IMMUNOBIOLOGY
Approximately 14 years ago, CD4+CD25+ regulatory T (T-reg) cells were first identified as playing an important role in the maintenance of allograft immune tolerance.1 Since that initial report, several more investigators have confirmed their role in a variety of allograft settings, including both solid organ and hematopoietic stem cell transplantation.2 In vitro, activation of CD4+CD25+ T-reg cells was shown to be antigen specific, but, once activated, the cells were antigen nonspecific in their ability to suppress T-cell reactivity.3 These data suggested that activation of CD4+CD25+ T-reg cells in vitro might induce systemic immune suppression upon adoptive transfer. However, numerous studies where CD4+CD25+ T-reg cells have been activated in vitro and then adoptively transferred in vivo have indicated that the cells do not induce systemic immune suppression. Animal data has shown that when CD4+CD25+ T-reg cells are activated in vitro with alloantigens, the cells can facilitate allograft tolerance in an antigen-specific manner, but these experiments were done in systems where graft tolerance and rejection against different alloantigens were not examined simultaneously. So, there has been no definitive data to show that CD4+CD25+ cells are truly antigen specific with regard to their effector function in vivo.
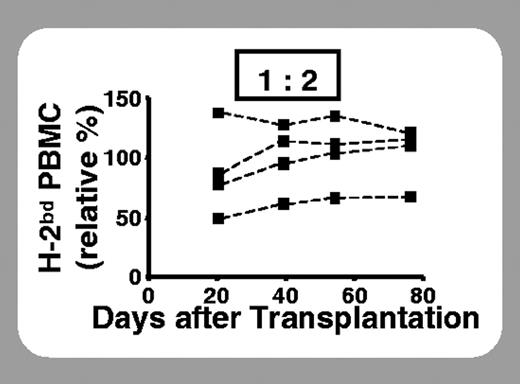
Using a mouse bone marrow graft rejection model, Joffre and colleagues (page 4216) demonstrate that recipient CD4+CD25+ cells can prevent hematopoietic stem cell graft rejection in an antigen-specific manner, confirming work by others in solid organ transplantation models.2 However, these studies go further to examine antigen specificity of the adoptively transferred T-reg cells in a novel graft rejection model. Freshly isolated CD4+CD25+ cells were incapable of preventing rejection, but when the cells were precultured in vitro with donor antigen-presenting cells, they were able to effectively prevent rejection mediated by CD4+, CD8+, or total T cells. Using an innovative model, in which lethally irradiated recipient mice were coinfused with donor, recipient, and third-party bone marrow, they were able to demonstrate that antigen-specific protection of donor engraftment by T-reg cells and rejection of third-party bone marrow could occur simultaneously. Their results clearly show that effector function of ex vivo–alloactivated CD4+CD25+ T-reg cells can be antigen specific in vivo. These results are remarkable, but several questions arise from these observations. While antigen specificity was observed at lower CD4+CD25+-to–effector T-cell ratios, why was prevention of graft rejection less specific when higher numbers of T-reg cells were administered? What is the mechanism(s) of antigen-specific suppression? Does the administration of alloantigen-activated CD4+CD25+ cells have any impact on clearance of a viral or bacterial infection? How do the adoptively transferred alloactivated CD4+CD25+ cells migrate and localize in vivo? And, is there truly an advantage to giving alloactivated CD4+CD25+ T-reg cells rather than polyclonally activated cells? Future studies using this model may answer some of these questions. If alloactivated CD4+CD25+ T-reg cells could be used clinically for establishing donor allograft tolerance with less need for nonspecific immunosuppressive drugs, this could have a major impact on clinical outcome after hematopoietic stem cell or solid organ transplantation.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal