NEOPLASIA
Research on Kaposi sarcoma (KS) was given a shot in the arm with the discovery in 1994 of Kaposi sarcoma-associated herpesvirus (KSHV), also known as human herpesvirus-8 (HHV-8).1 This virus is an etiological agent for KS and also for primary effusion lymphoma (PEL), multicentric Castleman disease (MCD), and possibly pulmonary hypertension. Like other herpesviruses, KSHV encodes for several unique genes that have their origin in the host genome. Some, including viral interleukin 6 (vIL-6), viral macrophage inflammatory protein-1 (vMIP-1), vMIP-2, and vMIP-3, have direct proangiogenic activity and contribute to KS pathogenesis.2 vIL-6 is also responsible for much of the symptomatology of MCD and acts as an autocrine growth factor for PEL cells. Other KSHV genes act indirectly by influencing host genes or pathways. In particular, a constitutively active viral G protein-coupled receptor (ORF74) can act indirectly to promote angiogenesis by inducing vascular endothelial growth factor (VEGF) production. This occurs at least in part through enhancement of the activity of hypoxia inducible factor (HIF).3
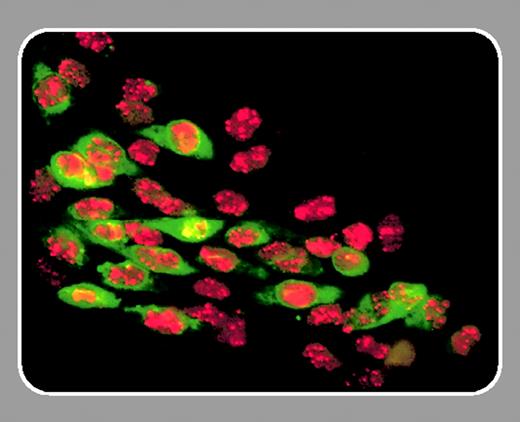
In this issue, McAllister and colleagues (page 3465) define a novel mechanism by which KSHV can induce growth of endothelial cells: by increasing the activity of heme oxygenase-1 (HO-1). The authors found the enhanced expression of this protein by comparing the protein expression profiles of KSHV-infected and uninfected endothelial cells. HO-1 is responsible for the physiologic breakdown of heme into carbon monoxide, iron, and biliverdin (which is then converted to bilirubin). In normal cells, HO-1 is induced by heme. It can also be up-regulated by hypoxia and HIF. In tissues affected by injury and bleeding, HO-1 helps improve vascular flow through the production of carbon monoxide; provides protection against free heme, a prooxidant, by producing biliverdin, an antioxidant; mediates antiapoptotic effects; and has anti-inflammatory activities. HO-1 also up-regulates a number of angiogenic growth factors including VEGF, 4 and, as shown in this paper, can enhance the proliferation of KSHV-infected dermal microvascular endothelial cells (DMVECs). Its induction by KSHV thus provides a new mechanism by which the virus can promote angiogenesis and the growth of infected endothelial cells. There is substantial blood extravasation in KS tissues (blood gives KS its characteristic color), and HO-1 induction also protects KSHV-infected cells against heme toxicity. Its importance in KS pathogenesis was underscored by the finding in the current paper that HO-1 mRNA and protein are highly expressed in KS lesions. These findings might, with further study, lead to new therapeutic avenues for treating KS with specific HO inhibitors that are already being used experimentally for the treatment of hyperbilirubinia.
The ability to promote angiogenesis through multiple pathways is one of the most distinctive features of KSHV. Very few KSHV-infected patients develop KS (outside a setting of HIV coinfection or other immunosuppression), and KS can probably best be viewed as a biologic accident resulting in part from the production of proangiogenic factors by KSHV-infected cells. But what forces have led KSHV to adopt the strategy of inducing angiogenesis? Endothelial cells are important targets for KSHV infection, and production of angiogenic factors may promote KSHV infection of and replication in these cells. The recent finding that KSHV lytic replication is up-regulated by hypoxia and HIF5 suggests that the virus may be particularly well poised to replicate in wounds (where it may find a portal of entry). The vascular compromise, heme deposition, and hypoxia at the edge of wounds lead to HO-1 expression, HIF activation, and angiogenesis with endothelial cell growth. This would appear to provide a fertile environment for KSHV infection. KSHV-induced activation of HO-1 and production of proangiogenic factors may then further optimize the environment for KSHV spread. This scenario is best viewed as a working hypothesis, and there is still much we do not know about the transmission and life cycle of KSHV in its human host. It will be interesting to further define the strategies this virus has developed in occupying its particular ecologic niche. This will not only advance our understanding of KSHV-induced diseases, but also provide a foundation on which to develop effective pathogenesis-based therapies.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal