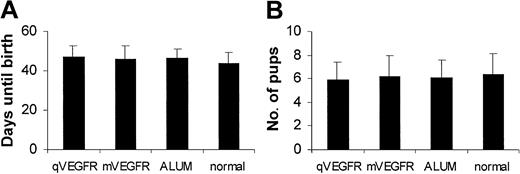
Female mice were immunized once a week for 4 continuous weeks with different doses of protein vaccine and were mated with nonimmunized male mice 2 weeks after the final immunization. All females of each experimental group gave birth. Moreover, the vaccination of qVEGFR did not show the impact on the average time from the start of cohabitation to parturition and number of pups compared with control groups (P > .05) (Figure 11).
Effect of the vaccination on fertility. Female mice (10 mice/group) were immunized and were allowed to cohabitate with males. Days until parturition (A) and number of pups (B) were recorded. Vaccination with qVEGFR did not show the impact on the average time from start of cohabitation to parturition and the number of pups compared with the control groups. Results are presented as mean ± SEM.
Effect of the vaccination on fertility. Female mice (10 mice/group) were immunized and were allowed to cohabitate with males. Days until parturition (A) and number of pups (B) were recorded. Vaccination with qVEGFR did not show the impact on the average time from start of cohabitation to parturition and the number of pups compared with the control groups. Results are presented as mean ± SEM.
Neuromuscular performance as determined by the wire test and the footprint test did not reveal any impairment in mice immunized with qVEGFR compared with controls (data not shown). For evaluation of the effects of qVEGFR on hematopoiesis, animals were investigated for more than 10 months and were subjected to complete peripheral blood counts and differentials. In addition, bone marrow cells were examined and enumerated. No decreased or compensating hematopoiesis was found (data not shown).
Discussion
Among the many different immunotherapeutic strategies currently evaluated, active specific immunotherapies with cancer vaccines based on tumor antigens represent promising approaches for cancer therapy.40,41 However, to date, with the few exceptions of melanoma antigen, there is limited information on the identity and density of antigenic peptides and cytotoxic T-lymphocyte (CTL) epitopes presented by human solid tumors. In addition, most of the identified tumor antigens are self-molecules.40,41 As expected, the reaction of the host toward these self-molecules may show immune tolerance to them if the host is immunized by vaccines based on these self-molecules. Efforts are ongoing to develop new strategy for cancer vaccines.
Several observations were made in the present study concerning a vaccine based on quail homologous VEGFR-2 as a model antigen, antitumor immunity, and angiogenesis. The protein vaccine qVEGFR could induce both protective and therapeutic antitumor immunity. Autoimmune response against Flk-1 may be provoked in a cross-reaction by the immunization with qVEGFR vaccine, and the autoantibody targeting of Flk-1 is probably responsible for the antitumor activity. Autoantibodies against Flk-1 were identified by Western blot analysis and ELISA. IgG1 and IgG2b were substantially increased in response to qVEGFR. Anti-VEGFR antibody-producing B cells were detectable by ELISPOT. There was endothelial deposition of immunoglobulins in tumor. Endothelial cell proliferation was inhibited in vitro by immunoglobulins from qVEGFR-immunized mice. Antitumor activity resulted from the adoptive transfer of the purified immunoglobulins. Antitumor activity and production of autoantibodies against Flk-1 could be abrogated by the depletion of CD4+ T lymphocytes. Angiogenesis was apparently inhibited within the tumors, and the vascularization of alginate beads was also reduced. Based on the findings mentioned, we may rule out the possibility that the antitumor activity with quail homologous VEGFR-2 may result from a nonspecifically augmented immune response against tumor growth in host mice.
Angiogenesis is a complex process involving many molecules and cellular biologic events. The importance of KDR/Flk-1 in tumor angiogenesis is exemplified in studies using neutralizing KDR/Flk-1 mAb,15 a dominant-negative Flk-1 receptor,42 or KDR/Flk-1 kinase inhibitors,16,17 all of which were shown to inhibit angiogenesis and tumor growth. It has been recently reported that peripheral T-cell tolerance against the murine VEGFR-2 (Flk-1) can be broken by an oral DNA vaccine encoding autologous Flk-1, delivered by an attenuated strain of Salmonella typhimurium.33 This vaccine was found to be effective in mouse tumor models of non-small cell lung carcinoma, colon carcinoma, and melanoma. Involvement of cytotoxic T cells in its antitumor activity was suggested by marked up-regulation of T-cell activation markers CD2, CD25, and CD69 on CD8+ T cells when coincubated with cells expressing Flk-1. In vitro cytotoxicity occurred only against target cells transduced to express Flk-1; furthermore, the effect of the vaccine was severely impaired in mice depleted in vivo of CD8+ T cells throughout the effector phase. Depletion of CD4+ cells was without effect. Thus, the antitumor activity of this DNA vaccine may result from the induction of CTL-mediated killing of endothelial cells.33 However, our approach is different in several ways compared with the report mentioned. First, our vaccine is based on the recombinant protein of quail VEGFR-2 (Quek-1, a xenogeneic homologue of Flk-1) with ALUM used as an adjuvant, but not on mice Flk-1 DNA vaccine with attenuated S typhimurium as an antigen carrier. Second, autoimmune response against Flk-1 may be provoked in a cross-reaction by the immunization with qVEGFR vaccine, and the autoantibody, not CTL targeting of Flk-1, is probably responsible for the antitumor activity. Third, the antitumor activity could be CD4+ T lymphocyte dependent but not CD8+ T lymphocyte dependent. The importance of CD4+ versus CD8+ T-cell immunity in these studies might have been determined by the use of different target antigens, adjuvants, and routes of immunization. It is known that CD4+ T lymphocytes can steer and amplify immune responses through the secretion of cytokines and the expression of surface molecules.43,44 For antibody-dependent immunity, CD4+ T lymphocytes can be required at the immunization phase and at the effector phase.45,46 Furthermore, CD4+ T lymphocytes have been reported to be required for the induction of antitumor immunity by vaccination with a recombinant vaccinia virus encoding self-tyrosinase–related protein 1 (TRP-1) in a mouse melanoma model.47 In addition, it has been reported that CD4+ T lymphocytes play a prominent role in classic mouse models of autoimmunity, such as experimental autoimmune encephalitis, systemic lupus erythematosus, and autoimmune gastritis.48-51 Taken together, these findings may help explain the requirement for CD4+ T lymphocytes in the induction of an autoimmune response against mouse VEGFR-2 in a cross-reaction in the present study.
We have paid special attention to investigating potential toxicity in the mice immunized and have not found marked adverse effects of qVEGFR vaccine in the present study. It has been reported that rats treated with the VEGF receptor blocker SU5416, a synthetic low-molecular–weight inhibitor of tyrosine kinase receptors, showed increased alveolar enlargement, alveolar septal cell apoptosis.36 We also examined whether the lungs of mice treated with qVEGFR showed increased apoptotic activity by active caspase-3 staining. We found that there was no increase in apoptotic activity by active caspase-3 staining. In addition, we did not find increased numbers of apoptotic cells in the lungs of mice treated with qVEGFR with TUNEL assay. Thus, the lack of toxicity in lung in the present study suggests that a different sensitivity of the lung cells may result from the use of the different blockers of VEGF receptor pathways. This suggestion was also supported by other findings.15,52 It has been reported that anti–Flk-1 mAb treatment was well tolerated in mice, no signs of antibody toxicity were observed, and no organ abnormalities were seen at autopsy. Histologic examination findings, including of the lung, also appeared normal in the anti–Flk-1 mAb-treated mice.15,52
Although it has been reported that angiogenesis is important in female reproductive function and fetal development,6,53-56 we found that the fertility of the mice immunized with qVEGFR remained unimpaired. In accordance with our observations, some recent studies demonstrate that treatment of experimental animals with an oral DNA vaccine encoding autologous Flk-1 or by administration of a VEGF-neutralizing antibody revealed no impact on fertility based on the pregnancy rate, the time elapsed from start of cohabitation until parturition, and the number of pups born.33,57 We also found that hematopoiesis and neuromuscular performance was not affected in the immunized mice. This result is compatible with the report that treatment with the inhibitor of vascular endothelial growth factor receptor tyrosine kinases or with an oral DNA vaccine encoding autologous Flk-1 had no significant effect on hematopoiesis and neuromuscular performance.16,33 In addition, it has been reported that Flk-1 is expressed in normal vascular endothelium at lower levels than in tumor vasculature.13,58 Thus, based on the findings mentioned, we may speculate that the sensitivity of the vascular endothelium in physiological processes such as pregnancy may be different from that in malignant tumor to the inhibition of angiogenesis by qVEGFR.
In the present study, a quail homologous VEGFR-2 protein vaccine (qVEGFR), based on quail VEGFR-2 as antigen, could induce not only protective but also therapeutic antitumor activity in several tumor models in mice without apparent adverse effects. In addition, sequence comparison analysis, through a search of the SwissProt database in the present study, indicated that the primary sequence of quail VEGFR-2 (Quek-1) at the amino acid level is 67% and 70% identical with mouse homologue (Flk-1) and human (KDR). Furthermore, the antibodies induced with qVEGFR recognized not only mouse VEGFR-2 but also human VEGFR-2. Human endothelial cell proliferation was also inhibited in vitro by immunoglobulins from qVEGFR-immunized mice. In addition, ALUM used as an adjuvant in the present study is the adjuvant approved by the Food and Drug Administration for use in human vaccines. Our findings suggest that qVEGFR vaccine may have potential application to the treatment of cancer patients. To explore this possibility, we are conducting a variety of preclinical studies to apply for clinical trials for the treatment of patients with advanced cancer.
Taken together, our findings may provide a vaccine strategy for cancer therapy through the induction of an autoimmune response against the self-molecules involved in tumor growth in a cross-reaction by immunization with the single xenogeneic homologous VEGFR-2. This vaccine strategy may be used in targeting other growth factors or their receptors associated with tumor growth. This suggestion is also supported by our unpublished data (October 2002) that a vaccine based on fibroblast growth factor (FGF) receptor or integrin αv, isolated from quail, can induce an antitumor effect through autoimmunity elicited against tumor endothelium in mouse and that a vaccine based on EGF-receptor from the fruit fly D melanogaster or from birds can induce autoimmunity against EGFR-positive tumors in mouse models. Thus, the breaking of immune tolerance to self-molecules involving angiogenesis with xenogeneic counterparts may be of importance for the further exploration of the applications of xenogeneic homologous genes identified in human and other animal genome sequence projects in cancer therapy.
Prepublished online as Blood First Edition Paper, May 15, 2003; DOI 10.1182/blood-2002-12-3772.
Supported by Special Project of National Key Basic Research Program of China (No. 2001-50) and National Key Basic Research Program of China (2001CB510001 and G1998051214), Project of National Natural Sciences Foundation of China, National 863 projects. The publication fees of this article were paid for by the Chinese Medical Board Foundation.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal