Monitoring of Epstein-Barr virus DNA by quantitative real-time polymerase chain reaction may serve as an accurate surrogate marker of tumor load in patients with Hodgkin and non-Hodgkin lymphoma that were demonstrated to be EBV-positive.
Epstein Barr virus (EBV) is a widespread human herpesvirus that establishes lifelong asymptomatic infection of B cells. In 1997, EBV was classified by the World Health Organization–International Agency for Research on Cancer (WHO-IARC) as a group I human carcinogen because of its etiologic role in nasopharyngeal carcinoma and lymphomagenesis. EBV is associated with endemic Burkitt lymphoma, posttransplantation lymphoproliferative disease (PTLD), some T-cell and natural killer (NK) cell lymphomas, and Hodgkin disease. While the exact role of EBV in the pathogenesis of each type of lymphoma still needs to be elucidated,1 epidemiologic studies have shown strong associations between infectious mononucleosis and EBV-positive Hodgkin disease2 and also between posttransplantation EBV reactivation and the development of PTLD.3 Molecular monitoring of EBV DNA levels in patients with PTLD has been shown to accurately and sensitively reflect disease activity and is currently used to tailor treatment for the individual patient. Although viral infection is a presumed source of EBV DNA in patients with PTLD, release of EBV fragments from tumor cells, instead of fully assembled viral particles, is likely to play a major role in established PTLD.FIG1
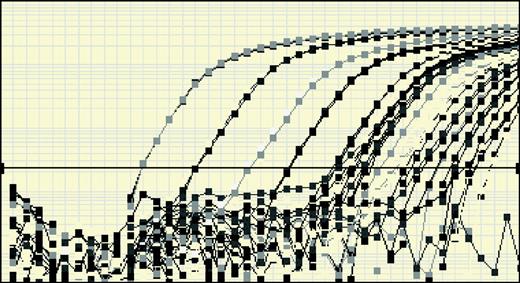
Standard curves for quantification of EBV DNA. See the complete figure in the article beginning on page 243.
Standard curves for quantification of EBV DNA. See the complete figure in the article beginning on page 243.
The hypothesis that release of EBV DNA fragments from EBV-positive lymphomas might be a general phenomenon and might be used as a surrogate marker of disease activity was the starting point for the study of Au and colleagues reported in this issue of Blood (page 243). The authors show that molecular monitoring of EBV DNA by quantitative real-time polymerase chain reaction (PCR) closely mirrors the clinical picture of the individual patient with an EBV-positive lymphoma. In addition, patients with a high EBV DNA copy number before the start of treatment showed inferior outcome. The prognostic significance of quantified EBV DNA seemed independent from the type of lymphoma, but was especially evident in patients with NK cell lymphoma. These results compare well to earlier findings in patients with PTLD and suggest that patients with non-Hodgkin lymphoma as well as patients with Hodgkin disease should be evaluated for the presence of EBV at diagnosis and during follow-up if EBV positivity has been demonstrated. Such diagnostic evaluation may include in situ hybridization for EBV-encoded RNA (EBER) on histopathologic examination and the quantification of EBV DNA in plasma by PCR.
Au et al used a very sensitive real-time PCR and reported relatively high values of EBV DNA in the NK cell lymphoma and PTLD group. The copy numbers reported exceed those reported in PTLD by a number of other investigators. The different quantified levels of EBV DNA hamper the comparison and combined analysis of several studies. It strongly supports efforts aimed at standardization of recently used real-time technology, such as has been initiated by the Quality Control for Molecular Diagnostics (QCMD, www.qcmd.org). Furthermore, the data presented by Au et al emphasize the importance of studies aiming to elucidate the exact pathogenetic role of EBV in lymphomagenesis, as such studies may yield new targets for therapy in poor-risk EBV-positive lymphoma. So far, the interplay between the EBV gene program, type and developmental stage of infected lymphocyte, and putative additional oncogenic event has remained an open but intriguing question in most EBV-positive lymphomas.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal