Abstract
Multiple myeloma (MM) remains as an incurable disease although new therapies can achieve a high rate of complete remissions (CR). Unfortunately, most patients ultimately relapse due to the persistence of minimal residual disease (MRD), and only a minority could be cured. Detection and quantification of these cells is an important tool for monitoring these patients and predicting a potential relapse. Here we analyze by RQ-PCR the MRD in MM patients achieving CR in order to classify them into different risk categories.
MATERIAL AND METHODS: 38 MM patients uniformly treated according to the GEM-2000 (Spanish group for Myeloma) protocol, and that have achieved CR following PBSCT were included in the study. 22 were IgG, 9 IgA, 6 B-J and 1 non-secretory (κ/λ 21/16). 27 were male & 11 female with a median age of 58 (range 48–65). Bone marrow samples obtained at diagnosis and 3 months after transplant were analyzed. Complete (VDJH) and incomplete (DJH) Ig rearrangements were amplified with the Biomed-2 strategy (
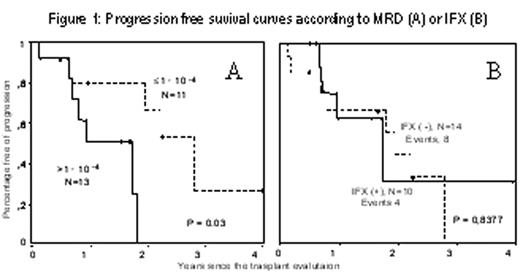
RESULTS: In 14 out of the cases included in the study, MRD investigation was not possible because the N-region was not longer enough to design the ASO primer (n=3), poor quality in the diagnostic sample to obtain the standard curve (n=8) or low plasma cell infiltration at diagnosis to obtain correct dilutions (n=3). The remaining 24 patients were classified into different risk groups according to the MRD level obtained 3 months after transplantation with a cut-off point of 0.01% tumor cells. Thus, progression free survival (PFS) was longer in those patients with MRD< 10−4 (p=0.03, figure 1A). By contrast, upon comparing the impact on PFS of immofixation (IFX) in these 24 patients that were in CR (defined by conventional electrophoresis criteria), it was observed that patients with IFX (−) didn’t showed a different outcome from those IFX (+) (figure 1B).
CONCLUSION: In summary, although RQ-PCR is a labor and time-consuming technique, it is an useful tool for monitoring MRD in MM. The level of 10−4 can contribute to classify patients into 2 groups (high and low MRD) with different risk of relapse that can be used to design specific therapies.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal